Guide to Understanding Tuberculosis
Tuberculosis (TB) Guide: Learn about the symptoms, causes, diagnosis, and modern treatment options for TB, including latent and active disease. Find reliable facts here.

Written by Dr. J T Hema Pratima
Reviewed by Dr. D Bhanu Prakash MBBS, AFIH, Advanced certificate in critical care medicine, Fellowship in critical care medicine
Last updated on 13th Jan, 2026

Introduction
Tuberculosis remains one of the world’s leading infectious diseases, yet many people still have questions about how it spreads, how to recognize it, and what treatment involves. If you’re seeking understanding of tuberculosis for yourself or a loved one, this guide brings together trusted facts, practical advice, and up-to-date insights in one place. We’ll explain the difference between latent TB and active TB disease, clarify common symptoms and red flags, and walk you through modern tests like chest X-ray and molecular assays. You’ll learn about today’s shorter, all-oral treatment options, ways to prevent transmission at home, and what recovery can look like—including support for lung health and mental wellbeing. We’ll also address special considerations for children, pregnancy, and people with conditions like HIV or diabetes. Along the way, we’ll point to authoritative resources and highlight new innovations you may not see in other articles. Whether you’re worried about a persistent cough, supporting a family member, or simply want to stay informed, this understanding of tuberculosis guide is designed to help you act with confidence and compassion.
TB at a Glance: What It Is and Why It Matters
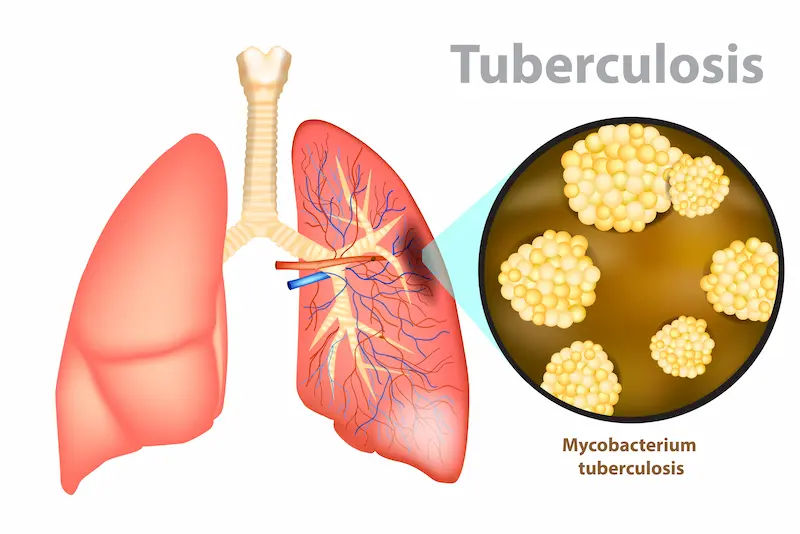
Tuberculosis (TB) is an infectious disease caused by Mycobacterium tuberculosis, a slow-growing bacterium that primarily affects the lungs but can involve the brain, lymph nodes, bones, or kidneys. Globally, TB remains a top infectious killer. The World Health Organization (WHO) estimates that about 10.6 million people developed TB in 2022, and approximately 1.3 million people died from TB among those without HIV, with additional deaths among people living with HIV [1]. Understanding tuberculosis starts with distinguishing between two states: latent TB infection (LTBI) and active TB disease. In LTBI, the bacteria are present but inactive; you feel well and cannot spread TB. In active TB disease, the bacteria multiply, causing symptoms and the potential to infect others.
Pulmonary TB (lungs) is the most common, and it’s responsible for most transmission through tiny air particles expelled when a person with active TB coughs, speaks, or sings. Extrapulmonary TB affects other organs and often requires tailored diagnostic approaches. The good news: TB is preventable and curable with proper treatment. Modern tools—such as rapid molecular tests (NAAT/Xpert), shorter treatment regimens, and prioritized contact tracing—are making a difference, even as drug-resistant TB remains a challenge.
Consult a Top General Physician
How TB Spreads—and How It Doesn’t
TB spreads through airborne particles from someone with active pulmonary TB. These microscopic droplets can stay suspended in the air, especially indoors with poor ventilation. Prolonged close contact—living in the same household, spending hours in a small room, or sharing transport over time—raises risk. Brief, casual outdoor contact usually carries much lower risk, especially with good airflow. Understanding tuberculosis also means debunking myths: you can’t get TB from sharing utensils, touching doorknobs, hugging, or from food and water. TB is not spread by mosquitoes.
The likelihood of infection depends on the infectiousness of the source (e.g., smear-positive, cavitary disease), duration and proximity of exposure, and environmental factors like ventilation and crowding. Masks, open windows, and air filtration reduce risk. In healthcare settings, airborne infection isolation rooms, N95 respirators, and careful sputum collection practices are standard. For families, practical measures—encouraging the person with TB to cover coughs, wear a mask during the early treatment phase, and maintain cross-ventilation—can protect others.
Myth-busting example: A coworker who had TB last year and completed treatment is not contagious now. In fact, most people become non-infectious within a few weeks of starting appropriate therapy. Long-tail terms included: how TB spreads through the air; TB prevention at home and work.
Who Is Most at Risk?
Anyone can develop TB, but some groups face a higher risk of infection or progression to disease. People with close exposure to someone with active pulmonary TB, those living in crowded or poorly ventilated settings, and healthcare workers are commonly affected. Certain medical conditions weaken immune defenses, including HIV, diabetes, undernutrition, chronic kidney disease, silicosis, and some cancers or medications that suppress immunity (e.g., steroids, biologics). Smoking and harmful alcohol use also increase risk. Children under five and older adults are more vulnerable to severe disease and complications.
Diabetes is an underappreciated driver: it roughly triples TB risk and can complicate treatment. If you have diabetes, strict glucose control supports TB recovery, and vice versa—successfully treating TB can improve glycemic control. Malnutrition is another key factor; balanced nutrition aids immunity and medication tolerance. In many settings, a quarter of the world’s population carries latent TB; while most never get sick, those with weakened immunity can progress to disease. This is why testing and preventive treatment for high-risk contacts—especially children and people with HIV—are critical.
Practical tip: If you live with someone being treated for active TB, your healthcare provider may recommend evaluation and, if appropriate, preventive therapy even if you feel well.
Long-tail terms: TB contact tracing process; TB and HIV coinfection guidance.
Unique insight: Household risk isn’t uniform—someone sleeping in the same room with the infectious person often has a higher risk than relatives in separate rooms. Simple changes in living patterns during early treatment can reduce exposure.
Signs and Symptoms: When to Seek Care
Classic symptoms of pulmonary TB include a persistent cough lasting more than two weeks, coughing up phlegm or blood, chest pain, fever, night sweats, fatigue, and unexplained weight loss. Not everyone has all these symptoms, and in children or older adults, signs can be subtle—poor weight gain, reduced activity, or nonspecific fevers. Extrapulmonary TB varies by site: swollen lymph nodes, back pain (spinal TB), abdominal pain, or persistent headaches if the brain is involved.
When to seek care: If you have a cough that won’t go away, fevers or night sweats, or weight loss—especially with a known exposure or risk factors—see a clinician promptly. Red flags needing urgent assessment include coughing up blood, severe breathlessness, confusion, persistent high fevers, or symptoms in very young children. Early diagnosis not only improves your outcome but also protects people around you.
If symptoms persist beyond two weeks, consult a doctor online with Apollo24|7 for further evaluation. A clinician can arrange appropriate tests or refer you to in-person services if needed. If you are acutely unwell (e.g., significant breathlessness), seek emergency care.
Getting Diagnosed: Tests You May Encounter
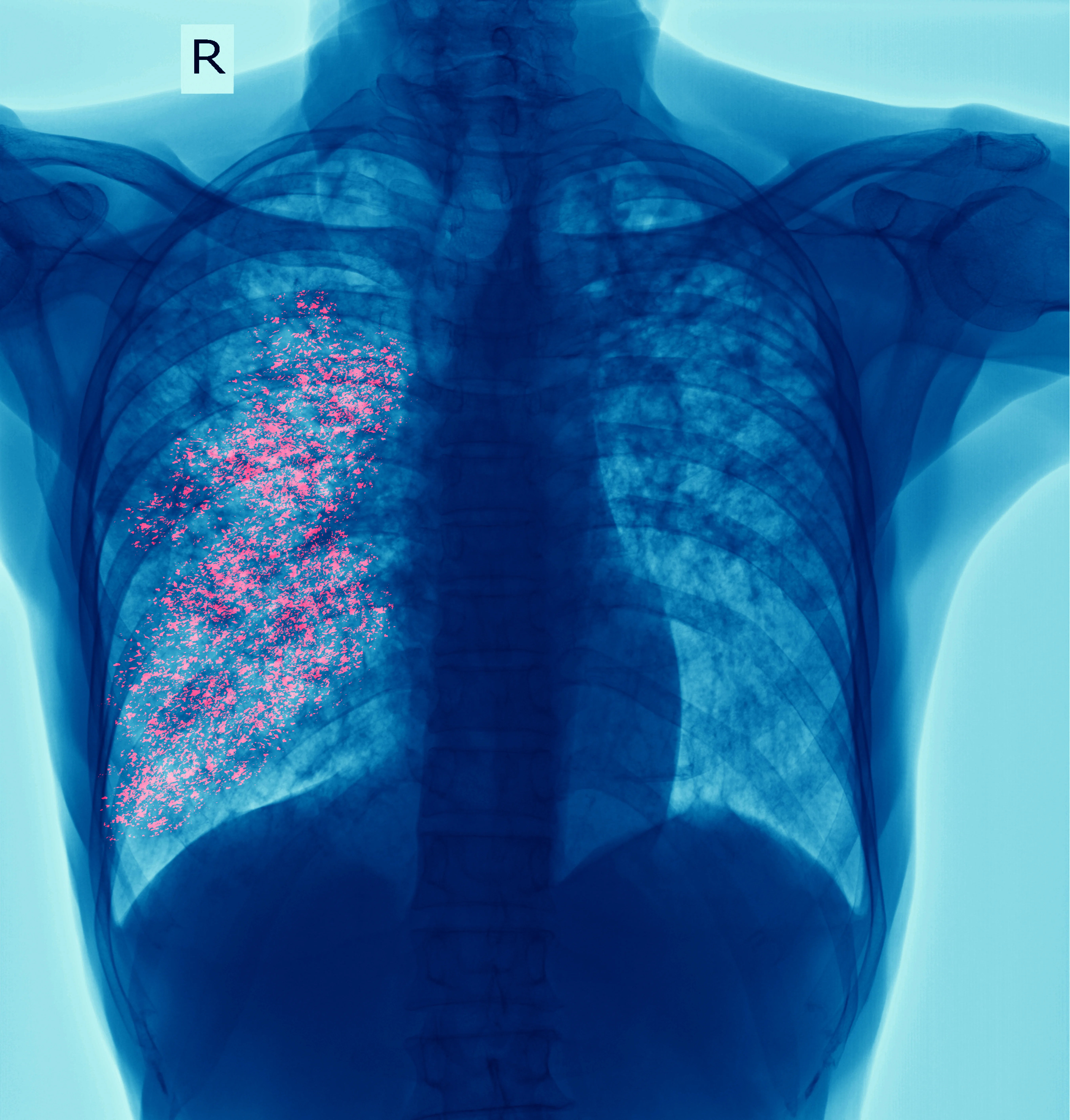
Diagnosis starts with a clinical evaluation and chest imaging, often a chest X-ray (CXR). If TB is suspected, sputum tests are essential. Sputum smear microscopy can show acid-fast bacilli, but it’s less sensitive and doesn’t detect drug resistance. Culture is the gold standard for confirming TB and allows full drug-susceptibility testing, but results take weeks. Rapid molecular tests—nucleic acid amplification tests (NAAT), such as Xpert MTB/RIF or Xpert Ultra—detect TB DNA and rifampicin resistance within hours to a day, and WHO recommends NAAT as the initial diagnostic test for people with signs and symptoms of TB.
For latent TB infection, the tuberculin skin test (TST) and interferon-gamma release assays (IGRAs) are used; a positive test indicates infection but not disease. You’ll still need an evaluation to rule out active TB before preventive treatment. In children or extrapulmonary disease, imaging (e.g., ultrasound, MRI) and specimen collection from other sites may be necessary.
• What results mean: A positive NAAT for TB suggests active disease, often prompting treatment while awaiting culture confirmation and broader drug-resistance results. A negative NAAT does not completely rule out TB, especially if symptoms and CXR are typical; clinicians may repeat testing or pursue culture. For latent infection, a positive IGRA with a normal CXR typically leads to discussion of preventive therapy.
If your condition does not improve after initial evaluation or you have difficulty accessing tests, book a physical visit to a doctor with Apollo24|7. Apollo24|7 also offers convenient home collection for common blood tests (e.g., vitamin D, HbA1c), which can help address comorbidities like diabetes that influence TB outcomes.
Treatment 101: From First-Line Therapy to Drug-Resistant TB
Drug-susceptible TB (DS-TB) is highly curable. Traditionally, treatment lasted six months with four drugs initially (isoniazid, rifampin, pyrazinamide, ethambutol) for two months, followed by two drugs for four months. Newer evidence supports a four-month regimen for pulmonary DS-TB in many adults and adolescents, using rifapentine and moxifloxacin in combination, achieving non-inferior outcomes in carefully selected patients [2][4]. Your clinician will decide the best option based on age, disease extent, and potential drug interactions.
Drug-resistant TB (DR-TB) requires specialized regimens. WHO now recommends shorter, all-oral regimens for many forms of multidrug-resistant or rifampicin-resistant TB, including the 6-month BPaLM regimen (bedaquiline, pretomanid, linezolid, moxifloxacin) in appropriate settings [1]. These advances improve tolerability and reduce the need for painful injections used in the past. Close monitoring is vital: common issues include liver enzyme elevations, neuropathy (isoniazid, linezolid), visual changes (ethambutol), and QT interval prolongation (bedaquiline). Always share your full medication list to avoid interactions (e.g., rifamycins can reduce effectiveness of many drugs, including some HIV therapies and contraceptives).
Adherence matters. People often feel better after a few weeks, but stopping early risks relapse and resistance. Digital tools—smart pill boxes, SMS reminders, or virtual adherence support—can help you complete therapy. If you experience side effects or cannot tolerate a medication, do not stop on your own; contact your healthcare provider to adjust safely.
If you’re navigating treatment decisions or side effects, consult a doctor online with Apollo24|7 for personalized guidance and coordination with local TB services.
Preventing TB: Protecting Yourself and Loved Ones
Prevention operates at multiple levels. Vaccination with BCG (Bacille Calmette–Guérin) is widely given to newborns in countries with higher TB burden and protects infants and young children against severe forms like TB meningitis. However, BCG has limited impact on adult pulmonary TB. For people exposed to TB or with risk factors, preventive therapy for latent infection is highly effective. Options include 3HP (once-weekly isoniazid + rifapentine for 12 doses), 4R (daily rifampin for 4 months), and 1HP (daily isoniazid + rifapentine for 1 month; commonly used in people with HIV). Your clinician will tailor choices based on age, interactions, and liver health.
At home, during the first weeks of treatment for an infectious case, simple measures reduce spread: fresh air circulation, wearing a mask when in close contact, spending time outdoors when feasible, and sleeping in separate spaces if possible. Cover coughs, and don’t delay testing for close contacts, especially children under five and people with weakened immunity.
Workplaces and schools benefit from good ventilation, symptom screening when appropriate, and prompt referral of suspected cases. Public health programs can help with contact tracing and preventive therapy. People with conditions like diabetes or HIV should keep routine follow-up and optimize control; addressing these comorbidities lowers TB risk.
TB in Children, Pregnancy, and Special Situations
• Children often have different TB patterns: they may develop disease soon after infection, sometimes with fewer bacteria, making sputum tests harder to obtain. Clinicians rely on a combination of exposure history, symptoms (e.g., persistent fever, poor weight gain), chest imaging, and alternative specimens (e.g., gastric aspirates) . Early diagnosis is essential to prevent severe forms like TB meningitis. Children tolerate treatment well, with weight-based dosing and child-friendly formulations increasingly available.
• During pregnancy, TB can be safely treated; the priority is protecting both parent and baby. Most first-line drugs are considered safe in pregnancy, but choices are individualized. Breastfeeding is generally encouraged with appropriate infection control during the infectious period and while on treatment. For people living with HIV, integrated care is crucial. TB is a leading cause of death among people with HIV, yet preventive therapy and early TB diagnosis dramatically reduce risk. Drug interactions require careful selection of regimens. If you’re pregnant, caring for a young child, or living with HIV, coordinate with specialized services.
If you need guidance on TB risk in pregnancy or concerns about child symptoms, book an online consultation with Apollo24|7 to discuss next steps and appropriate referrals. Long-tail terms: TB in children symptoms and care; TB and HIV coinfection guidance.
Living Through and Beyond TB
Recovery is more than finishing pills. Many people experience fatigue, low appetite, or mood changes. Nutrition supports healing: prioritize balanced meals with adequate protein, fruits, and vegetables; small, frequent portions can help during early treatment. For people who smoke, quitting improves outcomes and reduces relapse. Mental health matters—TB can bring stigma, isolation, and anxiety. Counseling, peer groups, and family education can make a major difference.
• Post-TB lung disease (PTLD) is increasingly recognized: after cure, some people have lingering breathlessness, cough, or reduced exercise capacity due to scarring or airway damage. Pulmonary rehabilitation, breathing exercises, and graded physical activity can improve quality of life. If you have persistent symptoms after completing treatment, ask about spirometry, a chest X-ray, or referral to a pulmonologist.
Keep follow-up appointments to monitor for side effects and assess response. If blood tests are part of your comprehensive care—such as HbA1c for diabetes or vitamin D levels—Apollo24|7 offers convenient home collection, making it easier to manage comorbidities alongside TB care.
The Global Picture: Trends, MDR-TB, and What’s Changing
TB trends reflect both progress and setbacks. According to WHO, 10.6 million people developed TB in 2022, with increases linked to disruptions during the COVID-19 pandemic. Drug-resistant TB remains a serious challenge; hundreds of thousands of people develop rifampicin-resistant or multidrug-resistant TB each year. On the bright side, shorter, all-oral regimens and improved diagnostics are scaling up, and more countries are adopting preventive therapy for household contacts and people with HIV.
• Innovation is accelerating: digital adherence technologies (DATs) provide reminders and allow remote check-ins; AI tools assist in reading chest X-rays where expert radiology is scarce; and new or repurposed drugs are reshaping treatment for drug-resistant TB. Research into next-generation vaccines aims to reduce adult pulmonary TB—potentially a game-changer for transmission.
Case example: Some programs report improved treatment completion with simple WhatsApp-based check-ins and refill reminders—low-cost tools with high impact. Still, gaps persist, especially in crowded urban areas and among people facing poverty, malnutrition, or stigma. Ending TB will require a whole-of-society approach: clinical excellence, strong public health, and social support. Long-tail terms: TB contact tracing process; TB adherence digital tools.
Your Next Steps: Care Pathways and How to Get Help
If you suspect TB:
• Don’t delay. Seek medical advice if cough or constitutional symptoms persist beyond two weeks, or sooner if you have risk factors.
• Expect an evaluation with a chest X-ray and sputum testing if pulmonary TB is suspected. Ask whether a rapid molecular test (Xpert) is available.
• Protect others while you wait: ventilate rooms, wear a mask in close contact, and cover coughs.
If you’re diagnosed:
• Start treatment promptly and take medications exactly as prescribed.
• Ask about regimen length (4 vs 6 months for DS-TB), potential side effects, and what to do if they occur.
• Encourage your household contacts—especially children—to be evaluated for TB and latent TB infection.
Support and follow-up:
• For non-urgent guidance or to discuss test options and comorbidities, consult a doctor online with Apollo24|7. If you need routine labs like HbA1c or vitamin D to optimize overall health during TB care, Apollo24|7 offers convenient home collection services.
• If your condition worsens or you develop severe side effects (e.g., jaundice, vision changes, severe rash), arrange an urgent in-person evaluation.
Conclusion
Understanding tuberculosis empowers you to act—whether that means seeking care for a stubborn cough, encouraging a family member to get tested, or supporting someone through treatment. TB spreads through the air from people with active pulmonary disease, but simple steps like improving ventilation and starting timely therapy quickly reduce risk. Today’s diagnostic tools, especially rapid molecular tests, help confirm TB and spot drug resistance earlier than ever. Treatment is effective, with shorter and more tolerable options now available for many. Prevention goes beyond the clinic: protecting children with BCG, offering preventive therapy to exposed contacts and high-risk groups, and addressing comorbidities such as HIV, diabetes, and undernutrition.
Recovery doesn’t end on the day you take your last pill. Pay attention to nutrition, mental health, and the possibility of post-TB lung symptoms—support and rehabilitation can restore quality of life. If you’re unsure where to start or you need help interpreting symptoms, consult a doctor online with Apollo24|7 for guidance, and arrange in-person evaluation if symptoms are severe or persist. Together—patients, families, and health systems—we can break the chain of transmission, replace stigma with support, and make TB a disease of the past. Keep this guide handy, share it with loved ones, and take the next step toward informed, compassionate care.Consult a Top General Physician
Consult a Top General Physician

Dr. Syed Ismail Ali
General Practitioner
7 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr. Srujana Mulakalapalli
General Physician/ Internal Medicine Specialist
5 Years • MBBS, MD (GENERAL MEDICINE)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru
(25+ Patients)

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Harshendra Jaiswal
General Physician/ Internal Medicine Specialist
12 Years • MBBS , MD (General medicine)
Kolkata
108 DHANA DHANVANTARI Clinic, Kolkata
(25+ Patients)
Consult a Top General Physician

Dr. Syed Ismail Ali
General Practitioner
7 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr. Srujana Mulakalapalli
General Physician/ Internal Medicine Specialist
5 Years • MBBS, MD (GENERAL MEDICINE)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru
(25+ Patients)

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Harshendra Jaiswal
General Physician/ Internal Medicine Specialist
12 Years • MBBS , MD (General medicine)
Kolkata
108 DHANA DHANVANTARI Clinic, Kolkata
(25+ Patients)
More articles from tuberculosis
Frequently Asked Questions
1) Is TB contagious after starting treatment?
Most people with pulmonary TB become far less contagious after a few weeks of effective therapy, but follow your clinician’s advice on precautions and masking.
2) What’s the difference between latent TB and active TB?
Latent TB means you carry the bacteria without symptoms and cannot spread it. Active TB causes illness and can be contagious. Testing and evaluation distinguish the two, and latent TB can be treated to prevent disease.
3) Do I need a NAAT/Xpert test for TB?
Rapid molecular tests are recommended by WHO as initial tests for suspected TB to speed diagnosis and detect rifampicin resistance. Your doctor will decide based on availability and your clinical picture.
4) Can children get TB, and how is it treated?
Yes. Children may have different signs, and testing can be challenging. Treatment is effective with weight-based dosing and child-friendly formulations. If a child has persistent fever, poor weight gain, or known exposure, seek care promptly.
5) How can I prevent TB at home if someone is diagnosed?
Ensure good ventilation, encourage masks during early treatment, separate sleeping spaces if possible, and arrange evaluation and preventive therapy for close contacts. If you need care coordination, consult a doctor online with Apollo24|7.