Your Guide to Endobronchial Ultrasound (EBUS): A Minimally Invasive Lung Diagnosis
Discover how Endobronchial Ultrasound (EBUS) helps diagnose and stage lung diseases. Learn the procedure, benefits, risks, and what to expect during recovery.

Written by Dr. Rohinipriyanka Pondugula
Reviewed by Dr. Md Yusuf Shareef MBBS
Last updated on 8th Sep, 2025

Navigating a potential lung condition can be daunting, especially when your doctor starts talking about tests and biopsies. If you or a loved one has been recommended an Endobronchial Ultrasound, commonly known as EBUS, it's natural to have questions. This advanced, minimally invasive procedure has revolutionised how pulmonologists diagnose and stage lung diseases, particularly lung cancer. Unlike traditional surgical methods, EBUS offers a highly accurate way to access hard-to-reach areas around the lungs with fewer risks and a faster recovery. This guide will walk you through everything you need to know about EBUS—from how it works and why it's used, to what you can expect during and after the procedure. Our goal is to empower you with clear, understandable information so you can approach your healthcare journey with confidence.
What is an Endobronchial Ultrasound (EBUS)?
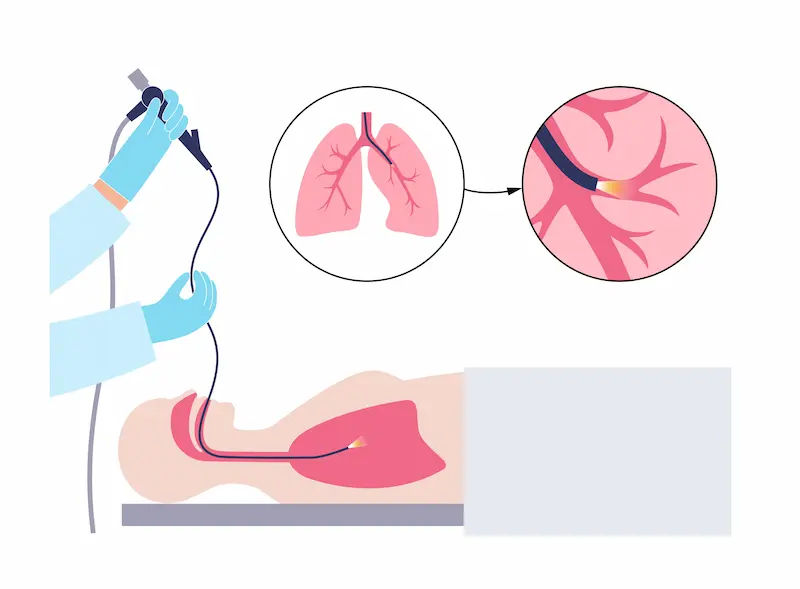
Endobronchial Ultrasound (EBUS) is a specialised procedure that allows a pulmonologist to see inside your airways and the surrounding areas of your lungs and chest. It combines two key technologies: a flexible bronchoscope (a thin, lighted tube) and an ultrasound probe attached to its tip. Think of it as giving your doctor "X-ray vision" to see through the airway walls and safely guide a needle to take tissue samples from lymph nodes or lung masses without major surgery.
How Does EBUS Work? The Technology Explained
The magic of EBUS lies in the ultrasound component. While a standard bronchoscope can only see the inner lining of your airways, the ultrasound probe emits sound waves that penetrate the airway walls. These waves bounce back off tissues and structures, creating a real-time, detailed image on a monitor. This allows the doctor to visualise blood vessels, lymph nodes, and masses that are outside the airways but within the mediastinum (the central area of the chest between the lungs). This precise imaging is crucial for performing a transbronchial needle aspiration (TBNA), where a small needle is passed through the bronchoscope to collect cell samples from these targeted areas.
EBUS vs. Traditional Bronchoscopy: What's the Difference?
A traditional bronchoscopy is like using a flashlight to look inside a room through the keyhole. You can see the walls and furniture immediately inside. EBUS bronchoscopy, on the other hand, is like using that same keyhole but with a sophisticated radar that maps out the entire house's interior layout, including the contents of adjacent rooms. The key difference is the ability to see and biopsy structures outside the airway. This makes EBUS far more powerful for diagnosing conditions that affect the lymph nodes in the chest, which are often the first place lung cancer spreads.
Why is an EBUS Procedure Performed? Key Uses and Indications
Doctors recommend an EBUS for specific reasons, primarily centred on obtaining tissue diagnosis from areas that were previously only accessible through surgery.
Diagnosing Lung Cancer and Other Lung Conditions
The most common reason for an EBUS is to investigate suspicious lung masses or enlarged lymph nodes seen on a CT scan. By obtaining a tissue sample (biopsy), doctors can provide a definitive diagnosis of lung cancer, determine its specific type (e.g., adenocarcinoma, squamous cell carcinoma), and run genetic tests to guide targeted therapy. EBUS is also highly effective in diagnosing other conditions like sarcoidosis, tuberculosis, and other infections or inflammatory diseases that cause lymph node enlargement.
Staging Lung Cancer: The Role of Lymph Node Biopsy
Staging is the process of determining if and how far lung cancer has spread, which is the single most important factor in determining prognosis and treatment. The lymph nodes in the mediastinum are a critical gateway. EBUS for lung cancer staging is the gold-standard minimally invasive method to check these nodes for cancer cells (a process called N-staging). Accurate staging with EBUS helps decide whether a patient is a candidate for curative surgery or if other treatments like chemotherapy or radiation are needed first.
Evaluating Other Mediastinal Abnormalities
Sometimes, imaging scans reveal unexplained masses or enlarged lymph nodes in the mediastinum that are not necessarily related to the lungs. EBUS provides a safe pathway to sample these abnormalities and determine their cause, which could range from lymphoma to benign cysts.
What to Expect: The EBUS Procedure Step-by-Step
Knowing what will happen can significantly ease pre-procedure anxiety. Here’s a breakdown of the typical EBUS journey.
Before the Procedure: Preparation and Pre-Op
Your medical team will give you specific instructions. This usually includes fasting (no food or water) for 6-8 hours before the procedure to prevent aspiration. You’ll discuss your medical history, allergies, and current medications with your doctor. It's crucial to inform them if you are on blood thinners. You may undergo some pre-operative tests, such as blood work or an ECG. You will need someone to drive you home afterwards, as you will not be allowed to drive due to the sedatives.
During the Procedure: Anaesthesia and the Process
The procedure is performed in an endoscopy suite. You will be connected to monitors to track your heart rate, blood pressure, and oxygen levels. You will receive sedation through an IV line, which will make you very sleepy and comfortable (conscious sedation), or in some cases, general anaesthesia. A local anaesthetic spray will be used to numb your throat. The doctor will then gently insert the EBUS bronchoscope through your mouth or nose and down into your airways. You will be able to breathe normally throughout.
The Biopsy: How Tissue Samples are Collected
Once the scope is in position, the doctor will use the ultrasound image to locate the target lymph node or mass. They will carefully guide a tiny needle through the airway wall directly into the target. The syringe attached to the needle is used to suction out cell samples. This may be repeated several times to ensure an adequate sample is collected for the pathologist to analyse. The real-time ultrasound imaging ensures the needle avoids major blood vessels, making the procedure very safe.
After the Procedure: Recovery and Immediate Aftercare
After the EBUS, you will be monitored in a recovery area for 1-2 hours. The numbness in your throat will wear off in about an hour. It's common to have a sore throat, a hoarse voice, or a minor cough for a day or two. You might cough up a small amount of blood-tinged saliva, which is normal. You will be advised not to eat or drink until the throat numbness is completely gone to prevent choking. Most people can resume normal activities the next day.
Understanding Your EBUS Results and Next Steps
The tissue samples collected are sent to a pathology lab for analysis. This process can take several days. Your doctor will schedule a follow-up appointment to discuss the results with you. The findings will determine the definitive diagnosis and the next steps in your treatment plan. If the EBUS biopsy confirms cancer, the results will also include its type and stage, which will guide discussions about surgery, oncology, or radiation therapy.
Benefits and Advantages of Choosing EBUS
EBUS offers significant benefits over traditional surgical techniques like mediastinoscopy:
- Minimally Invasive: No surgical incisions; access is through the natural airway.
- High Accuracy: Boasts a diagnostic accuracy of over 90% for lymph node staging.
- Safer Profile: Lower risk of complications compared to surgery.
- Faster Recovery: Usually performed as an outpatient procedure, allowing you to go home the same day.
- Cost-Effective: Avoids the costs associated with operating rooms and longer hospital stays.
Potential Risks and Complications of EBUS
EBUS is considered very safe, but like any medical procedure, it carries some risks. These are rare but can include:
Bleeding from the biopsy site (usually minimal and self-limiting).
- Infection.
- A hoarse voice.
- In very rare cases, a puncture of the airway or a pneumothorax (collapsed lung) may require a chest tube.
- Your medical team is trained to prevent and manage these complications effectively.
Conclusion
Endobronchial Ultrasound (EBUS) represents a major leap forward in pulmonary medicine, offering a precise, powerful, and patient-friendly approach to diagnosing serious lung conditions. By providing a clear window into the mediastinum and enabling safe biopsies, it eliminates the need for more invasive surgeries in many cases, reducing patient discomfort and speeding up recovery. If your doctor has suggested an EBUS, it is because it is the most effective way to get the answers needed to formulate the right treatment plan for you. Armed with knowledge, you can now approach this procedure with greater understanding and confidence. Always remember that open communication with your healthcare team is key. If you have further questions about your symptoms or a recent scan, consulting a pulmonologist is the best next step. You can book a physical visit to a specialist with Apollo24|7 to get a personalised evaluation and discuss whether EBUS is the right diagnostic tool for your situation.
Consult a Specialist for the best advice
Consult a Specialist for the best advice

Dr. Syed Ismail Ali
General Practitioner
7 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr. M L Ezhilarasan
General Practitioner
6 Years • MBBS
Visakhapatnam
Apollo 24|7 Clinic - Andhra Pradesh, Visakhapatnam

Dr D M Karthik
General Practitioner
4 Years • MBBS, Fellowship in Diabetes Mellitus, Advance certificate in Diabetes Mellitus, Derma Nutrition Certification
Visakhapatnam
Apollo 24|7 Clinic - Andhra Pradesh, Visakhapatnam

Dr. Suraja Nutulapati
General Physician/ Internal Medicine Specialist
10 Years • MBBS, MD (Internal Medicine)
Hyderabad
Apollo 24|7 Clinic, Hyderabad
(975+ Patients)

Dr. Mohammed Kamran
General Practitioner
5 Years • MBBS, FIDM
Nashik
Apollo 24|7 Clinic - Maharashtra, Nashik
Frequently Asked Questions
Is the EBUS procedure painful?
No, you should not feel pain during the procedure. You will be under sedation, which makes you sleepy and relaxed, and your throat will be numbed with a local anaesthetic. Most patients remember very little of the procedure itself. Some minor throat discomfort afterwards is common.
How long does an EBUS procedure take?
The procedure itself typically takes between 30 to 60 minutes. However, you should plan to be at the hospital or procedure centre for several hours to account for preparation before and recovery time afterwards.
How accurate is EBUS for lung cancer diagnosis?
EBUS is highly accurate, with studies showing a sensitivity and diagnostic yield often exceeding 90-95% for sampling mediastinal lymph nodes. This makes it an extremely reliable tool for diagnosis and staging.
What is the difference between EBUS and a mediastinoscopy?
Both are used to biopsy mediastinal lymph nodes, but the approach is vastly different. Mediastinoscopy requires a surgical incision at the base of the neck and general anaesthesia in an operating room. EBUS is performed through the mouth with a scope, requires no incision, and uses lighter sedation. EBUS has largely replaced mediastinoscopy for most patients due to its minimally invasive nature.
When should I call my doctor after an EBUS?
While rare, contact your doctor or seek immediate medical attention if you experience severe shortness of breath, cough up more than a few tablespoons of blood, develop a fever over 101°F (38.3°C), or have severe chest pain.