Your Guide to Revision Total Knee Replacement
Learn what to expect from revision total knee replacement surgery, including the procedure, recovery process, and tips for optimal outcomes.


Introduction
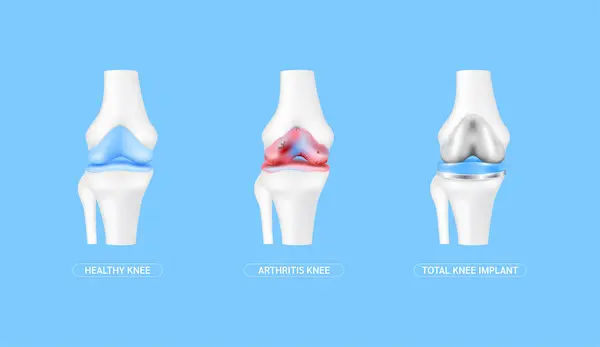
A total knee replacement is a highly successful surgery that relieves pain and restores function for millions. However, like any mechanical device, a knee implant may not last a lifetime. When a primary knee replacement wears out, becomes loose, or fails for other reasons, a second surgery known as a revision total knee replacement may be necessary. This procedure is significantly more complex than the first. It involves removing the original implant and replacing it with a new one. This guide is designed to walk you through everything you need to know, from understanding why a revision might be needed to what the recovery process truly entails. Our goal is to empower you with knowledge, so you can have informed discussions with your orthopedic specialist about your path forward.
Why Would a Knee Replacement Need to Be Revised?
A revision surgery isn't a decision taken lightly. Surgeons typically only recommend it when pain and loss of function significantly impact your quality of life. The reasons for failure are varied, but they generally fall into a few key categories.
Implant Loosening: The Most Common Cause
Over time, the bond between the implant and your bone can weaken. This is called aseptic loosening, meaning it occurs without an infection. The bone may recede (a process called osteolysis) from the implant, causing it to become unstable. This often leads to pain, especially when you start walking after a period of rest. It's the leading reason for revision total knee replacement many years after the initial surgery.
Wear and Tear of the Polyethylene Liner
The plastic spacer (polyethylene liner) that sits between the metal components acts as a cushion. While highly durable, it can wear down over 15-20 years of use. Tiny plastic particles can cause inflammation, which leads to bone loss. When the liner wears thin, it can cause metal-on-metal contact, leading to pain, squeaking, and further damage.
Infection: A Serious Complication
A periprosthetic joint infection is a devastating complication, occurring in a small percentage of cases. It can happen soon after surgery or years later. Bacteria can latch onto the implant, forming a biofilm that is resistant to antibiotics. Symptoms of a failing knee implant due to infection include persistent warmth, redness, swelling, drainage, and fever. Treating an infection often requires a two-stage revision: first to remove the infected implant and clear the infection, followed by a second surgery to implant the new knee.
Instability and Fractures Around the Implant
If the knee doesn't have the right balance of supporting ligaments, it can feel unstable or give way. This lack of support can necessitate revision. Additionally, a fall or trauma can cause a fracture in the bone around the implant, which may be too complex to fix without replacing the entire prosthesis.
Unique Insight: Surgeons are now using "synovial fluid biomarkers" as an emerging diagnostic tool. Analysing the fluid from your knee can sometimes detect signs of implant wear or inflammation long before they become visible on an X-ray, allowing for earlier intervention.
Consult an Orthopaedic Surgeon for the best advice
Recognising the Signs: Symptoms of a Failing Knee Implant
How do you know if your knee replacement is failing? The signs are often clear and progressive. The most common symptom is the return of pain. This isn't the mild, occasional ache you might expect, but a significant, deep pain that can occur at rest, at night, or during weight-bearing activities. You might feel a sense of instability, as if your knee is buckling or giving out. Stiffness that makes it difficult to bend or straighten your knee can return. Swelling around the joint that doesn't resolve is another red flag. If you experience any of these symptoms of failed knee replacement, it's crucial to consult your orthopedic surgeon for a thorough evaluation. If your knee pain persists or worsens, consulting a specialist online with Apollo24|7 can be a good first step to discuss your symptoms and determine if an in-person visit is necessary.
The Diagnostic Journey: Confirming the Need for Revision
Determining the exact cause of failure is a meticulous process. It begins with a detailed discussion of your symptoms and medical history. Your surgeon will then perform a physical examination, assessing your knee's range of motion, stability, and alignment.
Advanced Imaging: X-rays, CT Scans, and MRIs
X-rays are the first-line imaging tool. They can reveal obvious signs like implant loosening (a gap between the bone and implant), fractures, or significant wear. However, for a more detailed view, a CT scan is often used. It provides a 3D image that helps the surgeon assess bone loss and plan the complex reconstruction required in a revision knee surgery. In some cases, special MRI sequences can be used to evaluate the soft tissues around the implant.
Laboratory Tests for Infection
If infection is suspected, your surgeon will order blood tests, such as an ESR (Erythrocyte Sedimentation Rate) and CRP (C-Reactive Protein), which are markers of inflammation in the body. The definitive test is an aspiration, where fluid is drawn from your knee joint with a needle and sent to a lab to culture for bacteria. Apollo24|7 offers convenient home collection for routine blood tests like CRP, which can be part of the initial diagnostic workup.
Get Your Health Assessed
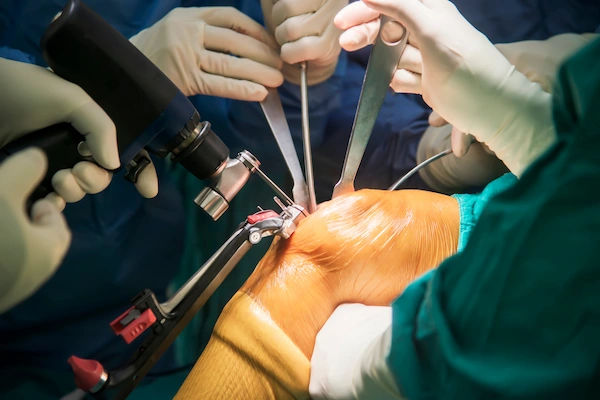
The Revision Surgery Procedure: A More Complex Operation
A revision is not simply a repeat of the first surgery. It is longer, more technically demanding, and carries higher risks.
Preoperative Planning: The Blueprint for Success
This is perhaps the most critical phase. Using the information from your diagnostic tests, your surgical team creates a detailed plan. They select the specific type of revision knee implants needed, which are often more robust and have longer stems to anchor into the bone marrow canal for stability. They also plan for potential bone grafts or specialised metal augments to fill any bone defects.
The Surgical Challenge: Implant Removal and Bone Loss
The first major challenge is safely removing the old implant without causing further damage to the already compromised bone. Specialised tools are used to break the implant-bone interface. Once the implant is out, the surgeon debrides the area, removing any unhealthy tissue or bone cement. Addressing bone loss is a key part of the procedure, using techniques like bone grafting or metal augments to rebuild the joint's foundation.
Reconstruction with Specialised Implants
After preparing the bone surfaces, the new components are implanted. These are typically "constrained" or "semi-constrained" implants, meaning they have built-in stability to compensate for any ligament damage. The goal is to create a stable, well-aligned knee that will restore function. The surgery can take anywhere from two to four hours or more.
The Road to Recovery: Rehabilitation After Revision Surgery
Recovery from a revision is generally slower and more challenging than from the initial replacement. Patience and commitment to rehabilitation are essential.
The Immediate Postoperative Period
You will likely stay in the hospital for a few days. Pain management is a priority. Physical therapy begins almost immediately, on the day of or the day after surgery. Initially, the focus is on safe movement getting in and out of bed and walking short distances with a walker. The goal is to prevent blood clots and maintain circulation.
Long-Term Physical Therapy Goals
After discharge, you will continue with outpatient physical therapy for several months. The recovery time for revision knee surgery is prolonged. Therapy focuses on restoring range of motion, but more critically, on building strength in the leg muscles that stabilise the new joint. You may need to use a walker or crutches for a longer period, often 6-8 weeks or more, to protect the reconstruction while it heals.
Weighing the Pros and Cons: Risks and Success Rates
The primary benefit of revision surgery is the relief of severe pain and the restoration of knee function, allowing you to return to an active lifestyle. However, the success rate of a second knee replacement is generally lower than for a primary replacement. Studies show a 85-90% success rate at 10 years, compared to over 95% for primary replacements.
Risks include all those of primary surgery (blood clots, infection, nerve damage) but at a higher rate. There's also a risk of continued pain, stiffness, and the possibility that the revision will not last as long as the original implant. The decision to proceed must be a careful balance between these factors and the impact of your current symptoms on your life.
Conclusion
Facing the prospect of a revision total knee replacement can feel daunting. It's a journey that requires resilience, patience, and a strong partnership with your medical team. However, for those struggling with the pain and disability of a failed knee implant, this procedure offers a powerful solution to reclaim mobility and quality of life. The key is to seek care from an orthopedic surgeon who specialises in revision joint replacement. They have the expertise and resources to navigate the complexities of your specific case. By understanding the reasons for revision, the intricate surgical process, and the dedicated rehabilitation required, you can approach this challenge with confidence. Remember, an informed patient is an empowered patient. Take this knowledge, ask questions, and actively participate in your care plan to achieve the best possible outcome.
Consult an Orthopaedic Surgeon for the best advice
Consult an Orthopaedic Surgeon for the best advice

Dr. Anil Pradeep Jadhav
Orthopaedician
23 Years • MBBS MS (Ortho)
Nashik
Apollo Hospitals Nashik, Nashik
(25+ Patients)

Dr. Rupam Chowdhury
Orthopaedician
10 Years • MBBS, DNB (Ortho.)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr. Suraj Prakash
Orthopaedician
5 Years • MBBS, MS (Ortho)
Bengaluru
Apollo Clinic, Indiranagar, Bengaluru

Dr. Padam Singh Gautam
General Physician/ Internal Medicine Specialist
43 Years • M.B.B.S (WARDHA M. S.), F.A.G.E. (MANIPAL), F.A.I.M.S. (Pb.), M.A.I.M.S. (Pb.), M.R.S.H. (LONDON)
Noida
Dr Padam Singh Gautam Fracture Clinic, Noida

Dr. Susheel B
Orthopaedician
13 Years • MBBS, MS, Ortho Fellowship in Trauma ( Germany) Fellowship in Arthroscopy and Arthroplasty ( Switzerland)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru
Consult an Orthopaedic Surgeon for the best advice

Dr. Anil Pradeep Jadhav
Orthopaedician
23 Years • MBBS MS (Ortho)
Nashik
Apollo Hospitals Nashik, Nashik
(25+ Patients)

Dr. Rupam Chowdhury
Orthopaedician
10 Years • MBBS, DNB (Ortho.)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr. Suraj Prakash
Orthopaedician
5 Years • MBBS, MS (Ortho)
Bengaluru
Apollo Clinic, Indiranagar, Bengaluru

Dr. Padam Singh Gautam
General Physician/ Internal Medicine Specialist
43 Years • M.B.B.S (WARDHA M. S.), F.A.G.E. (MANIPAL), F.A.I.M.S. (Pb.), M.A.I.M.S. (Pb.), M.R.S.H. (LONDON)
Noida
Dr Padam Singh Gautam Fracture Clinic, Noida

Dr. Susheel B
Orthopaedician
13 Years • MBBS, MS, Ortho Fellowship in Trauma ( Germany) Fellowship in Arthroscopy and Arthroplasty ( Switzerland)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru
More articles from Total Knee Replacement
Frequently Asked Questions
1. How long does a revision knee replacement last?
While a primary knee replacement can last 20 years or more, a revision implant typically has a shorter lifespan, often estimated at 10-15 years. This is due to the more complex nature of the surgery and the potential for increased stress on the components.
2. Is the pain worse after a revision than the first knee replacement?
The initial postoperative pain may be more significant due to the more extensive surgical dissection and longer operative time. However, modern pain management protocols are very effective. The goal is to replace the chronic, debilitating pain you had before surgery with manageable, temporary surgical pain that improves with healing.
3. What is the typical recovery time for revision knee surgery?
Recovery time for revision knee surgery is generally longer. While you may be walking with a walker within a day or two, full recovery can take a year or more. Most people use a walker for 6-8 weeks and require formal physical therapy for 3-6 months before returning to most daily activities.
4. Can a revision knee replacement be revised again?
Yes, it is possible, but it becomes exponentially more difficult with each subsequent surgery. The bone stock diminishes, and scarring increases, making the procedure highly complex. This is why choosing an experienced surgeon for your first revision is so important.
5. Will I be able to bend my knee as well after a revision?
The goal of surgery is to improve your range of motion. However, achieving the same degree of bend as after a primary replacement can be challenging, especially if there was significant scar tissue or bone loss. Your commitment to physical therapy is the most important factor in maximising your final range of motion.