Guide to Know About Endobronchial Ultrasound Ebus Radial Probe
Know about the endobronchial ultrasound radial probe(ebus), what it is, how it works, and the step-by-step process, radial ebus and linear ebus, application, benefits, advantages and more.

Written by Dr. Rohinipriyanka Pondugula
Reviewed by Dr. M L Ezhilarasan MBBS
Last updated on 23rd Sep, 2025

Introduction
Navigating a lung cancer diagnosis or a mysterious spot on a chest X-ray can be overwhelming. You might hear about biopsies and scopes, and the terminology can feel like a foreign language. One of the most significant advancements in pulmonary medicine is Endobronchial Ultrasound, or EBUS. While many are familiar with the linear EBUS probe for lymph node biopsies, its cousin, the radial probe endobronchial ultrasound, plays a uniquely crucial role. This guide is designed to demystify the EBUS radial probe. We will break down what it is, how it works, and why it's a game-changer for diagnosing peripheral lung lesions that were once difficult to reach without invasive surgery. You'll learn about the procedure itself, what to expect, and how this technology is improving diagnostic accuracy and patient outcomes in modern pulmonology.
What is an Endobronchial Ultrasound (EBUS) Radial Probe?
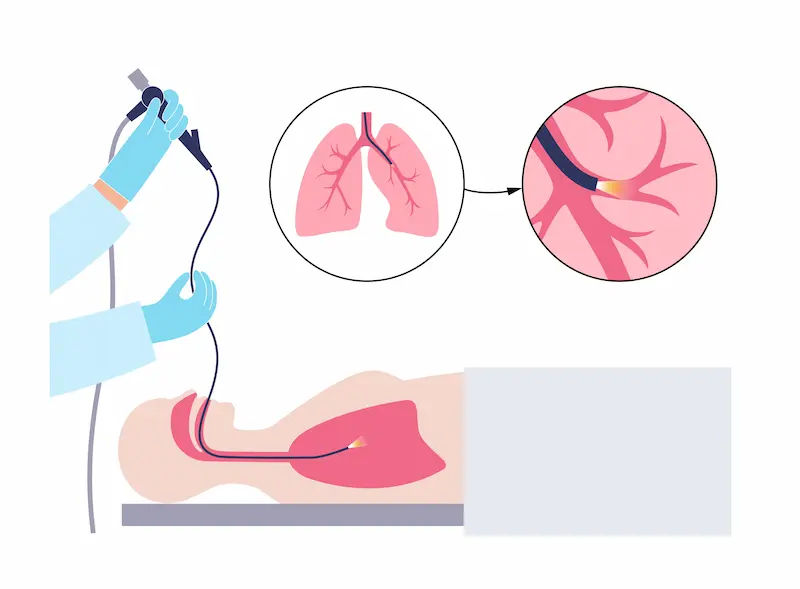
The endobronchial ultrasound radial probe is a specialised medical tool used by pulmonologists (lung doctors). Imagine a miniature ultrasound camera, less than 2mm in diameter, attached to a long, flexible catheter. This probe is inserted through the working channel of a standard bronchoscope—a thin, lighted tube passed through the mouth or nose into the lungs.
Unlike the linear EBUS probe, which looks sideways to biopsy lymph nodes, the radial probe provides a complete 360-degree ultrasound view perpendicular to the airway. When inflated with a small water-filled balloon, it offers a stunningly detailed, real-time image of the layers of the airway wall and the structures immediately surrounding it, such as blood vessels and lung nodules. This allows the physician to "see" through the airway wall, transforming the bronchial passages into a navigable roadmap.
Consult an Oncologist for Personalised Advice
How Does the Radial EBUS Procedure Work?
Understanding the step-by-step process can alleviate much of the anxiety associated with the procedure.
Pre-Procedure Preparation
Before the EBUS bronchoscopy, you will be asked to fast for several hours. Your medical team will review your history, current medications, and any allergies. You will receive sedation through an IV line, which makes you relaxed and drowsy but still able to breathe on your own—this is often called "twilight sedation."
Step-by-Step Process During the Procedure
The procedure process includes:
- Insertion: The pulmonologist gently guides the bronchoscope through your mouth and into your airways.
- Navigation: Using the bronchoscope's camera, they navigate through the complex bronchial tree toward the area of concern identified on your CT scan.
- Probe Deployment: The ultra-thin radial probe is then advanced through the scope's channel and into the smaller, peripheral airways that the scope itself cannot enter.
- Ultrasound Imaging: The probe is activated, sending out ultrasound waves. The returning echoes create a real-time, circular image on a monitor. The physician looks for the distinctive "blizzard sign" or a hyperechoic (bright white) circle that indicates the presence of a lung nodule.
- Guiding the Biopsy: Once the nodule is located and its position relative to the airway is confirmed, the probe is
removed. The physician then guides biopsy tools (like forceps or needles) through the same path to the exact spot to take tissue samples. - Sample Collection: Several samples are collected and sent to a pathology lab for analysis.
Post-Procedure and Recovery
The procedure typically takes 30-60 minutes. You will be monitored in a recovery area until the sedation wears off. You may have a mild sore throat or cough, but most people can go home the same day. You will need someone to drive you and are advised to rest for the remainder of the day.
Radial EBUS vs. Linear EBUS: Understanding the Key Differences
It's crucial to distinguish between the two types of EBUS, as they serve different purposes.
In short, Radial EBUS is for finding and diagnosing the lung tumour itself, especially small ones. Linear EBUS is for
determining if and where the cancer has spread to nearby lymph nodes. Sometimes, both procedures are performed in the same session for comprehensive diagnosis and staging.
Key Applications and Uses of Radial EBUS
The radial endobronchial ultrasound technique is invaluable for several clinical scenarios:
- Diagnosing Peripheral Pulmonary Nodules: This is its flagship application. It allows for precise sampling of nodules as small as 1-2 cm, which are often discovered incidentally on CT scans.
- Guiding Transbronchial Lung Biopsy: It dramatically increases the safety and yield of these biopsies by confirming the location of the biopsy tools within the lesion and away from major blood vessels.
- Staging Lung Cancer: While linear EBUS is the gold standard for nodal staging, radial EBUS can help determine if a tumour has directly invaded the airway wall or adjacent structures (T-staging).
- Assessing Airway Invasion: It can help evaluate whether cancers from nearby organs (like the oesophagus) are invading the airway.
- Planning for Intervention: The detailed anatomical view helps plan procedures like airway stenting or tumour
debulking.
Benefits and Advantages of Choosing Radial EBUS
Opting for a radial probe EBUS biopsy offers significant benefits over other diagnostic methods:
- Minimally Invasive: Avoids the need for surgical procedures like VATS (Video-Assisted Thoracic Surgery) or CT-
guided needle biopsy, which carry higher risks of pneumothorax (collapsed lung). - High Diagnostic Yield: Studies show it can achieve a diagnostic yield of over 70-80% for peripheral lesions, a
substantial improvement over fluoroscopy-guided bronchoscopy. - Excellent Safety Profile: The risk of major complications, such as significant bleeding or pneumothorax, is very low (typically <1-2%).
- Real-Time Imaging: Provides live feedback, allowing for immediate adjustment and confirmation of tool placement.
- Access to Difficult Areas: Can reach nodules in the lung's outer regions that are inaccessible to other non-surgical techniques.
Potential Risks and Limitations
No medical procedure is without risk, though they are rare with radial EBUS.
- Bleeding: Minor bleeding at the biopsy site is common and usually self-resolving. Significant bleeding is very
uncommon. - Pneumothorax: There is a small risk of air leaking from the lung, causing it to collapse. This may require a chest tube, but the incidence is lower than with CT-guided biopsy.
- Infection: As with any procedure, there is a minimal risk of infection.
- Sedation-Related Risks: Reactions to sedation medications are possible but are closely monitored by the anaesthesia team.
- Limitations: The success rate can be lower for very small nodules (<2cm), those without a clear "airway leading to them" (CT bronchus sign), or in certain locations. If your nodule is particularly challenging to reach, your
pulmonologist will discuss all diagnostic options with you, which may include a consultation with a thoracic surgeon.
What to Expect: Before, During, and After Your Procedure
Preparing for Your EBUS
You will receive specific instructions from your healthcare team. This will include fasting for 6-8 hours before the
procedure. Inform them of all medications, especially blood thinners (like aspirin, warfarin, clopidogrel), as you may
need to adjust these beforehand. Arrange for someone to drive you home and stay with you for the first evening.
The Day of the Procedure
You'll check in at the hospital or outpatient centre. An IV will be placed for fluids and sedation. The pulmonologist and anesthesiologist will meet with you to answer any last-minute questions. You'll then be taken to the procedure room, where monitoring equipment will be attached.
Recovery and Follow-Up
After the procedure, you'll wake up in a recovery room. Nurses will monitor your vital signs. Once you are fully awake and can swallow safely, you may be given ice chips or clear fluids. Your doctor will often provide a preliminary update, but the final pathology results take several days. A follow-up appointment will be crucial to discuss the biopsy results and the next steps in your care plan. If you're awaiting results, Apollo24|7 offers a convenient platform to book follow-up consultations online with specialists to review your reports and plan the way forward.
The Future of Navigational Bronchoscopy: Radial EBUS and Beyond
Radial EBUS is a cornerstone of modern interventional pulmonology, but technology continues to evolve. It is now often combined with other advanced techniques like:
Electromagnetic Navigational Bronchoscopy (ENB): This acts like a "GPS for the lungs," using CT scan data to create a 3D map and guide the bronchoscope to the target. Radial EBUS is then used for final confirmation before biopsy.
Robotic Bronchoscopy: New robotic systems offer unparalleled stability and reach into the deepest parts of the lung, again often using radial EBUS for confirmation.
These combined approaches, often called "multi-modal navigation," are pushing diagnostic yields for peripheral nodules above 90%, making surgery solely for diagnosis a thing of the past for most patients.
Conclusion
The endobronchial ultrasound radial probe represents a monumental leap forward in pulmonary medicine. It has transformed the diagnosis of lung nodules from a process that often required invasive surgery into a safe, outpatient, minimally invasive procedure. By providing a real-time ultrasound view from inside the airways, it allows pulmonologists to navigate with unprecedented precision, leading to earlier and more accurate diagnoses. This ultimately means better outcomes and more treatment options for patients. If you or a loved one has been recommended for a bronchoscopy to investigate a lung spot, understanding the role of radial EBUS can empower you to have informed discussions with your healthcare team about the best path forward.
Consult an Oncologist for Personalised Advice
Consult an Oncologist for Personalised Advice

Dr. Prof. Vijay Agarwal
Medical Oncologist
20 Years • MBBS, MD, MRCP (UK), PhD (UK), CCT (UK) Medical Oncology
Bengaluru
Apollo Hospitals Bannerghatta Road, Bengaluru

Dr. Tarun Jindal
Uro Oncologist
14 Years • MS (AIIMS, New Delhi), MCh (Gold Medalist), Fellow, VUI, Henry Ford Hospital, Detroit, USA; Robotic and Laparoscopic surgeon
Kolkata
Apollo Multispeciality Hospitals , Kolkata, Kolkata
(150+ Patients)

Dr Shaikat Gupta Director Surgical Onco
Surgical Oncologist
35 Years • MBBS (University Gold Medalist), MS, FRCSEd
Kolkata
Apollo Multispeciality Hospitals , Kolkata, Kolkata
(100+ Patients)

Dr. Ruquaya Ahmad Mir
Surgical Oncologist
20 Years • MBBS, DNB
Delhi
Apollo Hospitals Indraprastha, Delhi
(25+ Patients)

Dr Devashish Tripathi
Radiation Specialist Oncologist
20 Years • MBBS, PLAB, MRCP (UK)- General Medicine, FRCR (Oncology), Certificate of Completion of Training (CCT)- Clinical Oncology
Delhi
Apollo Hospitals Indraprastha, Delhi
Consult an Oncologist for Personalised Advice

Dr. Prof. Vijay Agarwal
Medical Oncologist
20 Years • MBBS, MD, MRCP (UK), PhD (UK), CCT (UK) Medical Oncology
Bengaluru
Apollo Hospitals Bannerghatta Road, Bengaluru

Dr. Tarun Jindal
Uro Oncologist
14 Years • MS (AIIMS, New Delhi), MCh (Gold Medalist), Fellow, VUI, Henry Ford Hospital, Detroit, USA; Robotic and Laparoscopic surgeon
Kolkata
Apollo Multispeciality Hospitals , Kolkata, Kolkata
(150+ Patients)

Dr Shaikat Gupta Director Surgical Onco
Surgical Oncologist
35 Years • MBBS (University Gold Medalist), MS, FRCSEd
Kolkata
Apollo Multispeciality Hospitals , Kolkata, Kolkata
(100+ Patients)

Dr. Ruquaya Ahmad Mir
Surgical Oncologist
20 Years • MBBS, DNB
Delhi
Apollo Hospitals Indraprastha, Delhi
(25+ Patients)

Dr Devashish Tripathi
Radiation Specialist Oncologist
20 Years • MBBS, PLAB, MRCP (UK)- General Medicine, FRCR (Oncology), Certificate of Completion of Training (CCT)- Clinical Oncology
Delhi
Apollo Hospitals Indraprastha, Delhi
Frequently Asked Questions
1. Is radial EBUS painful?
No, the procedure is not painful. You will be under sedation or general anaesthesia to ensure you are comfortable and feel no discomfort. The most common sensation afterwards is a mild sore throat.
2. How accurate is radial EBUS in diagnosing lung cancer?
The accuracy, or diagnostic yield, is high, especially when combined with navigation technology. For nodules larger than 2cm with a clear airway leading to them, the yield can be 80% or higher. The accuracy can be lower for smaller or harder-to-reach nodules.
3. What is the difference between a radial EBUS and a CT-guided needle biopsy?
CT-guided biopsy is performed by a radiologist who uses CT imaging to insert a needle through the chest wall to the nodule. It has a high yield but carries a higher risk of pneumothorax (collapsed lung). Radial EBUS is performed through the natural airway by a pulmonologist, avoiding puncturing the lung lining, which significantly reduces the pneumothorax risk.
4. How long does it take to get biopsy results from an EBUS procedure?
The initial pathology report may be available within 2-3 working days. However, more specialised testing (e.g., molecular testing for targeted cancer therapy) can take up to two weeks. Your doctor will give you a timeline for when to expect results.
5. Can radial EBUS be used to treat conditions, or is it only for diagnosis?
Currently, the radial probe is primarily a diagnostic tool. However, by accurately diagnosing and staging a condition it directly informs and guides the treatment plan, which may involve other therapeutic procedures.