Tuberculosis Myths and Facts: A Complete Guide
Separate tuberculosis myths from facts with this complete guide. Learn about TB symptoms, diagnosis, treatment, and how to protect yourself while understanding the realities of this curable disease.

Written by Dr. Vasanthasree Nair
Reviewed by Dr. D Bhanu Prakash MBBS, AFIH, Advanced certificate in critical care medicine, Fellowship in critical care medicine
Last updated on 13th Jan, 2026

Introduction
Tuberculosis (TB) is one of the world's oldest and most misunderstood diseases. Despite being preventable and curable, it remains a major global health concern, surrounded by stigma, fear, and misinformation. These tuberculosis myths can prevent timely diagnosis and treatment, leading to worse health outcomes and further transmission.
This guide aims to separate fiction from fact, debunking the most common misconceptions about TB, its spread, who is at risk, and available treatments. Armed with accurate knowledge, you can protect yourself, support loved ones, and contribute to ending the stigma surrounding this disease. Let’s uncover the truth about tuberculosis.
What is Tuberculosis? A Quick Refresher
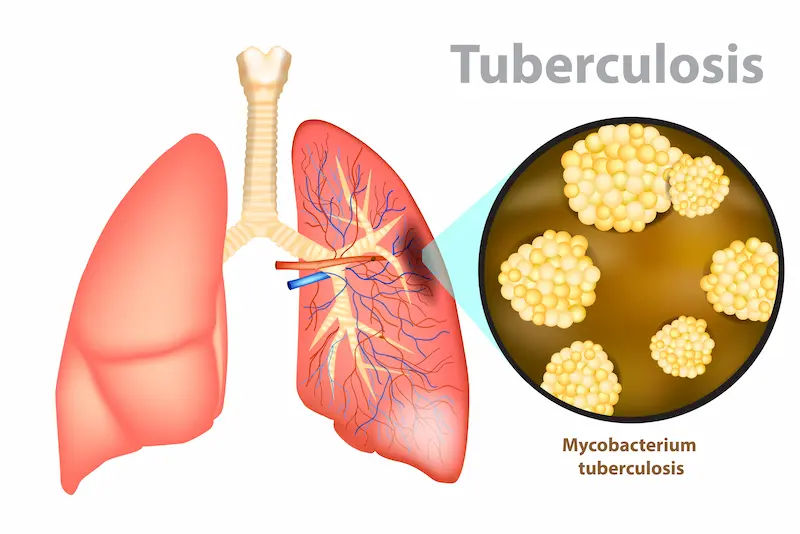
Tuberculosis is a potentially serious infectious disease caused by the bacterium Mycobacterium tuberculosis. It primarily affects the lungs but can also impact other parts of the body, such as the kidneys, spine, and brain. TB bacteria spread through the air when a person with active TB in their lungs coughs, sneezes, speaks, or sings. It is important to understand that not everyone infected with TB bacteria becomes sick.
Latent TB Infection (LTBI) vs. Active TB Disease
Understanding the difference between latent and active TB is crucial.
Latent TB Infection (LTBI): The bacteria are inactive. People show no symptoms and are not contagious. However, the bacteria can become active later.
Active TB Disease: The bacteria are multiplying, causing symptoms. If the infection is in the lungs or throat, it can be spread to others.
Consult Top Doctors for Personalised Advice
Debunking Common Tuberculosis Myths
Misinformation fuels fear and stigma. Here, we address the most persistent myths about TB.
Myth 1: TB is Incurable and Always Fatal
Historically, TB was often fatal, but medical advances have changed this reality.
The Fact: Effective Treatment is Available
TB is a curable disease. With proper medical care, most patients achieve a complete cure. Treatment involves taking special antibiotics for 6 to 9 months. Completing the full course is vital to kill all bacteria and prevent drug-resistant TB strains.
Myth 2: Everyone with TB is Highly Contagious
This misconception can lead to unnecessary social isolation.
The Fact: Understanding Contagious Periods
Only people with active pulmonary TB are contagious. Individuals with latent TB cannot spread the infection. Moreover, a person with active TB typically becomes non-contagious within weeks of starting effective treatment. Following the prescribed treatment is essential for both personal recovery and public health.
Myth 3: TB is a Disease of the Past
Some think TB is only a historical concern.
The Fact: TB's Global Impact Today
TB remains a major global health challenge. According to WHO, in 2022, 10.6 million people fell ill with TB, and 1.3 million died. Although incidence is lower in some countries, TB continues to affect millions worldwide.
Myth 4: TB is Hereditary/Runs in Families
Multiple cases in a family can give the false impression that TB is genetic.
The Fact: It's a Bacterial Infection, Not Genetic
TB is an infectious disease, not inherited. Family clustering occurs due to exposure to the same contagious person, not shared genes. Close, prolonged contact in poorly ventilated spaces increases risk.
Myth 5: TB Only Affects the Lungs
TB is often thought to be limited to pulmonary infection.
The Fact: Extrapulmonary Tuberculosis Exists
TB can affect other organs, including lymph nodes, bones, brain, kidneys, and spine. While not contagious, extrapulmonary TB requires specific treatment.
Myth 6: Positive Skin Test Means You're Contagious
A positive TB skin test or IGRA often causes concern.
The Fact: What a Positive Test Really Indicates
A positive test shows infection with TB bacteria but does not distinguish between latent and active TB. Further tests, like chest X-rays or sputum analysis, are needed to confirm active disease. Most people with a positive result have latent TB and are not sick or contagious.
The Facts: Symptoms, Diagnosis, and Treatment of TB
Accurate information about TB symptoms and management is key to early intervention.
Recognising the Symptoms of Active TB
Common symptoms include:
Cough lasting 3 weeks or more
Coughing up blood or sputum
Chest pain or discomfort when breathing or coughing
Unintentional weight loss
Fatigue, fever, night sweats, chills
Loss of appetite
If these symptoms persist, consult a doctor promptly. You can also seek an online consultation with Apollo24|7 for initial assessment and guidance.
How is Tuberculosis Diagnosed?
Diagnosis involves multiple steps:
Tuberculin Skin Test (TST) or IGRA Blood Test: Detects TB infection.
Chest X-ray: Identifies signs of active TB in the lungs.
Sputum Tests: Confirms TB bacteria presence in pulmonary TB. Apollo24|7 provides home collection services for relevant lab tests.
Get Your Health Checked
The Standard TB Treatment Regimen (DOTS)
The most effective TB treatment is DOTS (Directly Observed Therapy, Short-course). A healthcare worker supervises medication intake to ensure adherence. Treatment usually lasts 6-9 months and involves multiple antibiotics. Incomplete treatment is the main cause of drug-resistant TB.
Conclusion
Accurate knowledge about tuberculosis is crucial for both personal and public health. By debunking myths, we can promote early diagnosis, adherence to treatment, and a supportive environment for those affected. TB is neither a death sentence nor a source of shame—it is a treatable infection. If you experience symptoms or suspect exposure, seek professional advice without delay, including online consultation options such as Apollo24|7, to start timely treatment and protect yourself and others.
Consult Top Doctors for Personalised Advice
Consult Top Doctors for Personalised Advice

Dr. Sumara Maqbool
Pulmonology Respiratory Medicine Specialist
12 Years • MBBS, DNB Respiratory, critical care and sleep medicine, DrNB superspeciality Critical care, IDCCM, IFCCM, EDIC
Delhi
Apollo Hospitals Indraprastha, Delhi
(25+ Patients)

Dr Shubham Agarwal
Pulmonology Respiratory Medicine Specialist
4 Years • MBBS (Gold Medal) MD, DM (Pulmonary, Critical Care and Sleep Medicine), DNB (Medicine) , MRCP (UK), EDARM,
Lucknow
Apollomedics Super Speciality Hospital, Lucknow

Dr. Dawar Masud Rizavi
Pulmonology Respiratory Medicine Specialist
26 Years • MBBS, MD (Respiratory Diseases & TB) MRCP (London, UK)
Lucknow
Apollomedics Super Speciality Hospital, Lucknow

Dr. Bala Prakash
Pulmonology Respiratory Medicine Specialist
12 Years • MD
Chennai
Apollo Hospitals Greams Road, Chennai
(375+ Patients)

Dr. Battu Chaithanya
Pulmonology Respiratory Medicine Specialist
15 Years • DTCD, DNB( Respiratory diseases), DRCPC( Canada) Lung transplant fellowship, Toronto
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
(200+ Patients)
Get Your Health Checked
₹3229(₹8072)60% off
More articles from tuberculosis
Frequently Asked Questions
Q1. Can TB spread by sharing food or water?
No. TB is airborne and cannot spread through food, drinks, handshakes, or shared surfaces.
Q2. How can I prevent getting tuberculosis?
Avoid close contact with contagious individuals, ensure good ventilation, and consider the BCG vaccine where recommended. Latent TB can be treated preventively.
Q3. What is the main cause of drug-resistant TB?
Drug-resistant TB arises when antibiotics are misused, treatment is incomplete, or an unreliable drug supply is used.
Q4. Is there a vaccine for TB?
The BCG vaccine prevents severe TB forms in children but is less effective against adult pulmonary TB and can affect skin test results.
Q5. How long does TB treatment last?
Drug-susceptible TB requires at least 6 months of treatment. Drug-resistant TB may require 9-12 months or longer, with more complex regimens.