Guide to Climate Change And Tuberculosis
Explore how climate change is worsening the tuberculosis crisis and impacting global health, with insights on prevention and awareness.

Written by Dr. Dhankecha Mayank Dineshbhai
Reviewed by Dr. Vasanthasree Nair MBBS
Last updated on 13th Jan, 2026

Introduction
When we think about the impacts of climate change, images of melting glaciers, extreme weather, and rising sea levels often come to mind. But a more insidious threat is brewing, one that connects our planet's health directly to our own: the resurgence of infectious diseases like tuberculosis (TB). TB, an ancient disease caused by the bacterium Mycobacterium tuberculosis, remains one of the world's deadliest infectious killers. While modern medicine has made strides in its treatment, the escalating climate change crisis is undoing progress and creating a perfect storm for tuberculosis to thrive. This article will unravel the complex links between a warming planet and this pulmonary disease. We'll explore how factors like malnutrition, displacement, and overwhelmed health systems are increasing vulnerability to TB. More importantly, we'll provide guidance on recognising risks, seeking timely care, and understanding how protecting our environment is intrinsically linked to safeguarding our health from diseases like tuberculosis.
The Unseen Link: Connecting a Warming Planet to an Ancient Disease
To understand the connection, we must first look at the two players individually. Climate change is not just about temperature; it's a cascade of environmental disruptions including altered rainfall patterns, more frequent and severe droughts and floods, and increased air pollution.
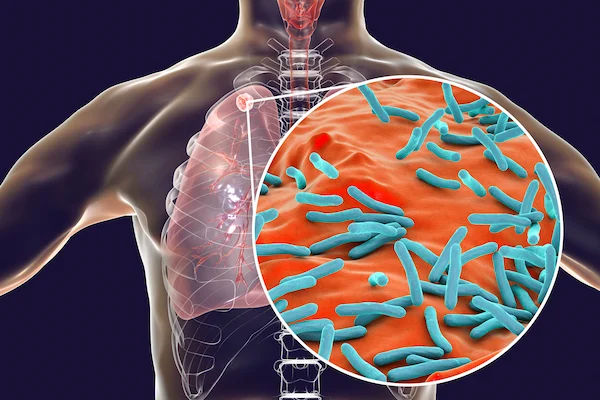
Understanding Tuberculosis (TB) in the Modern World
Tuberculosis primarily affects the lungs and is spread through the air when a person with active TB coughs, sneezes, or speaks. It's important to distinguish between latent TB infection (where bacteria live in the body without making you sick) and active TB disease. Factors that weaken the immune system, like HIV, diabetes, or malnutrition, can cause latent TB to become active. This is where climate change acts as a dangerous catalyst.
The Broad Strokes of Climate Change's Health Impacts
The World Health Organisation (WHO) has declared climate change the single biggest health threat facing humanity. It impacts the social and environmental determinants of health, clean air, safe drinking water, sufficient food, and secure shelter. By destabilising these pillars, it creates conditions where diseases like malaria, dengue, and TB can flourish, posing a significant challenge to public health infrastructure worldwide.
The Direct Pathways: How Climate Change Worsens TB Risk
The link isn't just theoretical; it's backed by growing evidence. A 2023 study published in The Lancet Planetary Health found a correlation between extreme climate events and increased TB incidence, highlighting two primary pathways.
Malnutrition and Food Insecurity: Weakening the Body's Defences
Climate-induced droughts and floods devastate agriculture, leading to crop failure and food shortages. This results in widespread malnutrition, which severely compromises the immune system. A malnourished body is far less capable of fighting off infections or keeping latent TB in check. This creates a direct pathway where food insecurity, driven by climate change, leads to higher rates of active tuberculosis disease. This is a critical point of the link between malnutrition and tuberculosis.
Population Displacement and Overcrowding: Creating Ideal Conditions for Spread
As sea levels rise and storms become more violent, millions of people are forced to leave their homes. These climate refugees often end up in temporary shelters or informal settlements that are densely populated and poorly ventilated. Overcrowding is a classic risk factor for TB transmission, as the bacteria spread easily in close quarters. This situation creates a perfect environment for a rapid increase in tuberculosis cases, demonstrating how population displacement fuels outbreaks.
Consult a Pulmonologist for the best advice
The Indirect Threats: Straining the Systems that Fight TB
Beyond direct health risks, climate change cripples the very systems designed to protect us.
Disruption of Healthcare Services and Supply Chains
Extreme weather events can destroy clinics, disrupt transportation, and halt the delivery of essential medical supplies.
This means interruptions in TB diagnosis, treatment, and the distribution of medicines. Consistent treatment is vital for
curing TB and preventing the development of drug-resistant strains. When climate change disrupts healthcare services, it jeopardises years of progress in TB control.
The Financial Drain: Diverting Resources from TB Control
Governments and aid organisations are forced to spend billions on disaster relief and rebuilding efforts after climate-related catastrophes. This financial pressure often leads to reduced funding for long-term public health programs, including TB eradication initiatives. The money needed to fight tuberculosis is increasingly being diverted to address the immediate damages of climate change, creating a vicious cycle.
A Double Burden: Climate Change and Drug-Resistant TB
The convergence of these factors creates a particularly alarming scenario: the rise of drug-resistant TB (MDR-TB). When TB treatment is interrupted due to displaced populations losing access to care or supply chain breakdowns, it increases the risk of the bacteria mutating and becoming resistant to first-line drugs. Treating MDR-TB is far more complex, expensive, and lengthy, putting an even greater strain on already fragile health systems. This makes the impact of climate change on TB a multiplier for an already severe health crisis.
Protecting Yourself and Your Community in a Changing Climate
While the global challenge is immense, individual and community awareness is the first line of defence.
Recognising the Symptoms of TB
Knowing the signs of active pulmonary TB is crucial. They include:
- A persistent cough that lasts for three weeks or more.
- Chest pain.
- Coughing up blood or sputum.
- Unintentional weight loss.
- Fever, night sweats, and chills.
- Fatigue.
When to Seek Professional Medical Advice
If you or someone you know experiences a persistent cough along with other symptoms like weight loss and fever, it is
essential to seek medical evaluation promptly. Early diagnosis and treatment are key to recovery and preventing spread. If symptoms persist beyond two weeks, consult a doctor online with Apollo24|7 for further evaluation. They can guide you on the next steps, which may include a simple skin test or a sputum test.
Supporting Community Health and Resilience
You can contribute by supporting policies that address climate change, advocating for robust public health funding, and promoting community initiatives that improve nutrition and housing. Strengthening community health resilience is a powerful tool in the fight against diseases like TB in a changing climate.
Conclusion
The evidence is clear: the fight against tuberculosis cannot be won without addressing climate change. The two are inextricably linked through a web of environmental, social, and economic factors. From worsening malnutrition to destroying healthcare infrastructure, the impacts are already being felt, particularly in vulnerable communities. While the scale of the problem requires global action, individual awareness is powerful. Understanding the risks, recognising the symptoms of TB, and seeking timely medical care are critical steps in protecting your health. If you have concerns about a persistent cough or other symptoms, don't hesitate to seek professional guidance. By taking care of our health and advocating for a stable planet, we can work towards a future where ancient diseases like TB are finally consigned to history.
Consult a Pulmonologist for the best advice
Consult a Pulmonologist for the best advice

Dr Rikin Hasnani
Pulmonology Respiratory Medicine Specialist
14 Years • MBBS NTR University of Health Sciences MD NTR University of Health Sciences
Hyderguda
Apollo Hospitals Hyderguda, Hyderguda

Dr. Keshavan. V.
Pulmonology Respiratory Medicine Specialist
10 Years • "MBBS (CMC, Vellore) MD (CMC, Vellore) DNB EDARM (France) SCE(UK) ATSF (USA) MRCPS (Glasgow) FCCP (USA) FAPSR (Japan) MNAMS"
Hyderguda
Apollo Hospitals Hyderguda, Hyderguda
(25+ Patients)

Dr. Varun Kumar K
Pulmonology Respiratory Medicine Specialist
12 Years • DNB Respiratory Medicine
Secunderabad
Apollo Hospitals Secunderabad, Secunderabad

Dr. Sumara Maqbool
Pulmonology Respiratory Medicine Specialist
12 Years • MBBS, DNB Respiratory, critical care and sleep medicine, DrNB superspeciality Critical care, IDCCM, IFCCM, EDIC
Delhi
Apollo Hospitals Indraprastha, Delhi
(25+ Patients)

Dr. Dawar Masud Rizavi
Pulmonology Respiratory Medicine Specialist
26 Years • MBBS, MD (Respiratory Diseases & TB) MRCP (London, UK)
Lucknow
Apollomedics Super Speciality Hospital, Lucknow
Consult a Pulmonologist for the best advice

Dr Rikin Hasnani
Pulmonology Respiratory Medicine Specialist
14 Years • MBBS NTR University of Health Sciences MD NTR University of Health Sciences
Hyderguda
Apollo Hospitals Hyderguda, Hyderguda

Dr. Keshavan. V.
Pulmonology Respiratory Medicine Specialist
10 Years • "MBBS (CMC, Vellore) MD (CMC, Vellore) DNB EDARM (France) SCE(UK) ATSF (USA) MRCPS (Glasgow) FCCP (USA) FAPSR (Japan) MNAMS"
Hyderguda
Apollo Hospitals Hyderguda, Hyderguda
(25+ Patients)

Dr. Varun Kumar K
Pulmonology Respiratory Medicine Specialist
12 Years • DNB Respiratory Medicine
Secunderabad
Apollo Hospitals Secunderabad, Secunderabad

Dr. Sumara Maqbool
Pulmonology Respiratory Medicine Specialist
12 Years • MBBS, DNB Respiratory, critical care and sleep medicine, DrNB superspeciality Critical care, IDCCM, IFCCM, EDIC
Delhi
Apollo Hospitals Indraprastha, Delhi
(25+ Patients)

Dr. Dawar Masud Rizavi
Pulmonology Respiratory Medicine Specialist
26 Years • MBBS, MD (Respiratory Diseases & TB) MRCP (London, UK)
Lucknow
Apollomedics Super Speciality Hospital, Lucknow
More articles from Tuberclosis
Frequently Asked Questions
1. Does air pollution directly cause tuberculosis?
Air pollution doesn't directly cause TB, as the disease is caused by a specific bacterium. However, exposure to high levels of air pollution (like PM2.5 particles) damages the lungs and weakens the immune system, making individuals more susceptible to TB infection and more likely to progress from latent to active disease.
2. I live in a city with high air pollution. What is my TB risk?
While high air pollution is a risk factor, it is one of many. Your overall risk depends on other factors like your nutritional status, proximity to someone with active TB, and overall health. Practicing good hygiene, maintaining a healthy diet, and being aware of the symptoms are the best protective measures. If you have a weakened immune system, consult a doctor for personalised advice.
3. How does climate change specifically affect TB diagnosis?
Climate-related disasters can destroy diagnostic facilities, cut off power needed to run lab equipment, and prevent people from reaching health centres for testing. This leads to delays in diagnosis, allowing the disease to spread further and progress to more severe stages.
4. Are some populations more vulnerable to climate-related TB spread?
Yes, populations in low-income countries, particularly those dependent on agriculture, coastal communities, and informal urban settlements, are disproportionately affected. They often have higher existing TB burdens, weaker health systems, and fewer resources to adapt to climate shocks.
5. Can the BCG vaccine protect against these new threats?
The BCG vaccine is effective at preventing severe forms of TB in children but offers variable protection against pulmonary TB in adults. While vaccination is important, it is not a silver bullet against the increased transmission driven by climate change. A multi-pronged approach focusing on prevention, robust healthcare, and climate action is essential.