Diabetes Management
Juvenile Diabetes: Early Signs to Watch out For
4 min read
By Apollo 24/7, Published on - 09 July 2021, Updated on - 11 December 2023
Share this article
0
0 like

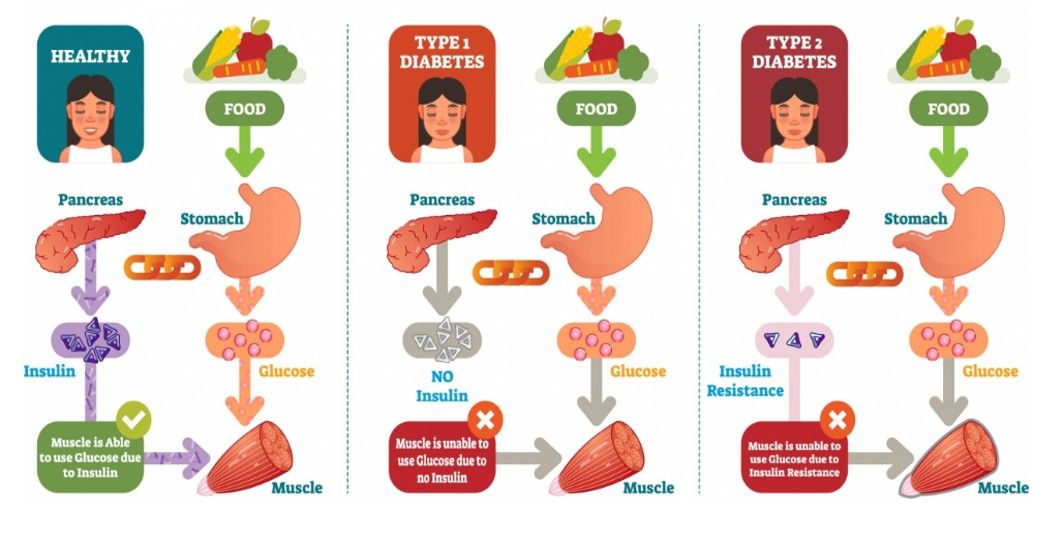
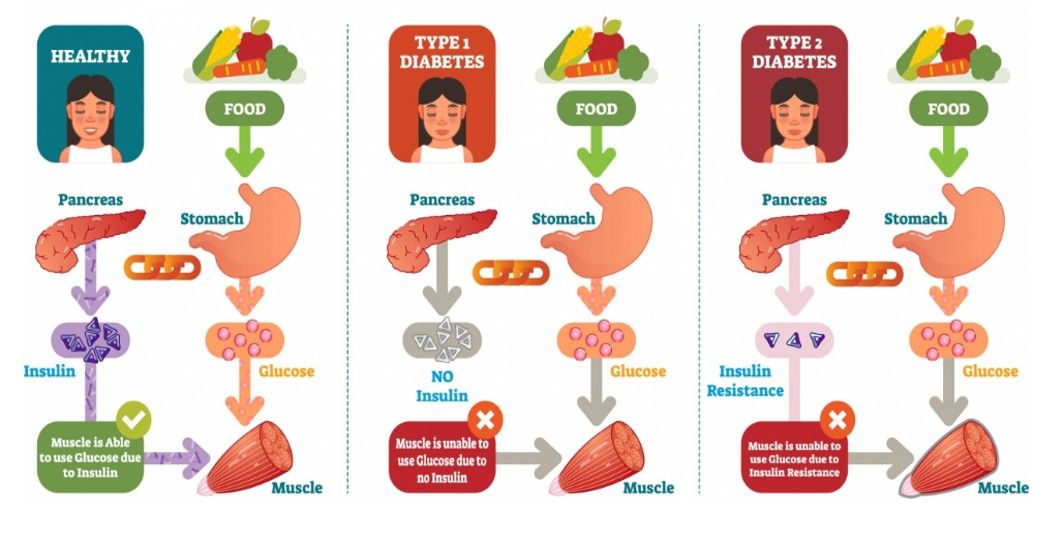
The human body needs insulin, a hormone produced in the pancreas, to help blood sugar or glucose enter the cells and produce energy. When the pancreas makes very little or no insulin, the glucose builds up in the bloodstream resulting in type 1 diabetes. Statistics reveal that around 90% of the cases of type 1 diabetes are reported in children and people younger than 25 years of age.
Juvenile diabetes is a term previously used to describe type 1 diabetes in children and young people, characterized by an abnormal increase in the blood sugar levels of the body. Children suffering from juvenile diabetes need a regular supply of artificial insulin as the absence of insulin can be life-threatening for them. Therefore, it is extremely important to identify the early signs of diabetes in children to prevent any such consequences.
What causes juvenile diabetes?
The exact cause of juvenile diabetes is not entirely known yet. However, the possible reasons for type 1 diabetes in children include:
- Genes: Those who have a family history of type 1 diabetes are at high risk of developing the same.
- Autoimmune disorder: The body’s immune system gets hyperactivated and damages the insulin-producing beta cells in the pancreas, resulting in type 1 diabetes.
- Environmental trigger: Exposure to a virus can also trigger type 1 diabetes in some people.
Also read:
Can Diabetic People Consume Low Calorie Sweeteners?
What are the early signs of juvenile diabetes?
The signs of juvenile diabetes often appear suddenly and may vary in every child. However, some of the common early signs include:
- Dehydration and excessive thirst (polydipsia): Due to the improper functioning of the kidneys, excess glucose and other fluids are released into the urine. This causes dehydration, making the person feel thirsty all the time.
- Frequent urination (polyuria): Usually, when the kidney filters blood to make urine, it reabsorbs all the sugar and returns it to the bloodstream. However, due to abnormally high blood glucose levels, all the sugar does not get reabsorbed. This extra sugar pulls more water from the surrounding tissues, resulting in higher volumes of urine.
- Extreme hunger (polyphagia): Despite having increased blood glucose levels, the cells cannot absorb the glucose either due to lack of insulin or insulin resistance. Since there is not enough glucose, the body does not have energy and hence, the person feels hungry all the time.
- Persistent fatigue: Inability to turn the glucose into energy can result in constant tiredness.
- Vision disturbances: High blood sugar levels can result in blurred vision, cataracts, and other vision problems.
- Fruity smelling breath: Due to excess sugar in the blood, ketone bodies (molecules formed in the absence of enough insulin) start depositing in the body, resulting in a breath that smells fruity or acetone-like.
- Yeast infection: High blood sugar allows yeast to overgrow especially in the vaginal region.
- Gastrointestinal symptoms: Diabetes prevents quick digestion of food, causing it to stay in the stomach for long. This can lead to nausea and abdominal pain. Excess build-up of ketone bodies can also result in nausea and vomiting.
- Mood change: Fluctuations in blood sugar levels can result in irritability, mood swings, and restlessness.
- Delayed healing: Diabetes can slow down the healing of cuts, grazes or wounds.
A child exhibiting any of these symptoms must be taken to a doctor for further examination. Apart from understanding the patient’s medical history, the doctors would prescribe blood tests such as fasting and random plasma glucose test to measure the amount of blood sugar. A urine test is also prescribed to identify sugar and ketone bodies in the urine sample.
To know more about diabetes and its effects in children, consult our expert Diabetologists.
Can juvenile diabetes be treated?
There is no cure for juvenile diabetes. However, the child’s quality of life can be improved if the parents are well educated about the condition and the treatment options. Parents or caregivers of the child affected by the condition must ensure to:
- Administer insulin through injections or pumps regularly to maintain the blood sugar levels.
- Include healthy foods such as fruits, vegetables, whole grains, and low-fat dairy products in the diet.
- Encourage children to take up moderate-intensity exercises such as brisk walking, swimming or riding a bicycle in the daily routine.
- Monitor the blood sugar levels twice daily using a glucometer to prevent hypoglycemia (extremely low blood sugar).
Conclusion
Juvenile diabetes is a long-term condition that can start at any age. There's no cure for type 1 diabetes in children, but it can be managed by appropriate medical care. The child requires daily insulin delivery and regular glucose monitoring to maintain blood sugar levels. Parents need to stay in contact with their child’s health care team to understand the treatment plan and other management measures.
For any diabetes-related query, you can speak with a diabetologist.
You can also try the Apollo 24|7 Diabetes Self-Management Tool to log your sugar values, track patterns, know all about food nutrition and more.
Diabetes Management
Leave Comment
Recommended for you
.jpg?tr=q-80)
Diabetes Management
Corn and Diabetes: Best Ways to Consume & Nutritional Breakdown
Can corn be part of a diabetic diet? Yes, certainly! Corn has valuable nutrients and can be consumed safely by individuals with diabetes when paired wisely with proteins and healthy fats. However, like all foods, it's about portion control and balance. For personalised guidance on managing diabetes through dietary choices, consider joining the Apollo Super 6 programme.
Diabetes Management
Understanding the Different Types of Diabetes
In a world where diabetes is increasingly common, understanding the different types can be crucial for early detection, effective management, and prevention of complications. Whether it's type 1, type 2, gestational, or even rare forms such as monogenic and secondary diabetes, each has its own causes and management strategies. Keep in mind that maintaining a healthy lifestyle is key to managing all forms of diabetes.

Diabetes Management
The Impact of Gestational Diabetes on the Baby's Health
Gestational diabetes, a high blood sugar condition that develops during pregnancy, can potentially impact your baby's health in various ways. From an increased birth weight to the risk of obesity and type 2 diabetes, understanding these possible effects can help in managing this condition.
Subscribe
Sign up for our free Health Library Daily Newsletter
Get doctor-approved health tips, news, and more.
Visual Stories

8 Fruits That are Incredibly Healthy for Diabetes
Tap to continue exploring
Recommended for you
.jpg?tr=q-80)
Diabetes Management
Corn and Diabetes: Best Ways to Consume & Nutritional Breakdown
Can corn be part of a diabetic diet? Yes, certainly! Corn has valuable nutrients and can be consumed safely by individuals with diabetes when paired wisely with proteins and healthy fats. However, like all foods, it's about portion control and balance. For personalised guidance on managing diabetes through dietary choices, consider joining the Apollo Super 6 programme.
Diabetes Management
Understanding the Different Types of Diabetes
In a world where diabetes is increasingly common, understanding the different types can be crucial for early detection, effective management, and prevention of complications. Whether it's type 1, type 2, gestational, or even rare forms such as monogenic and secondary diabetes, each has its own causes and management strategies. Keep in mind that maintaining a healthy lifestyle is key to managing all forms of diabetes.

Diabetes Management
The Impact of Gestational Diabetes on the Baby's Health
Gestational diabetes, a high blood sugar condition that develops during pregnancy, can potentially impact your baby's health in various ways. From an increased birth weight to the risk of obesity and type 2 diabetes, understanding these possible effects can help in managing this condition.