What Leads To Symptoms Types Of Spinal Tuberculosis
Learn about spinal tuberculosis (Pott disease)—its symptoms, causes, types, diagnosis, and treatment options. Understand how inflammation and bone damage cause pain and when surgery may be needed.

Written by Dr. Mohammed Kamran
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 13th Jan, 2026

Back pain that won’t go away, night sweats, and fatigue are easy to dismiss—until they add up to something serious. Spinal tuberculosis (also called Pott disease or tuberculous spondylitis) is an infection caused by Mycobacterium tuberculosis that travels from the lungs or another site to the bones and discs of your spine. It’s the most common form of skeletal TB and can lead to nerve compression, deformity, and long-term disability if not treated early. This comprehensive guide explains what leads to symptoms, the types of spinal tuberculosis doctors talk about, how it is diagnosed, and the treatments that work. You’ll learn how inflammation, bone destruction, and abscesses cause pain and weakness; how MRI and biopsy confirm the condition; and when medicines are enough versus when surgery is needed. We’ll also cover recovery, prevention, and practical tips for living well during treatment. If you’re seeking clear answers for yourself or a loved one, you’re in the right place.
Understanding Spinal Tuberculosis (Pott Disease)
Before exploring the symptoms and types, it’s important to understand what spinal tuberculosis actually is and how it develops in the body.
What spinal tuberculosis is—and isn’t
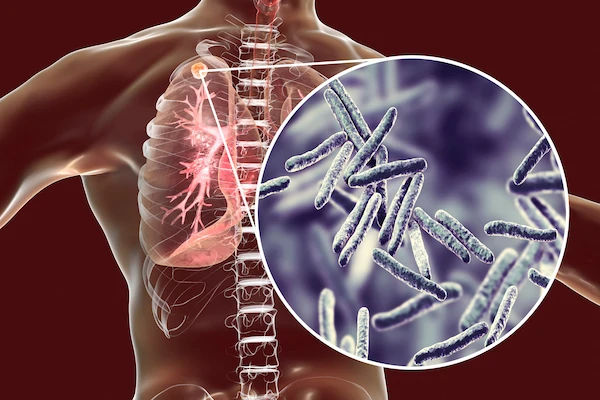
Spinal tuberculosis is a form of extrapulmonary TB where the TB bacteria infect the vertebrae and intervertebral discs.
You may also hear “Pott disease” or “tuberculous spondylitis.” While pulmonary TB affects the lungs and is more
infectious through coughing, spinal TB is primarily a local disease causing bone and soft tissue damage; the spine itself
does not spread TB through casual contact. However, active TB elsewhere (especially lungs) can be contagious, so
evaluation for pulmonary TB is part of care.
Spinal tuberculosis accounts for roughly half of all skeletal TB cases. It can occur at any age, with a predilection for the
thoracic and lumbar regions. In countries with high TB prevalence or among people with weak immune systems, cases
are more common.
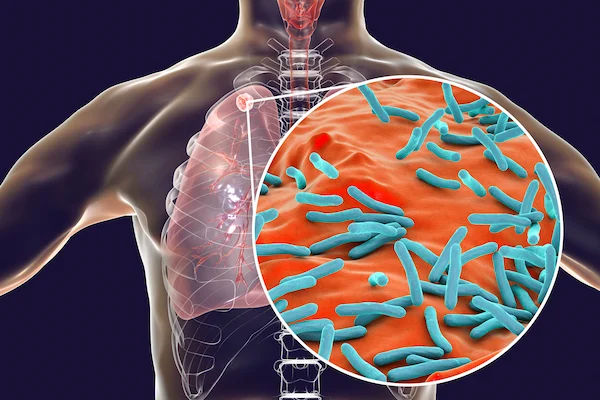
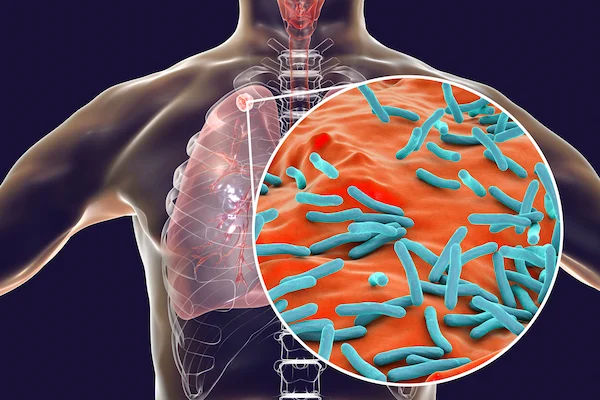
How TB bacteria reach the spine
TB bacteria typically spread through the bloodstream or lymphatics from a primary site (often the lungs) to the spine.
They lodge in the highly vascular regions of the vertebral bodies, sometimes using the valveless venous plexus (Batson’s
plexus) as a conduit. Once established, the bacteria trigger chronic inflammation, leading to bone destruction
(osteolysis), disc involvement, and formation of “cold abscesses” (collections of pus without redness or heat). This
process underlies most symptoms and complications of spinal tuberculosis.
The slow pace of TB inflammation means symptoms often creep up over weeks to months, distinguishing it from
sudden mechanical back strains.
Consult Top Specialists
The Types of Spinal Tuberculosis (Classifications You’ll Hear)
Spinal tuberculosis can appear in several forms depending on where and how the infection spreads. Understanding these
types helps predict symptoms and guide treatment:
Paradiscal type
This is the most common type. The infection starts near the endplates of two adjacent vertebral bodies and spreads into
the intervertebral disc. As the disc collapses, the vertebrae move closer, producing progressive kyphosis (forward bend).
Paradiscal disease is a frequent cause of TB spondylodiscitis and often presents with persistent back pain, muscle spasm,
and stiffness.
Central (vertebral body) type
Here, the infection sits in the centre of a vertebral body, causing a “vertebra plana” appearance (flattened vertebra) on
imaging when severe. Because discs are initially spared, early X-rays may be subtle. Central lesions may cause
instability or collapse, with pain that worsens on standing or walking.
Anterior subligamentous (migratory) type
TB can track under the anterior longitudinal ligament across multiple levels. This creates long collections of pus and
widespread anterior vertebral erosion. Patients may have a visible or palpable fullness from a paravertebral abscess and
more extensive kyphosis.
Posterior element (appendiceal) type
This type involves the posterior elements—pedicles, laminae, and spinous processes. Because the infection is close to the spinal canal, even small lesions can cause significant nerve compression. Symptoms often include local tenderness and early neurological deficits such as sciatica-like pain.
Atypical and non-contiguous (“skip”) lesions
In atypical cases, multiple nonadjacent spinal segments are involved, or only the posterior elements are diseased. Non-
contiguous disease can be overlooked if imaging is limited to one region, so full-spine MRI is recommended when suspicion is high.
Types can overlap—for example, a paradiscal lesion can evolve into an anterior subligamentous spread, showing why
follow-up imaging matters during treatment.
What Leads to Symptoms in Spinal TB?
Symptoms in spinal TB result from the body’s inflammatory response and the structural damage it causes to bone, discs, and surrounding tissues. Here are the symptoms:
Bone destruction, disc collapse, and deformity
TB bacteria provoke granulomatous inflammation that gradually eats into bone. When the disc is involved, it loses
height, the vertebrae approximate, and a kyphotic deformity can develop. Kyphosis alters spinal mechanics, increases
pain, and can narrow the space for the spinal cord, risking paralysis. Children are particularly prone to deformity
because their bones are still developing.
Abscesses: paravertebral, psoas, and epidural
Spinal TB often forms “cold” abscesses—collections of pus that lack heat or redness. These can track along tissue
planes:
- Paravertebral abscesses can cause visible swelling or fullness.
- Psoas abscesses (from lumbar TB) may present with groin or lower abdominal pain and difficulty extending the hip.
- Epidural abscesses can compress the spinal cord, causing weakness or numbness—a medical emergency.
Pain that worsens at night and is unrelieved by rest often signals an infectious cause like TB.
Symptoms and Red Flags You Shouldn’t Ignore
Recognising early signs can make a crucial difference in recovery. Seek prompt evaluation if you notice these warning
symptoms. Here are the symptoms you should know about:
Common early symptoms (pain, fever, weight loss)
- Persistent, localised back or neck pain
- Low-grade fever and night sweats
- Weight loss, fatigue, and stiffness
- Local tenderness over the spine
A classic scenario is a person with months of dull back pain, night sweats, and weight loss who finds little relief from rest or physiotherapy.
Neurological symptoms (radiculopathy to paraplegia)
If the infection compresses nerves or the spinal cord, symptoms may include:
- Shooting pain, tingling, or numbness in the arms or legs
- Weakness or difficulty walking
- Loss of bladder or bowel control (urgent sign)
- Saddle anaesthesia (numbness around the groin or buttocks)
Early recognition and treatment improve recovery chances.
Children vs. adults: how signs differ
Children may refuse to walk or show a visible hump due to growth-related deformity, while adults usually present with
chronic pain and fatigue. In both, progressive weakness or bladder issues are red flags.
If symptoms persist beyond two weeks, or you notice weakness or bladder issues, consult a doctor online with Apollo 24
|7 for evaluation. Sudden loss of bladder control or new weakness requires emergency care.
How Spinal TB Is Diagnosed
Diagnosis combines clinical suspicion, imaging, and laboratory confirmation to ensure accurate and timely treatment.
Here’s how spinal TB is diagnosed:
Clinical exam and basic blood tests (ESR/CRP)
Doctors assess spinal tenderness, range of motion, and neurological function. Blood tests such as ESR and CRP often
rise during inflammation and help track progress. TB skin tests or interferon-gamma release assays show exposure but
cannot confirm spinal disease.
Imaging: X-ray, CT, and MRI—what each shows
- X-ray: Shows late changes like vertebral collapse and disc space loss.
- CT: Highlights bone destruction and helps guide biopsies.
- MRI: Detects early inflammation, abscesses, and spinal cord compression. It’s the preferred tool for diagnosis.
Microbiology and pathology: biopsy, GeneXpert/CBNAAT, culture
A definitive diagnosis requires tissue confirmation. CT- or MRI-guided biopsy provides samples for:
- Microscopy and culture for Mycobacterium tuberculosis
- Molecular tests like GeneXpert/CBNAAT for detecting TB DNA and drug resistance
- Histopathology to identify granulomas typical of TB
Differential diagnosis (what else it could be)
Conditions like pyogenic spondylodiscitis, brucellosis, fungal infections, or spinal tumours can mimic TB.
Distinguishing features include slower onset and large abscesses with less systemic toxicity.
If your doctor recommends routine monitoring such as liver or blood tests, Apollo 24|7 offers convenient home
collection.
Treatment: Medicines, Monitoring, and Adherence
Medical therapy is the cornerstone of spinal TB management and is effective for most patients when followed diligently.
Here are the treatment options for Tuberculosis:
Standard anti-TB drug regimens and duration
Treatment usually includes:
- Intensive phase: Two months of isoniazid, rifampicin, pyrazinamide, and ethambutol
- Continuation phase: Isoniazid and rifampicin for 4–10 additional months
The duration typically ranges from 6 to 12 months depending on the site and response. Drug susceptibility tests like
GeneXpert help tailor therapy when resistance or HIV co-infection is suspected.
Side effects, liver tests, and staying on track
Anti-TB drugs may cause nausea, liver enzyme elevation, or visual changes. Regular liver function tests are advised.
Report any jaundice, vision problems, or severe rashes promptly.
Adherence tips:
- Take medicines consistently at the same time each day.
- Track your doses and consult your doctor for missed doses.
- Maintain a protein-rich diet and adequate hydration.
Supportive care: bracing, nutrition, pain control
Short-term rest may ease pain, but early guided mobilisation helps recovery. A brace supports unstable spines and
reduces discomfort. Nutrition plays a key role—adequate calories, protein, and vitamins promote healing.
If you don’t notice improvement, book an in-person visit with an Apollo 24|7 specialist for review.
When Surgery Is Needed and What Recovery Looks Like
While most cases respond to medical therapy, surgery becomes necessary when complications arise. Know more about
it:
Indications for surgery
- Progressive or severe neurological deficits
- Spinal instability or severe deformity
- Large abscesses causing compression
- Lack of improvement with medical therapy
- Diagnostic uncertainty requiring open biopsy
Timely surgery relieves pressure on nerves, corrects deformity, and stabilises the spine, always alongside anti-TB therapy.
Surgical approaches and outcomes
Common procedures include:
- Anterior debridement and fusion: Removing infected tissue and stabilising the front column.
- Posterior instrumentation: Using screws and rods for support.
- Combined approaches: For complex deformities.
When performed appropriately, surgery offers pain relief and improved neurological recovery.
Rehabilitation and return to activity
Rehabilitation involves gradual strengthening, posture training, and balance work. Most patients return to normal
activities over several months depending on initial severity.
Even without surgery, early physiotherapy under supervision prevents muscle weakness and stiffness.
Prevention, Prognosis, and Living Well After Spinal TB
Here’s how you can prevent and live well after a spinal TB:
Preventing spread and protecting family
Screening for pulmonary TB helps prevent airborne spread. Household members, especially children or those with weak
immunity, should be evaluated. BCG vaccination in infancy lowers the risk of severe childhood TB.
Managing comorbidities (HIV, diabetes) and nutrition
Managing conditions like HIV, diabetes, or malnutrition improves treatment outcomes. Controlling blood sugar,
maintaining good nutrition, and ensuring adequate vitamin D levels support recovery.
Myths vs. facts about spinal tuberculosis
- Myth: Back pain from TB improves with rest.
Fact: It usually persists and worsens at night. - Myth: Spinal TB is contagious.
Fact: The spine itself doesn’t spread TB; lungs can. - Myth: You must avoid all movement.
Fact: Controlled movement aids recovery. - Myth: Surgery means severe disease.
Fact: Surgery addresses complications and complements medicines.
With early diagnosis and full adherence to treatment, most people make a strong recovery and regain normal activity levels.
Conclusion
Spinal tuberculosis combines infection with mechanical damage, turning simple back pain into a complex medical problem. Recognising warning signs such as night pain, weight loss, and stiffness can lead to early diagnosis when medication alone often suffices. Understanding its types—paradiscal, central, anterior subligamentous, and posterior element—helps explain differences in severity and symptoms. Diagnosis depends on imaging and biopsy to confirm TB and detect resistance.
Most patients recover fully with appropriate medication, consistent monitoring, and good nutrition. Surgery, when needed, provides additional stability and nerve decompression. With timely treatment, the prognosis is good and long-term mobility can be restored. If symptoms persist or worsen, consult a doctor online with Apollo 24|7 or schedule an in-person visit for evaluation. Prompt care can prevent complications and help you return to an active, healthy life.
Consult Top Specialists
Consult Top Specialists

Dr. Chandrani Chatterjee
Pulmonology Respiratory Medicine Specialist
7 Years • MBBS,MD (Respiratory Medicine)
Kolkata
Samaritan Clinic, Kolkata

Dr. Tamal Bhattacharyya
Pulmonology Respiratory Medicine Specialist
8 Years • MBBS, MD (Respiratory Medicine)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr Vishwa Vijeth K.
Pulmonology Respiratory Medicine Specialist
8 Years • MBBS, MD ( Respiratory Medicine)
Bangalore
Apollo Clinic Bellandur, Bangalore
Dr. Preeti Kathail
General Physician/ Internal Medicine Specialist
17 Years • MBBS, PGDHHM
Bangalore
Apollo Clinic Bellandur, Bangalore
Dr. Naseeha Mohammed S V
Pulmonology Respiratory Medicine Specialist
6 Years • MBBS, MD ,DNB Respiratory Medicine
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru
Consult Top Specialists

Dr. Chandrani Chatterjee
Pulmonology Respiratory Medicine Specialist
7 Years • MBBS,MD (Respiratory Medicine)
Kolkata
Samaritan Clinic, Kolkata

Dr. Tamal Bhattacharyya
Pulmonology Respiratory Medicine Specialist
8 Years • MBBS, MD (Respiratory Medicine)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr Vishwa Vijeth K.
Pulmonology Respiratory Medicine Specialist
8 Years • MBBS, MD ( Respiratory Medicine)
Bangalore
Apollo Clinic Bellandur, Bangalore
Dr. Preeti Kathail
General Physician/ Internal Medicine Specialist
17 Years • MBBS, PGDHHM
Bangalore
Apollo Clinic Bellandur, Bangalore
Dr. Naseeha Mohammed S V
Pulmonology Respiratory Medicine Specialist
6 Years • MBBS, MD ,DNB Respiratory Medicine
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru