Ways To Reduce Uric Acid Naturally With Home Remedies
Discover effective home remedies and diet tips to naturally lower uric acid levels and manage gout. Learn about hydration, low-purine foods, cherry juice, and more for joint health.

Written by Dr. Md Yusuf Shareef
Reviewed by Dr. Dhankecha Mayank Dineshbhai MBBS
Last updated on 13th Jan, 2026

Introduction
If you’ve ever experienced a sudden, throbbing pain in a joint—especially the big toe—uric acid might be the culprit. When uric acid levels get too high, crystals can build up in joints and tissues, leading to gout attacks, kidney stones, and long-term joint damage. The good news? You can often lower uric acid naturally with simple, practical home remedies and daily habits. In this guide, you’ll learn exactly what uric acid is, how it affects your body, and which foods, drinks, supplements, and lifestyle changes can help bring levels down. We’ll draw on evidence from trusted health sources and break everything into easy, actionable steps. You’ll also see where home treatments work best, when to get lab tests, and how to know it’s time to consult a doctor. If you’re ready to tackle uric acid without guesswork, keep reading—we’ll help you build a home plan that’s science-backed, budget-friendly, and realistic for everyday life.
Uric Acid Basics: What It Is, Why It Rises, and What It Feels Like
What is uric acid?
Uric acid is a waste product formed when your body breaks down purines—substances found naturally in your body and in many foods. Normally, uric acid dissolves in the blood, goes to the kidneys, and exits through urine. When production is too high or excretion too slow, uric acid builds up, a state called hyperuricemia.
How the body handles urate
About two-thirds of daily uric acid comes from your body’s own purine turnover; one-third is from diet . Kidneys excrete most uric acid; a small amount leaves via the gut. Genetics, kidney function, certain medications (like thiazide and loop diuretics), insulin resistance, and dehydration all affect this balance.
Symptoms of high uric acid
• Gout: sudden, intense joint pain (often big toe, but also ankle, knee), redness, swelling, and warmth, usually peaking within 24 hours.
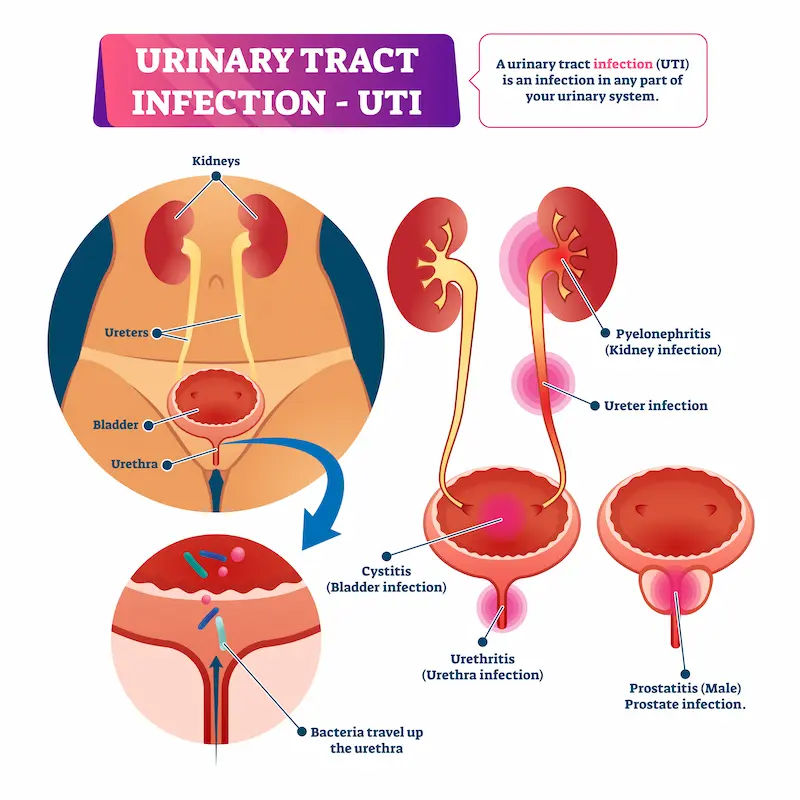
• Kidney stones: flank pain, blood in urine, nausea.
• Silent hyperuricemia: high levels without symptoms—still worth addressing, especially if you have risk factors (hypertension, CKD, obesity).
If symptoms persist beyond two weeks or you have recurrent flares, consult a doctor online with Apollo 24|7 for further evaluation.
Consult a Top General Physician
Diet and Uric Acid: From Purines to Fructose
Purine-rich foods
Not all purines are equal. High-purine animal foods (organ meats like liver; anchovies, sardines, mackerel; and large portions of red meat) raise uric acid and gout risk . Plant purines (like in lentils or spinach) appear less problematic and are generally safe in moderation because they come with fiber and phytonutrients that improve insulin sensitivity and uric acid excretion .
Fructose and sugary drinks
Fructose metabolism generates uric acid rapidly. Sugary sodas, energy drinks, and fruit juices sweetened with high-fructose corn syrup can spike levels and trigger gout flares . Even 100% fruit juice can raise uric acid if consumed in large amounts. Whole fruits are different; their fiber slows absorption and is generally protective when eaten in normal portions .
Alcohol: beer, spirits, and wine
Alcohol reduces uric acid excretion and adds purines (especially beer). Beer and spirits are associated with higher gout risk; wine appears less problematic in small amounts but can still trigger flares for some people. If you drink, limit to no more than one drink daily (women) or two (men), and avoid alcohol during or near a flare.
Practical plate example:
• - Half the plate: colorful vegetables (broccoli, peppers, leafy greens)
• - Quarter: whole grains (brown rice, oats, quinoa)
• - Quarter: lean proteins (skinless poultry, eggs, tofu, or small portions of fish like salmon or trout)
• - Plus: a serving of low-fat yogurt or milk for added benefit
Hydration Strategies That Help Lower Uric Acid
Water is your friend. Uric acid leaves the body mainly through urine; staying well-hydrated can improve excretion and reduce gout flare risk . Aim for pale-yellow urine as a simple daily check.
• Target intake: For most adults, 2–3 liters per day total fluids (more if you live in hot climates, sweat heavily, or exercise). People with heart or kidney disease should follow clinician guidance.
• Water vs. other beverages:
• Best choices: plain water, mineral water, herbal teas, and coffee/tea (unsweetened) in moderation .
• Be cautious: sugary drinks, fruit juices, and sports drinks can raise uric acid due to fructose .
• Alcohol dehydrates; avoid during flares.
• Hydration timing matters: Sip throughout the day. Have a glass of water with each meal and one between meals. Before bed, a small glass helps, especially if you tend to wake dehydrated (unless on fluid restriction).
Unique tip: Add a “water anchor”—like pairing a glass with routine tasks (check email, after bathroom breaks)—to reliably hit your intake goal without counting every sip.
Evidence-Backed Home Remedies (What to Add to Your Diet)
Cherries and tart cherry juice
Observational research found that cherry consumption was associated with a 35% lower risk of gout attacks over a 2-day period; pairing cherries with allopurinol lowered risk even further . Tart cherry juice may reduce inflammation and modestly lower uric acid in some small trials. Try:
• 1–2 cups fresh cherries (or ~1/2–1 cup frozen) daily during high-risk periods; or
• 240–480 ml tart cherry juice daily (unsweetened or lightly sweetened), monitoring total sugar.
Vitamin C–rich foods
A meta-analysis shows vitamin C supplementation can modestly reduce uric acid (about 0.3–0.5 mg/dL for many people), though it’s not a standalone treatment for gout [10]. Food-first approach:
• Citrus (oranges, grapefruit), kiwi, strawberries, bell peppers, broccoli.
• If using supplements, 500 mg/day can be considered, but check with your doctor if you have kidney stones or are on specific medications [10].
Low-fat dairy and coffee
• Low-fat dairy may promote uric acid excretion and reduce gout risk.
• Coffee consumption has been associated with lower uric acid and reduced gout risk, potentially via improved insulin sensitivity and increased uric acid excretion. Keep it unsweetened; limit to 2–3 cups daily if tolerated and avoid if it worsens reflux, anxiety, or sleep.
Fiber and whole foods
High-fiber foods improve insulin sensitivity and help stabilize uric acid over time. Think oats, barley, legumes, apples, leafy greens, and nuts in modest portions. Long-tail terms to know: low purine vegetables, anti-inflammatory diet for gout.
Herbs and Supplements: What Works, What Doesn’t
Quercetin and bromelain
• Quercetin (a flavonoid found in onions, apples) has small studies suggesting a modest uric acid–lowering effect, likely by inhibiting xanthine oxidase (the enzyme that produces uric acid). Doses in research vary (e.g., 500 mg/day). Evidence is not definitive; safety is generally good but can interact with some antibiotics and blood thinners.
• Bromelain (from pineapple) is more known for anti-inflammatory effects than direct urate lowering. It may help joint comfort for some but evidence for uric acid reduction is limited.
Omega-3, turmeric, and ginger
• Omega-3 fats (e.g., 1–2 g EPA+DHA daily from fish oil) may reduce inflammation and cardiovascular risk, which is relevant because gout often coexists with metabolic issues. They don’t directly lower uric acid but may reduce flare intensity.
• Turmeric (curcumin) and ginger offer anti-inflammatory benefits; they may help symptom control but don’t replace urate-lowering strategies. Choose standardized extracts; discuss with your clinician if you take blood thinners or have gallbladder issues.
Celery seed, nettle, apple cider vinegar—evidence check
• Celery seed and nettle teas are traditional diuretics; robust trials for uric acid lowering are lacking. They may mildly increase urine output; ensure adequate hydration and monitor for interactions (celery seed can interact with anticoagulants; nettle may affect blood pressure meds).
• Apple cider vinegar doesn’t have strong evidence for lowering uric acid. It may aid glucose control slightly for some, but can damage teeth and irritate the stomach. If you use it, dilute well and avoid if you have reflux.
Safety and interactions
Natural doesn’t mean risk-free. Always:
• Start one change at a time and monitor for reactions.
• Avoid combining multiple new supplements at once.
• If you take medications (blood thinners, diabetes meds, BP meds), are pregnant, or have kidney disease, discuss supplements with your doctor first.
• If your condition does not improve after trying these methods, book a physical visit to a doctor with Apollo 24|7.
Lifestyle Changes That Lower Uric Acid
Weight loss—how fast is safe?
Gradual weight loss improves insulin sensitivity and lowers uric acid . Aim for 0.5–1% body weight/week. Extreme low-calorie diets or fasting can temporarily raise uric acid and precipitate flares—avoid crash diets. Focus on:
• Protein at each meal (eggs, yogurt, tofu, poultry)
• Fiber-rich carbs (vegetables, whole grains, legumes)
• Healthy fats (olive oil, nuts, seeds)
• Balanced portions and mindful eating
Movement, stress, and sleep
• Exercise: 150 minutes/week moderate cardio + 2 sessions of strength training improves metabolic health and helps control uric acid indirectly. Choose low-impact activities during flares (cycling, swimming).
• Stress: Chronic stress and poor sleep can worsen inflammation and lifestyle choices. Try brief daily routines—10 minutes of breathing, stretches, or a short walk after dinner.
• Sleep: 7–9 hours supports hormone balance and weight control. Sleep apnea is linked with gout; if you snore or feel unrefreshed, seek evaluation.
Unique insight: Micro-habits add up. A 10-minute walk after meals improves glucose handling and may reduce uric acid over time by improving insulin sensitivity. If you can’t overhaul your lifestyle overnight, stack micro changes across the day.
Foods to Limit or Avoid (and Smart Swaps)
High-purine animal foods
• Limit: organ meats (liver, kidney), sardines, anchovies, mackerel, herring, large portions of red meat.
• Swap: eggs, skinless chicken, tofu, tempeh, or small portions of salmon/trout.
Sugary drinks and juices
• Limit or avoid: sodas, energy drinks, sweetened iced tea, large glasses of fruit juice.
• Swap: sparkling water with lemon, unsweetened herbal iced teas, diluted juice (1 part juice to 3–4 parts water).
Alcohol choices
• Limit: beer and spirits; avoid during flares.
• If you drink: consider small amounts of wine with meals and hydrate well. Some individuals are sensitive even to wine—track your own response.
Portion guide:
• Meat/fish: 85–100 g cooked (about a deck of cards), 2–3 times per week if you’re prone to gout.
• Dairy: 1–2 servings low-fat per day (e.g., yogurt, milk).
• Legumes: 2–4 times per week are generally fine for most people with gout when portions are moderate, due to overall health benefits .
H2: Monitoring, Targets, and Lab Tests
Ideal urate levels
• General target: serum uric acid below 6 mg/dL (360 µmol/L) for most; below 5 mg/dL (300 µmol/L) if you have tophi or severe gout, as advised by your doctor .
• Check frequency: If you’re making lifestyle changes, retest in 8–12 weeks to assess impact. If on medication, follow your doctor’s schedule.
Testing options
• Laboratory serum uric acid test is the standard. Apollo 24|7 offers convenient home collection for tests like serum uric acid, kidney function, or related metabolic labs.
• Keep a simple tracking log: date, uric acid value, weight, average fluids/day, alcohol intake, and any flares. Patterns help guide adjustments.
When to repeat tests
• Stable and symptom-free: every 6–12 months.
• After significant diet/lifestyle changes: 8–12 weeks.
• On medication changes: as directed by your clinician.
When to See a Doctor and Medication Options?
Treating gout flares
During an acute flare, anti-inflammatory treatment is the priority:
• NSAIDs, colchicine, or short courses of steroids are common options .
• Rest the joint, apply ice, elevate, and stay hydrated.
• Do not start or stop long-term urate-lowering medication during a flare unless directed.
Long-term urate lowering
If you have recurrent flares, tophi, kidney stones, or very high uric acid, medication is often needed:
• Allopurinol and febuxostat reduce uric acid production; probenecid increases excretion (less common if kidney function is reduced). Your doctor will tailor therapy to your profile .
• Lifestyle changes still matter—they reduce flare triggers and improve overall health.
Red flags and care access
• Seek medical care if you have a fever with joint pain, severe swelling not improving, or new kidney stone symptoms.
• If symptoms persist beyond two weeks, consult a doctor online with Apollo 24|7 for further evaluation, treatment, or referrals.
Special Situations: Tailoring Your Plan
Kidney disease and stones
Reduced kidney function raises uric acid. Avoid dehydration, be careful with high-protein fad diets, and review all supplements with your doctor. For uric acid kidney stones, alkalinizing urine (e.g., with potassium citrate, if prescribed) and hydration are key.
Diabetes, hypertension, and diuretics
Insulin resistance elevates uric acid. Improving glucose control and weight helps. Some blood pressure medications (like losartan) may lower uric acid, while thiazides can raise it—your doctor can adjust therapy accordingly.
Women, pregnancy, and menopause
Premenopausal women have lower uric acid on average; levels may rise after menopause. In pregnancy or when trying to conceive, avoid most supplements and discuss any herbal remedies with your obstetrician.
Conclusion
Lowering uric acid naturally doesn’t require a perfect diet or a shelf full of supplements. It comes down to a few consistent habits: drink enough water, favor whole foods and low-fat dairy, cut back on sugary drinks and alcohol, and move your body regularly. Add targeted choices like cherries and vitamin C–rich produce for an extra edge, and consider coffee if you tolerate it. If you’re dealing with recurrent gout flares or your uric acid remains high despite best efforts, don’t wait—combine lifestyle changes with medical care for the best results. Track your lab values and symptoms to see what works, and adjust gradually. For convenient testing, Apollo 24|7 offers home collection services for serum uric acid and related labs, and if your symptoms persist or you need a personalized plan, you can consult a doctor online with Apollo 24|7. With a clear plan and steady steps, most people can bring uric acid levels into a safer range and get back to living—and moving—comfortably.
Consult a Top General Physician
Consult a Top General Physician

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Santanu Mandal
General Physician/ Internal Medicine Specialist
18 Years • MD (Physician), DNB (General Medicine)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
(25+ Patients)

Dr. Sajid Samiullah Siraj
General Physician/ Internal Medicine Specialist
2 Years • MBBS
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru

Dr. Swagato Podder
General Practitioner
5 Years • MBBS
Kolkata
GRD POLYCLINIC, Kolkata

Dr. Arif Ahmed
General Physician/ Internal Medicine Specialist
9 Years • MBBS, MD (Genl. Med.)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
Consult a Top General Physician

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Santanu Mandal
General Physician/ Internal Medicine Specialist
18 Years • MD (Physician), DNB (General Medicine)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
(25+ Patients)

Dr. Sajid Samiullah Siraj
General Physician/ Internal Medicine Specialist
2 Years • MBBS
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru

Dr. Swagato Podder
General Practitioner
5 Years • MBBS
Kolkata
GRD POLYCLINIC, Kolkata

Dr. Arif Ahmed
General Physician/ Internal Medicine Specialist
9 Years • MBBS, MD (Genl. Med.)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
More articles from Urinary Tract Infections
Frequently Asked Questions
Q1: What is the fastest way to reduce uric acid at home?
Increase water intake, avoid alcohol and sugary drinks immediately, and focus on low-purine meals (vegetables, whole grains, low-fat dairy). These steps can support uric acid excretion within days, though full effects on serum urate often take weeks.
Q2: Do bananas, apples, or oats increase uric acid?
No—these are generally safe. Oats and apples provide fiber that can help metabolic health. Bananas are moderate in fructose; enjoy in normal portions as part of a balanced, low purine diet plan.
Q3: Can lemon water reduce uric acid?
Lemon water can support hydration and may slightly increase urine pH, which might help with uric acid excretion. It’s not a standalone cure, but it’s a good hydration choice for many people.
Q4: Is chicken okay for gout?
Yes, in moderate portions. Choose skinless poultry and limit to ~85–100 g cooked per serving, a few times per week, alongside plenty of vegetables and whole grains.
Q5: How long do home remedies take to work for high uric acid?
You may feel fewer triggers within 1–2 weeks (especially with hydration and dietary shifts), but measurable changes in serum uric acid are best checked after 8–12 weeks. If levels remain high, discuss medication options with a doctor.