Interventional Neurology: Tackling the Number One Cause of Disability
Learn how Interventional Neurology techniques are used to treat acute stroke, the leading cause of adult disability. Understand procedures like mechanical thrombectomy and their role in improving patient outcomes.

Written by Dr. Mohammed Kamran
Reviewed by Dr. Dhankecha Mayank Dineshbhai MBBS
Last updated on 24th Oct, 2025

Introduction
Stroke is a medical emergency—and one of the number one causes of serious long-term disability worldwide. The good news is that interventional techniques now allow specialists to physically remove clots, seal bleeding vessels, and prevent future strokes with minimally invasive procedures. In this guide for the general public, you’ll learn what interventional neurology is, how it saves brain cells when time matters most, and the steps you can take today to lower your risk. We’ll break down symptoms you must never ignore, what happens in the hospital, and what to expect from treatments like mechanical thrombectomy. You’ll also get practical tips on prevention, rehab, and choosing the right hospital before an emergency strikes. Throughout, we’ll weave in real-world data, expert guidance, and easy-to-understand explanations so you can take action with confidence.
SERP Snapshot and Content Gap Analysis (What Top Pages Cover)
We reviewed high-authority, top-ranking pages you’re likely to find when searching for stroke and interventional care. Common strengths include clear symptom checklists and overviews of treatments. Gaps often include practical “what to do right now,” what to ask hospitals ahead of time, and the latest advances beyond the emergency room.
What Is Interventional Neurology?
Interventional neurology (often called interventional neuroradiology or endovascular neurosurgery) is a specialty that treats blood vessel problems in the brain and spine using tiny tubes (catheters) threaded through arteries—often starting from the wrist or groin. Instead of open brain surgery, doctors use live X-ray imaging to navigate to the problem area and deploy tools such as stent retrievers, aspiration catheters, coils, and flow-diverting stents.
Why this matters: Because stroke is a leading cause of serious long-term disability, the ability to restore blood flow quickly—or stop bleeding—can mean the difference between walking and wheelchair, speaking and silence, independence and lifelong care.
How Does It Differ from Neurology and Neurosurgery?
Neurology focuses on diagnosis and medical management (e.g., stroke units, medications).
Neurosurgery performs open operations (e.g., clipping aneurysms, decompressive craniectomy).
Interventional neurology works from inside the blood vessels, offering minimally invasive options for clots (ischemic stroke), aneurysms (ballooning arteries), arteriovenous malformations (AVMs), and carotid narrowing.
Common Procedures and When They’re Used?
Mechanical thrombectomy: Removing a clot causing a large-vessel ischemic stroke.
Intra-arterial thrombolysis: Directly delivering clot-busting medication at the blockage.
Aneurysm coiling and flow diversion: Preventing or treating bleeding from aneurysms.
Carotid artery stenting: Widening a narrowed neck artery to prevent future strokes.
Intracranial angioplasty/stenting: For select, high-risk narrowings within the brain’s arteries.
Related terms to note: interventional neuroradiology stroke treatment; ischemic vs hemorrhagic stroke explained.
Consult a Top Neurologist for Personalised Advice
Stroke and Disability: Why It’s the Number One Cause?
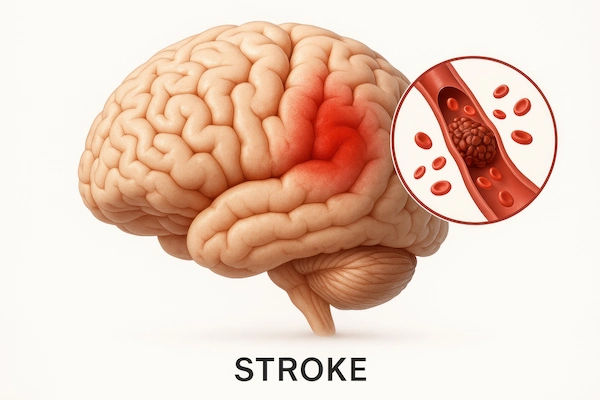
Stroke occurs when part of the brain is deprived of blood flow (ischemic stroke) or bleeding damages brain tissue (hemorrhagic stroke). The brain is extremely sensitive to oxygen deprivation—millions of neurons can die each minute a major artery is blocked. That’s why stroke is widely recognized as a leading cause of serious long-term disability in adults. In the United States, someone has a stroke about every 40 seconds; worldwide, stroke is a top cause of death and disability-adjusted life years lost .
Global and Local Statistics
- Globally, stroke remains among the top two causes of death and a major cause of disability .
In the U.S., stroke is a leading cause of serious long-term disability, impacting mobility, speech, cognition, and independence . - Risk increases with age but strokes also strike younger adults; about 10–15% occur in people under 50, depending on region and risk profiles.
Why Stroke Leaves Lasting Disability?
- Brain “real estate” matters: If the clot or bleed affects areas that control language, vision, or movement, disability can be profound.
- Time to treatment: Delays reduce the benefit of clot-busting drugs or thrombectomy.
- Collateral circulation: People with better backup vessels sometimes fare better.
- Rehab intensity and timing: Early, focused rehabilitation is a key predictor of recovery.
Unique insight: Disability risk isn’t just biology—it’s logistics. Communities with rapid EMS response, nearby thrombectomy-capable centers, and strong rehab systems consistently achieve better outcomes, underscoring the importance of emergency systems of care .
Spotting Stroke Fast: Symptoms and First Steps
When it comes to strokes, minutes matter. If you suspect a stroke, call emergency services immediately—don’t drive yourself. Early activation ensures rapid transport to the right hospital and primes the interventional team if needed.
BE FAST: The Checklist That Saves Brain Cells
- B – Balance: Sudden loss of balance or coordination
- E – Eyes: Sudden vision trouble in one or both eyes
- F – Face: Facial drooping on one side
- A – Arms: Arm (or leg) weakness or numbness
- S – Speech: Slurred speech, trouble speaking or understanding
- T – Time: Call emergency now; note when symptoms started
Additions: Severe headache (especially with bleeding), sudden confusion, dizziness, or one-sided neglect warrant urgent attention. When in doubt, treat it as a stroke.
When in Doubt, Call Emergency—Don’t Drive Yourself?
Why calling matters:
- EMS notifies the hospital (“stroke alert”) so CT/CTA imaging and the interventional team are ready.
- Paramedics take you to the nearest appropriate facility—often a thrombectomy-capable or comprehensive stroke center.
If you or a family member recently had brief, stroke-like symptoms (a transient ischemic attack, or TIA), seek urgent evaluation the same day. If symptoms persist or recur, consult a doctor online with Apollo 24|7 for rapid triage and guidance, and to go to the nearest emergency department.
Acute Treatments: From tPA to Mechanical Thrombectomy
Intravenous Thrombolysis (tPA and Tenecteplase)
- IV thrombolysis breaks up clots in certain ischemic strokes. Alteplase (tPA) is typically given within 4.5 hours of symptom onset in eligible patients .
- Tenecteplase, a single-bolus alternative, is used in some centers and trials; guidance varies by region.
- Not everyone qualifies (e.g., recent major surgery, high bleeding risk). Rapid CT scans rule out bleeding before treatment.
Mechanical Thrombectomy—Evidence and Eligibility
- For large-vessel occlusions (LVOs) in arteries like the internal carotid or proximal middle cerebral artery, mechanical thrombectomy physically removes the clot using stent retrievers and/or aspiration catheters.
- Landmark trials and pooled analyses show thrombectomy dramatically improves the chance of functional independence at 90 days, especially when performed quickly .
- Extended windows: DAWN and DEFUSE 3 trials showed that, with favorable imaging, benefits can extend up to 16–24 hours from last known well .
Time Windows, Imaging, and Real-World Examples
- Typical windows: Up to 6 hours for many LVOs; up to 16–24 hours in select patients based on CT/MRI perfusion imaging .
- Example: In DAWN, 49% of thrombectomy patients were functionally independent at 90 days vs 13% with medical therapy alone . In DEFUSE 3, it was 45% vs 17% .
- Symptomatic bleeding risks remain relatively low compared with the benefits in appropriately selected patients, but individual risk varies .
- Related terms: mechanical thrombectomy for large vessel occlusion; stroke treatment time window tPA 4.5 hours.
Inside an Interventional Suite: What to Expect?
Step-by-Step: Accessing the Brain’s Arteries
- Arrival and imaging: You’ll get rapid CT and vessel imaging to confirm the blockage and assess salvageable brain tissue.
- Anesthesia: Many centers use conscious sedation; some scenarios require general anesthesia.
- Access: A small tube is placed into an artery at the wrist (radial) or groin (femoral). Under X-ray, catheters are navigated into the blocked brain artery.
- Clot removal: A stent retriever may be deployed to ensnare the clot, or a large-bore catheter may directly suction it out. Often, both are used.
- Reperfusion grading: The team assesses how fully blood flow is restored (e.g., using the TICI scale).
- Aftercare: Patients typically go to an ICU or stroke unit for close neurologic monitoring.
Risks, Benefits, and Recovery Timeline
- Benefits: When done quickly in the right patients, thrombectomy significantly boosts chances of independent living.
- Risks: Vessel injury, bleeding, groin or wrist complications, contrast reactions, and, rarely, new stroke.
- Recovery: Some patients improve immediately; others recover steadily over days to weeks.
- Rehabilitation begins early to maximize brain plasticity. Expect continued improvement for months.
- Unique insight: Ask your hospital about their “door-to-groin puncture” and “door-to-reperfusion” times. Centers that track and publish these metrics usually have mature processes that improve outcomes.
Beyond Clots: Hemorrhagic Stroke and Structural Causes
Aneurysm Coiling and Flow Diverters
- Aneurysms are weak, bulging spots in arteries. If ruptured, they cause subarachnoid hemorrhage, a life-threatening emergency.
- Coiling: Soft platinum coils pack the aneurysm to prevent blood flow inside it.
- Flow diverters: Specialized stents redirect blood along the parent artery, promoting aneurysm healing over time.
- Decision-making depends on aneurysm size, shape, and location and may involve both interventionalists and neurosurgeons.
Carotid Artery Stenting and Intracranial Angioplasty
- Carotid stenosis (narrowing in the neck) can cause strokes by reducing flow or launching clots to the brain.
- Carotid stenting is a minimally invasive alternative to surgery (carotid endarterectomy) in selected patients; decision depends on plaque features, anatomy, and surgical risk .
Intracranial angioplasty/stenting may be considered for highly selected cases of severe, recurrent narrowing despite best medical therapy; careful risk–benefit assessment is essential.
AVM Embolization and Other Emergencies
- AVMs (artery-vein tangles) can bleed; embolization uses liquid agents (glues, Onyx) to block abnormal vessels, sometimes as a stand-alone therapy or as a bridge to surgery or radiosurgery.
Other emergencies: Endovascular treatments can target dural fistulas, vasospasm after subarachnoid hemorrhage, and selected bleeding sources. - Related terms: aneurysm coiling vs clipping outcomes; carotid artery stenting vs endarterectomy.
Prevention and Life After Stroke
Preventing the first stroke—or a second one—is just as important as emergency care. The pillars are controlling blood pressure, managing atrial fibrillation, stopping smoking, treating diabetes and cholesterol, staying active, and taking prescribed medications.
Medications and Lifestyle That Lower Risk
- Blood pressure: Target per your doctor; it’s the most powerful modifiable risk factor.
- Cholesterol: Statins reduce ischemic stroke risk, especially after an event.
- Diabetes: Tight control lowers vascular complications. Apollo 24|7 offers convenient home collection for tests like HbA1c and lipid panel to guide management.
- Atrial fibrillation: Anticoagulants lower stroke risk substantially in eligible patients.
- Lifestyle: No smoking, moderation in alcohol, Mediterranean-style diet, and regular aerobic plus strength exercise.Related terms: blood pressure control to prevent stroke; stroke prevention with atrial fibrillation.
Secondary Prevention Procedures (PFO Closure, Carotid Stent)
- Patent foramen ovale (PFO) closure may be considered in certain younger patients with cryptogenic stroke after thorough evaluation .
- Carotid endarterectomy or stenting for symptomatic carotid stenosis reduces recurrent stroke risk; choice depends on anatomy and risk profile.
- Work with a stroke specialist to tailor the plan; if your condition does not improve or you have recurrent symptoms, book a visit to a doctor with Apollo 24|7 for further evaluation and coordinated care.
Rehabilitation After Thrombectomy: Setting Expectations
- Early mobilization, task-specific therapy, and communication rehab are key.
- Recovery is not linear; plateaus can be followed by new gains.
- Track progress with your team using functional scales and goals that matter to you (e.g., walking independently, driving, returning to work).
- Unique insight: Create a “rehab dashboard”—a simple one-page tracker of weekly goals, barriers, and wins. Patients who co-create goals with therapists often stay more engaged and improve adherence.
Choosing Care, Costs, and the Future
How to Find a Comprehensive Stroke Center?
- Ask your local EMS which hospitals are designated thrombectomy-capable or comprehensive stroke centers.
- Look for 24/7 neurointerventional coverage, door-to-needle and door-to-groin metrics, access to advanced imaging, and robust rehabilitation services.
- Pro tip: Keep a “stroke go-bag” with your medication list, allergies, recent labs, and ID. Store a photo of this info on your phone and share with family.
Costs, Access, and Health Equity
Thrombectomy is cost-effective because it prevents disability, reducing long-term care needs .
Disparities exist by geography and socioeconomic status. Regionalized systems, tele-stroke networks, and streamlined transfers (“drip-and-ship” or “mothership” models) improve access .
Advocate locally for EMS routing protocols that prioritize thrombectomy-capable centers when suspected LVO is present.
Future Directions: AI Triage, Mobile Stroke Units, Robotics
- AI imaging tools can flag LVOs within minutes and support transfer decisions.
- Mobile stroke units (ambulances with CT scanners) can deliver tPA in the field and speed decisions about thrombectomy .
- Remote robotics and next-gen catheters may extend expert care to underserved areas in the future.
- Related terms: mobile stroke unit benefits; comprehensive stroke center near me.
Conclusion
Stroke doesn’t have to define the rest of your life. Thanks to interventional neurology, many people who would once have faced profound disability can now walk, talk, and return to what matters—if they get to the right care fast. You’ve learned how to spot stroke, why calling emergency services immediately is critical, and what happens during treatments such as tPA and mechanical thrombectomy. We also explored how interventional procedures address hemorrhages and aneurysms, and how lifestyle, medications, and targeted preventive procedures can reduce your risk of a first or recurrent event. Prepare now: identify a thrombectomy-capable hospital near you, set up a stroke go-bag, and share the BE FAST checklist with your family. If you have questions about your personal stroke risk, experience warning signs, or need help coordinating prevention and follow-up, consult a doctor with Apollo 24|7 and consider convenient home collections for key labs like HbA1c and cholesterol. When a stroke strikes, time matters—but preparation and knowledge matter, too.
Consult a Top Neurologist for Personalised Advice
Consult a Top Neurologist for Personalised Advice

Dr. Avinash Goswami
Neurologist
11 Years • MBBS, DNB (Medicine), Dr.NB (Neurology), MNAMS
Delhi
Apollo Hospitals Indraprastha, Delhi

Dr. Abhisek Nanda
Neurologist
10 Years • DM (NEUROLOGY) ,DNB(MEDICINE)
Rourkela
Apollo Hospitals, Rourkela, Rourkela
(150+ Patients)

Dr. Sanket Patel
Neurologist
4 Years • MBBS, DNB Medicine, DrNB Neurolgy
Ahmedabad
Apollo Hospitals - Gandhinagar, Ahmedabad, Ahmedabad
Dr. J C Rasmi Reddy
Neurologist
5 Years • M.B.B.S, M.D, DrNb in Neurology
Nellore
Apollo Speciality Hospitals, Nellore

Dr. Sreenivas U M
Neurologist
8 Years • MD, DM, MRCP (UK)
Chennai
Apollo Speciality Hospitals Vanagaram, Chennai
Consult a Top Neurologist for Personalised Advice

Dr. Avinash Goswami
Neurologist
11 Years • MBBS, DNB (Medicine), Dr.NB (Neurology), MNAMS
Delhi
Apollo Hospitals Indraprastha, Delhi

Dr. Abhisek Nanda
Neurologist
10 Years • DM (NEUROLOGY) ,DNB(MEDICINE)
Rourkela
Apollo Hospitals, Rourkela, Rourkela
(150+ Patients)

Dr. Sanket Patel
Neurologist
4 Years • MBBS, DNB Medicine, DrNB Neurolgy
Ahmedabad
Apollo Hospitals - Gandhinagar, Ahmedabad, Ahmedabad
Dr. J C Rasmi Reddy
Neurologist
5 Years • M.B.B.S, M.D, DrNb in Neurology
Nellore
Apollo Speciality Hospitals, Nellore

Dr. Sreenivas U M
Neurologist
8 Years • MD, DM, MRCP (UK)
Chennai
Apollo Speciality Hospitals Vanagaram, Chennai
More articles from Stroke
Frequently Asked Questions
What is the difference between tPA and mechanical thrombectomy?
tPA is a clot-busting medication given through a vein, most effective within 4.5 hours. Mechanical thrombectomy is an interventional procedure that physically removes large clots from brain arteries and can help selected patients up to 16–24 hours after onset.
How do I know if I’m a candidate for thrombectomy?
Candidates typically have a large-vessel occlusion, measurable symptoms, and imaging that shows salvageable brain tissue. Eligibility is determined rapidly in the emergency department with CT/MRI and vessel imaging.
Is stroke really the number one cause of disability?
Stroke is widely recognized as a leading cause of serious long-term disability in adults, impacting mobility, speech, cognition, and independence . Preventing and rapidly treating stroke are essential to reduce disability.
What can I do today to lower my stroke risk?
Control blood pressure, manage atrial fibrillation and diabetes, lower cholesterol, quit smoking, maintain a healthy weight, and stay active. Ask your doctor about a personalized plan; Apollo 24|7 offers home collection for tests like lipid panel and HbA1c.
What should I bring or prepare in case of a stroke?
Keep a “stroke go-bag” with a medication list, allergies, medical summary, recent labs, ID, and emergency contacts. Know the nearest comprehensive or thrombectomy-capable stroke center. Teach your family the BE FAST checklist and to call emergency immediately.