Hormonal Changes and Urological Health: A Complete Guide
Explore how hormonal changes impact urological health, including common issues, prevention tips, and strategies to maintain a healthy urinary system.

Written by Dr. Mohammed Kamran
Reviewed by Dr. D Bhanu Prakash MBBS, AFIH, Advanced certificate in critical care medicine, Fellowship in critical care medicine
Last updated on 13th Jan, 2026

Introduction
Have you ever wondered why bladder issues seem to crop up during major life transitions like pregnancy, menopause, or even midlife for men? The answer often lies not just in your bladder, but in your bloodstream. Hormonal changes are a natural part of life, yet their profound impact on urological health is frequently overlooked. From regulating tissue strength and elasticity to controlling the urge to urinate, hormones are the silent conductors of your urinary system. This guide will demystify the intricate link between your endocrine and urinary systems. We'll explore how fluctuations in key hormones like oestrogen and testosterone can lead to conditions like incontinence, frequent UTIs, and prostate enlargement. More importantly, we'll provide actionable strategies, from lifestyle adjustments to knowing when to consult a professional to help you navigate these changes confidently and maintain optimal wellness at every stage of life. Understanding this connection is the first step toward taking back control of your urological health.
The Hormone-Urology Connection: Why They're Inseparable
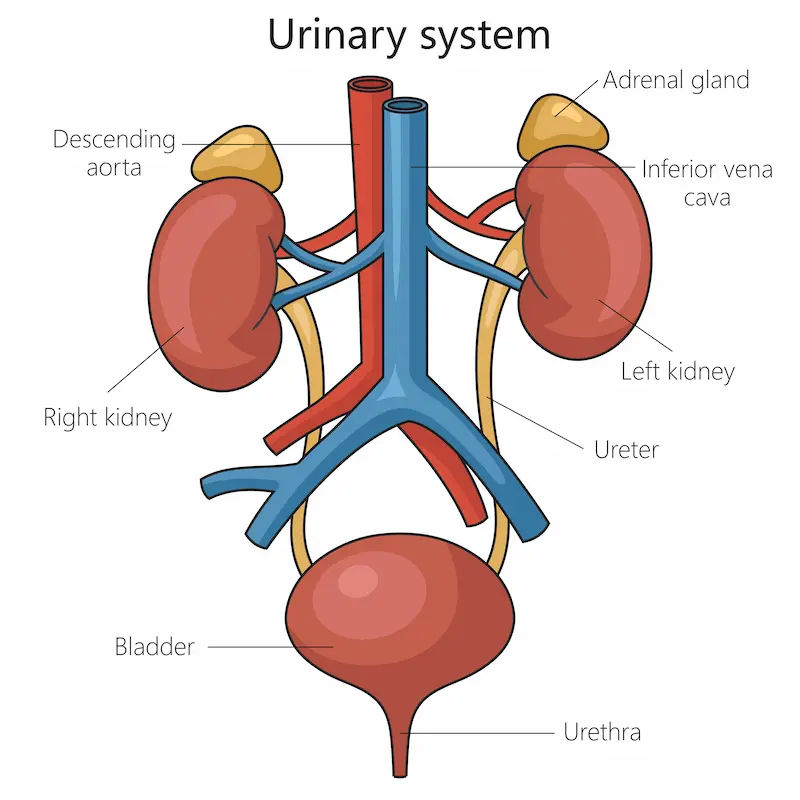
Your urinary system, comprising the kidneys, ureters, bladder, and urethra, is far from a simple plumbing system. Its tissues are rich with hormone receptors, making them highly responsive to your body's chemical messengers. When hormone levels are balanced, the system functions smoothly. But when hormonal changes occur, it can directly affect muscle tone, blood flow, and the integrity of the lining in the urethra and bladder.
Key Hormones Governing Your Urinary System
Hormones play a crucial role in keeping your urinary system functioning smoothly.
Oestrogen: The Guardian of Female Urological Tissues
Oestrogen is crucial for maintaining the health of the female urinary tract. It promotes blood flow, keeps tissues thick, moist, and elastic, and supports the friendly bacteria that protect against infection. When oestrogen levels drop most notably during menopause, the urethral and vaginal tissues can become thin, dry, and weak (a condition known as genitourinary syndrome of menopause, or GSM). This can lead to a host of issues, including increased susceptibility to UTIs, urgency, and stress incontinence.
Testosterone: More Than a Male Sex Hormone
While testosterone is synonymous with male characteristics, it plays a vital role in urological health for all genders. In men, it influences prostate size and function. It also helps maintain muscle mass, including the pelvic floor muscles that support bladder control. Low testosterone levels can contribute to decreased pelvic muscle strength and may be linked to an overactive bladder. Furthermore, testosterone is a precursor to oestrogen, even in men, and this balance is critical for overall tissue health.
The Supporting Cast: Cortisol, Progesterone, and Thyroid
• Cortisol: Chronic stress elevates cortisol, which can suppress immune function, potentially increasing the risk of urinary tract infections. High cortisol can also disrupt sleep patterns, exacerbating issues like nocturia (waking up at night to urinate).
• Progesterone: This hormone, which rises and falls during the menstrual cycle and pregnancy, can relax smooth muscle tissue, including the bladder, sometimes leading to temporary incontinence.
• Thyroid Hormones: Both hyperthyroidism and hypothyroidism can affect kidney function and urinary output, influencing frequency and urgency.
Consult a Urologist for the best advice
Hormonal Shifts in Women and Urological Impact
Women experience more dramatic and cyclical hormonal changes throughout their lives, making their urological health particularly vulnerable to these shifts.
Pregnancy and Childbirth: The First Major Shift
During pregnancy, soaring levels of progesterone relax the bladder muscles, while the growing uterus places direct pressure on the bladder. This often leads to stress incontinence (leaking when coughing or sneezing) and urgency. Childbirth can further stretch and weaken the pelvic floor muscles, compounding these issues. While many symptoms resolve postpartum, some can persist, highlighting the need for pelvic floor rehabilitation.
Perimenopause and Menopause: Navigating the Change
The perimenopausal and menopausal transition marks the most significant hormonal change for urological health. The decline in oestrogen directly causes the thinning of the urethral lining and weakening of the pelvic floor. A study published in Menopause Review notes that nearly 50% of postmenopausal women report experiencing some form of urinary incontinence. The risk of recurrent UTIs also increases significantly due to changes in the vaginal microbiome and tissue integrity.
Common Conditions: Stress Incontinence, UTIs, and Vaginal Atrophy
The culmination of these changes often manifests as:
• Stress Incontinence: Leakage of urine during physical activity.
• Urge Incontinence: A sudden, intense urge to urinate followed by involuntary leakage.
• Recurrent UTIs: Caused by anatomical changes and loss of protective bacteria.
• Vaginal Atrophy (GSM): Leading to dryness, irritation, and painful urination.
Hormonal Changes in Men: Beyond the Prostate
Men experience a more gradual hormonal shift, but it is no less significant for urological health.
Andropause (Male Menopause): The Gradual Decline
Andropause refers to the age-related decline in testosterone, typically starting around age 40-50. While not as abrupt as female menopause, this decline can affect muscle mass, energy, and, crucially, pelvic floor strength. This can contribute to male urinary incontinence, especially after prostate surgery, but also as a primary condition.
Benign Prostatic Hyperplasia (BPH): The Testosterone Connection
BPH, or prostate enlargement, is extremely common in aging men. It's not high testosterone itself that causes BPH, but the conversion of testosterone to dihydrotestosterone (DHT). DHT stimulates prostate growth, which can squeeze the urethra and cause symptoms like weak urine stream, dribbling, frequent urination (especially at night), and a feeling of incomplete emptying.
Low Testosterone and Its Impact on Bladder Function
Emerging research suggests a link between low testosterone and overactive bladder (OAB) symptoms in men. Testosterone helps maintain the health of nerves and muscles involved in urination. A deficiency may lead to increased bladder sensitivity and contractions, causing urgency and frequency. If you're experiencing these symptoms alongside low energy or low libido, it's worth discussing with a doctor.
Lifestyle Strategies to Support Urological Health Through Change
While you can't stop hormonal changes, you can powerfully influence how your body responds to them.
Dietary Choices for a Healthy Bladder
• Stay Hydrated: Contrary to instinct, drinking less water concentrates urine, irritating the bladder. Aim for 6-8 glasses daily.
• Limit Irritants: Caffeine, alcohol, artificial sweeteners, and spicy foods can aggravate an overactive bladder.
• Focus on Fiber: Constipation puts pressure on the bladder. A diet rich in fruits, vegetables, and whole grains helps prevent this.
The Power of Pelvic Floor Exercises (Kegels for All!)
Pelvic floor exercises are not just for women! Both genders can benefit immensely. Strong pelvic muscles provide better support for the bladder and urethra, reducing incontinence. A physical therapist can ensure you're performing them correctly for maximum benefit.
Stress Management and Quality Sleep
Chronic stress worsens urinary symptoms. Practices like yoga, meditation, and deep breathing can help manage stress levels. Prioritising sleep is also critical, as poor sleep can disrupt hormone regulation further.
When to Seek Professional Help
Lifestyle changes are a great first step, but some situations require medical expertise. If symptoms like incontinence, frequent urination, or pain during urination persist beyond two weeks and interfere with your quality of life, consult a doctor online with Apollo24|7 for further evaluation.
Medical Interventions: From HRT to Minimally Invasive Procedures
A urologist or endocrinologist can offer solutions tailored to your needs:
• Hormone Replacement Therapy (HRT): Topical vaginal oestrogen is highly effective and safe for treating GSM and reducing UTI risk in women. Systemic HRT or testosterone replacement therapy for men are options that require careful discussion of benefits and risks.
• Medications: Drugs can relax the prostate (for BPH) or calm an overactive bladder.
• Minimally Invasive Procedures: For stress incontinence, procedures like slings can provide significant relief. For BPH, treatments like Rezum or UroLift can reduce obstruction without major surgery.
• Diagnostic Tests: If lab tests are needed, Apollo24|7 offers convenient home collection for tests like PSA (Prostate-Specific Antigen) or routine urine analysis.
Get Your Health Assessed
Conclusion
Navigating the ebbs and flows of our hormones is a universal human experience, and its impact on urological health is profound yet manageable. By understanding the connection between hormonal changes and the function of your bladder and urinary system, you move from a place of frustration to one of empowerment. Whether you're a woman navigating perimenopause or a man concerned about prostate health, remember that proactive steps, from strengthening your pelvic floor to making mindful dietary choices, can make a world of difference. Most importantly, never dismiss persistent symptoms as "just getting older." Your quality of life is paramount. Armed with knowledge and the right support, you can maintain excellent urological health through every season of life.
Consult a Urologist for the best advice
Consult a Urologist for the best advice

Dr. Pavan Kumar S K
Urologist
11 Years • MBBS, MS , Mch( Urology) DNB (Urology)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Pradeep Champawat
Urologist
10 Years • MBBS, MS, DNB Urology
Delhi
Apollo Hospitals Indraprastha, Delhi
(175+ Patients)

Dr. Sudhakar G V
Urologist
25 Years • MBBS, MS(Gen.Surgery), DNB Urology
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Ramesh H
Urologist
16 Years • MBBS, MS , Mch( Urology)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Prabir Basu
Urologist
19 Years • MBBS, MS General Surgery, DNB Genito-Urinary Surgery
Jodhpur Park
Dr. Prabir Basu urology clinic, Jodhpur Park
(200+ Patients)
Consult a Urologist for the best advice

Dr. Pavan Kumar S K
Urologist
11 Years • MBBS, MS , Mch( Urology) DNB (Urology)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Pradeep Champawat
Urologist
10 Years • MBBS, MS, DNB Urology
Delhi
Apollo Hospitals Indraprastha, Delhi
(175+ Patients)

Dr. Sudhakar G V
Urologist
25 Years • MBBS, MS(Gen.Surgery), DNB Urology
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Ramesh H
Urologist
16 Years • MBBS, MS , Mch( Urology)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Prabir Basu
Urologist
19 Years • MBBS, MS General Surgery, DNB Genito-Urinary Surgery
Jodhpur Park
Dr. Prabir Basu urology clinic, Jodhpur Park
(200+ Patients)
More articles from Urology Consultation
Frequently Asked Questions
1. Can hormonal imbalances cause UTIs in young women?
Yes, absolutely. While often linked to sexual activity, hormonal fluctuations during the menstrual cycle can temporarily alter the pH and bacterial environment in the vagina and urethra, increasing susceptibility to UTIs in some women.
2. Is frequent urination at night a sign of hormonal changes?
Yes, nocturia can be a sign. In men, it's a classic symptom of BPH driven by hormonal shifts. In women, declining oestrogen can contribute to bladder overactivity. However, it can also indicate other issues like sleep apnea or diabetes, so it's important to get it checked.
3. What are the first signs of urological issues related to menopause?
Often, the first signs are increased frequency of urination, a feeling of urgency, and stress incontinence (leaking when laughing, coughing, or exercising). You might also notice increased discomfort or recurrent UTIs.
4. Can improving my diet really help with overactive bladder caused by hormones?
Yes, dietary changes can significantly reduce irritation. Bladder irritants like caffeine and alcohol can exaggerate the symptoms caused by underlying hormonal changes. Eliminating them often brings noticeable relief.
5. Are there natural alternatives to hormone therapy for urological health?
Some people find relief with phytoestrogens (like those in soy) for menopausal symptoms, and pelvic floor physical therapy is a highly effective, non-hormonal treatment for incontinence. However, the efficacy varies, and it's essential to discuss these options with your doctor to create a safe, personalised plan.