Tuberculosis (TB): Symptoms, Causes & Prevention
Clear guide to Tuberculosis symptoms, causes, testing, treatment, and TB prevention. Trusted tips to protect against this serious lung disease.

Written by Dr. M L Ezhilarasan
Reviewed by Dr. Shaik Abdul Kalam MD (Physician)
Last updated on 14th Jan, 2026

Introduction
Tuberculosis is a contagious infection that primarily targets the lungs, making it one of the most significant infectious diseases globally. Although many people associate it with the past, TB continues to affect millions every year. The encouraging news is that TB is both preventable and treatable when managed correctly. Understanding common Tuberculosis symptoms, how the infection spreads and the steps you can take to prevent transmission can significantly reduce your risk and help protect your community. Early awareness is crucial because TB responds best when diagnosed promptly, and learning how to minimise exposure remains a powerful tool in public health.Consult a Top General Practitioner for Personalised Advice
What Is Tuberculosis?
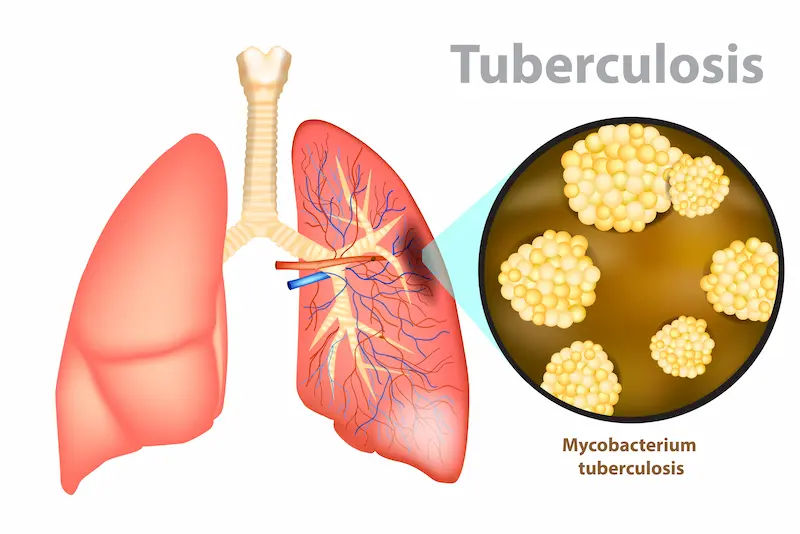
Tuberculosis is caused by Mycobacterium tuberculosis, a slow-growing bacterium that thrives in the lungs but is capable of affecting several other organs. People can develop either a non-contagious form that remains silent or the active form that causes illness and may spread to others.
Types Of TB-Related Conditions
The types of TB-related conditions
• TB usually affects the lungs but may occur in the spine, lymph nodes, kidneys, brain or other organs.
• Latent TB infection occurs when TB bacteria enter the body but remain inactive. There are no Tuberculosis symptoms, and people with latent TB cannot spread the infection.
• Active TB disease develops when bacteria multiply and cause illness. When active TB affects the lungs or throat, it becomes contagious and can spread through the air during coughing or even talking.
• TB does not spread through skin contact, shared utensils, touching surfaces, or exchanging everyday items such as towels or bedding.
Tuberculosis Symptoms: What To Watch?
Recognising Tuberculosis symptoms early is essential to accessing treatment promptly and preventing further spread. Active pulmonary TB, the most common form, typically presents with noticeable and persistent respiratory signs.
Common Pulmonary Symptoms
Common pulmonary symptoms include:
• A cough that lasts three weeks or longer
• Coughing up mucus or blood
• Chest pain or discomfort that worsens with breathing
• Fever or chills that fluctuate
• Night sweats that may soak bedding or clothing
• Tiredness or persistent weakness
• Loss of appetite accompanied by unintentional weight loss
Extrapulmonary Tuberculosis Symptoms
When TB affects areas outside the lungs, the symptoms vary according to the affected organ. These cases are not usually contagious but still require urgent medical care.
• Swollen, painful lymph nodes
• Back pain or joint discomfort when TB affects bones or the spine
• Persistent headaches, confusion or neck stiffness when TB infects the brain and its coverings
• Abdominal discomfort or urinary changes if the kidneys or urinary tract are involved
• Shortness of breath or fluid accumulation around the lungs
Anyone experiencing Tuberculosis symptoms, such as a persistent cough, fever or unexplained weight loss, should speak with a healthcare professional, especially if they have been exposed to someone with TB.
How TB Spreads (And How It Doesn’t)?
TB bacteria spread through tiny airborne droplets released when someone with infectious TB coughs, sneezes, shouts or sings. Inhaling these droplets can lead to infection, although this usually requires prolonged close contact.
How TB Spreads?
• Airborne droplets released during coughing
• Close indoor exposure in poorly ventilated environments
• Repeated contact over an extended period
How TB Does Not Spread?
TB may not spread by:
• Shaking hands or hugging
• Sharing food, drinks or eating utensils
• Touching doorknobs, toilet seats or other surfaces
The risk of infection increases when spending long periods in enclosed spaces with someone who is untreated and actively infectious.
Who Is At Higher Risk For TB?
Although anyone can become infected, certain factors increase susceptibility.
Higher-Risk Groups
• People living with or exposed to someone who has infectious TB
• Individuals born in or frequently travelling to regions where TB is common
• People in crowded or group-living environments, such as prison facilities or shelters
• Healthcare workers exposed to patients with TB
• People with weakened immune systems due to HIV, cancer, organ transplant medicines or immunosuppressive therapies
• Individuals with medical conditions such as diabetes, chronic kidney disease or silicosis
• People who use tobacco heavily or consume alcohol excessively
• Undernourished individuals
• Young children and older adults
Diagnosis of TB?
Diagnosing TB involves several steps, starting with tests for infection and progressing to tests that identify active disease.
Tests For TB Infection
• TB blood tests measure the immune response to TB proteins and help detect both latent and active infection.
• TB skin tests involve placing a small amount of testing material under the skin and assessing the area after 48 to 72 hours.
• Positive results indicate TB exposure but do not confirm active disease.
Tests For Active TB
It includes:
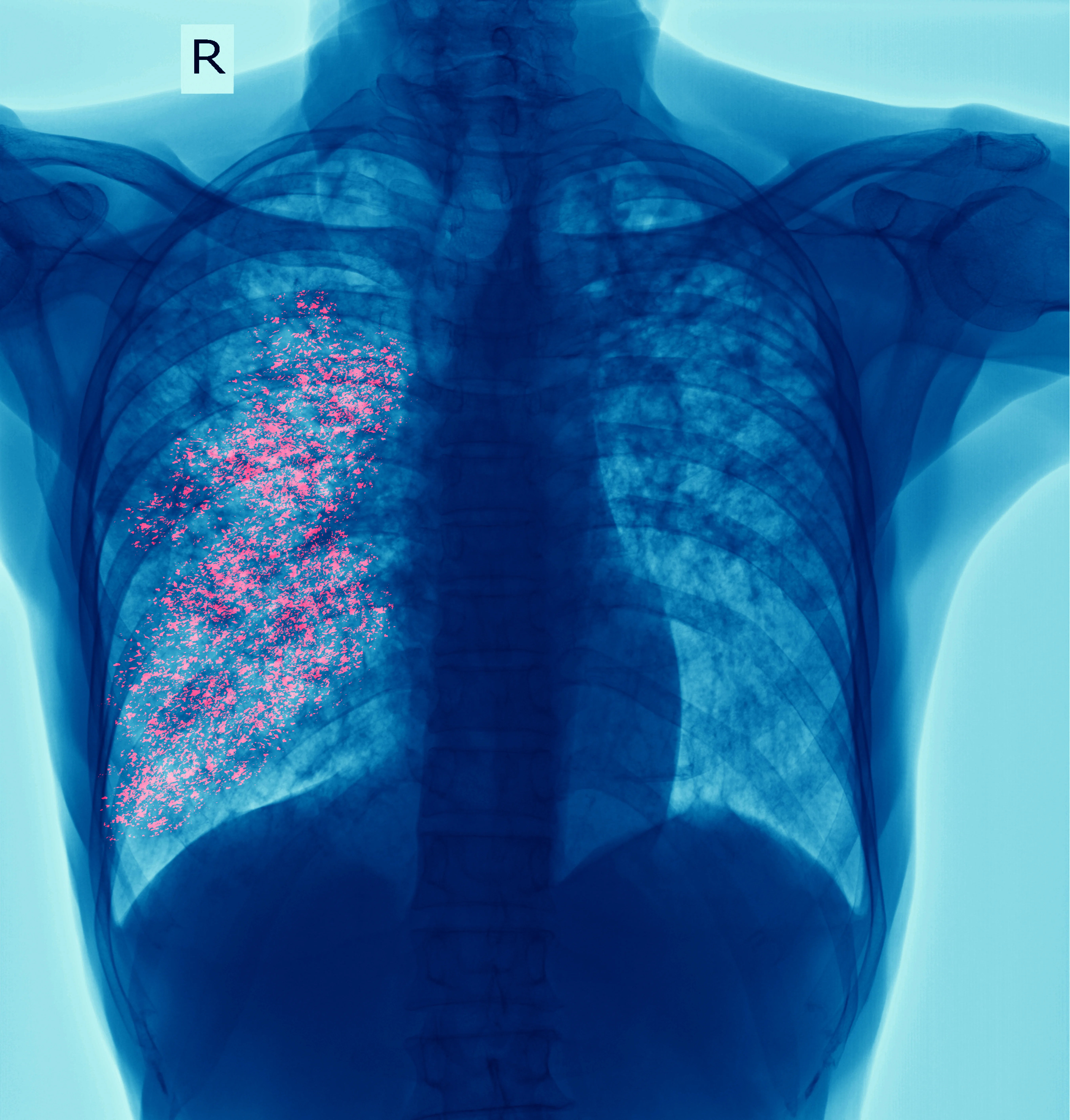
• Chest X-rays reveal lung abnormalities consistent with TB.
• Sputum tests examine mucus samples for TB bacteria under a microscope.
• Molecular tests detect TB DNA rapidly and identify certain drug resistance markers.
• Culture testing confirms TB and identifies which antibiotics are effective, although this method takes longer.
Additional Evaluations
• CT scans or targeted samples from affected areas for extrapulmonary TB
• HIV testing because co-existing HIV can affect treatment choices and outcomes
Treatment For TB: Is it Curable?
Treatment depends on whether a person has latent TB or active disease. Completing the full course of medication is essential to preventing drug resistance and ensuring full recovery.
Treatment For Latent TB Infection
The aim is to eliminate bacteria before they become active. Treatment options include:
• Short-course rifamycin regimens, such as three months of once-weekly isoniazid and rifapentine
• Four months of daily rifampicin
• Three months of daily isoniazid plus rifampicin
• Longer courses of isoniazid when other options are unsuitable
Clinicians tailor treatment based on age, medical conditions and interactions with other medications.
Treatment For Active TB Disease
Active TB requires multiple medicines taken for several months.
• The initial phase usually includes isoniazid, rifampicin, pyrazinamide and ethambutol.
• A continuation phase uses fewer medicines but must be completed fully.
• Many patients begin feeling better after a few weeks, but stopping early can result in relapse or resistance.
• People with lung TB may need to stay home initially to avoid spreading infection.
• Side effects such as vision changes, yellowing of the skin, abdominal pain or tingling in the limbs should be reported promptly.
• Rifampicin interacts with various medicines, including some HIV drugs, blood thinners and hormonal contraceptives, so reviewing all medicines with a clinician is crucial.
Drug-Resistant TB
Drug-resistant TB arises when bacteria stop responding to standard medicines. This form requires specialist treatment, often with a longer and more complex regimen. Despite the challenges, many people fully recover with appropriate support.
TB Practical Steps To Protect Yourself
Effective prevention combines environmental measures, personal habits and timely medical care.
Everyday Prevention
• Ensure good ventilation by opening windows and using fans
• Practise cough etiquette by covering the mouth and nose
• Wear masks or respirators in high-risk or healthcare environments
• Avoid spending long periods in poorly ventilated spaces with someone who may be infectious
Preventive Healthcare Measures
• Get tested if exposed or if belonging to a high-risk group
• Treat latent infection to prevent future illness
• Manage conditions such as HIV or diabetes with ongoing medical care
• Avoid smoking and heavy drinking to support lung health
• Maintain adequate nutrition for a strong immune system
Vaccination (BCG)
• The BCG vaccine offers significant protection for infants and young children against severe forms of TB
• It does not reliably prevent adult pulmonary TB
• Policies differ by country and depend on TB prevalence
How to Handle Active TB?
Ways to handle active TB:
• Encourage immediate treatment and support adherence
• Improve ventilation in shared spaces
• Follow guidance from public health teams regarding testing and temporary isolation
• Ensure young children, older adults and immunocompromised household members are evaluated
When to Seek Medical Help?
People should contact a clinician if they:
• Have a persistent cough lasting more than three weeks
• Experience night sweats, fever or unexplained weight loss
• Have been exposed to someone with active TB
• Test positive for TB infection
Urgent help is needed if:
• Breathing becomes difficult
• Large amounts of blood appear in the mucus
• Severe headaches, confusion or chest pain develop
Living Well With TB
Tips on living well with TB:
• Take medicines exactly as instructed and consider using reminders
• Attend all follow-up visits for monitoring and sputum tests
• Rest and eat well to support recovery
• Avoid alcohol while taking TB medicines
• Discuss family planning options if using rifampicin-related drugs
• Inform your clinician of all medicines and supplements.
Key Takeaways
1. Know the signs: Tuberculosis symptoms like a persistent cough, fever, night sweats, and weight loss need medical attention.
2. Get tested after exposure or if you’re at risk. Treat latent TB to prevent future illness.
3. Start treatment promptly if you have active TB and complete the full course.
4. Practice TB prevention: good ventilation, cough etiquette, masks in high-risk settings, and regular medical care for underlying conditions.
Consult a Top General Practitioner for Personalised Advice
Consult a Top General Practitioner for Personalised Advice

Dr. Debdatta Pati
Psychiatrist
18 Years • MBBS, DPM, MD (PSYCHIATRY)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr. Pinaki Mukhopadhyay
General Physician/ Internal Medicine Specialist
32 Years • MBBS
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
(25+ Patients)

Dr. Ashita Kuruvilla
General Physician/ Internal Medicine Specialist
7 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Sougata Kumar
General Practitioner
8 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Rupam Chowdhury
Orthopaedician
10 Years • MBBS, DNB (Ortho.)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
Consult a Top General Practitioner for Personalised Advice

Dr. Debdatta Pati
Psychiatrist
18 Years • MBBS, DPM, MD (PSYCHIATRY)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr. Pinaki Mukhopadhyay
General Physician/ Internal Medicine Specialist
32 Years • MBBS
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
(25+ Patients)

Dr. Ashita Kuruvilla
General Physician/ Internal Medicine Specialist
7 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Sougata Kumar
General Practitioner
8 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Rupam Chowdhury
Orthopaedician
10 Years • MBBS, DNB (Ortho.)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
More articles from tuberculosis
Frequently Asked Questions
1) Is TB curable?
Yes. With the right combination of antibiotics taken for the full prescribed time, most people with drug-susceptible TB are cured. Early diagnosis and consistent treatment are key.
2) How contagious is TB, and how long is someone infectious?
Untreated lung or throat TB can be contagious, especially with close, prolonged indoor contact. After starting effective treatment, most people become much less infectious within a few weeks. Your healthcare team will confirm when it’s safe to resume work, school, or social activities.
3) What’s the difference between latent TB and active TB?
A/Latent TB infection: You have TB bacteria in your body, but you feel well, have no symptoms, and can’t spread TB to others. Treatment reduces your future risk of getting sick.
Active TB disease: The bacteria are multiplying and causing illness. If it’s in your lungs or throat, you can spread TB to others. Treatment is needed to cure the infection and prevent transmission.
4) Can I catch TB from kissing, sharing utensils, or touching doorknobs?
TB spreads through the air when a person with infectious TB coughs, speaks, sings, or sneezes. It is not spread by shaking hands, sharing dishes or utensils, or touching surfaces. Risk is highest with close, prolonged indoor exposure to someone with untreated lung TB.
5) Does the BCG vaccine prevent TB in adults? Should I get it?
BCG helps protect infants and young children from severe forms of TB but does not reliably prevent adult lung TB. In countries with low TB rates, BCG is not routinely given. Ask your healthcare provider or local public health department about recommendations where you live.