- male
- 65 Years
- 29/01/2025
I'm a bit concerned about my dadhe's got a history of paroxysmal atrial fibrillation. His reports show no blockage and his echo report is normal, but his blood tests indicate an iron and magnesium deficiency. We've started him on Orofer XT for the iron since his Hb level is 10.3 because of low ferritin. I've seen some folks online saying that magnesium citrate 1000 mg per day and L-Taurine have helped reduce their Afib episodes. Is it okay for my dad to take these supplements too, and if so, for how long should he be on them? Also, he's currently taking Cordarone (Amiodarone), Prolomet 25, and Xarelto 15. We're wondering if he could switch from Amiodarone to Flecanide (Flecarite 50) since we've heard Cordarone can be quite toxic compared to other meds. Would love to hear your thoughts on this.
Answered by 1 Apollo Doctors
Q1. Can my father take magnesium citrate and L-Taurine supplements to help reduce Afib episodes? If yes, for how long? Yes, your father can take magnesium citrate and L-Taurine supplements to help reduce Afib episodes. He can take magnesium citrate 1000 mg per day and L-Taurine supplements as reported by other patients. It is recommended to continue taking these supplements as long as they are providing benefit in reducing Afib episodes. Q2. Can my father switch from Cordarone (amiodarone) to FlecanideFlecarite 50, since Cordarone is very toxic compared to other medicines? Yes, your father can consider switching from Cordarone (amiodarone) to FlecanideFlecarite 50 as an alternative treatment for paroxysmal atrial fibrillation. It is important to consult with your father's healthcare provider to discuss the potential benefits and risks of switching medications. The healthcare provider can provide guidance on the appropriate dosage and duration of treatment with FlecanideFlecarite 50 based on your father's individual health condition.
Dr. Ibrahim Suggests...
Consult a Cardiologist
Answered 04/07/2025
0
0

More Cardiology Health Queries
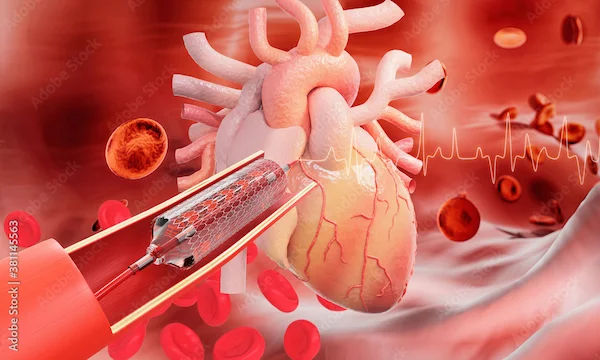
View allmy 65 year old mom is very weak and one doctor recommended a pacemaker followed by stents but others are saying bypass surgery is the only option what are the pros and cons of each approach which would be safer for someone in her condition
pros are reduced chest pain,lowered risk of heart attack restoration of blood flow.Cons include infection,bleeding,delirium,arrhythmias.
Answered by 1 Apollo Doctors
I've been feeling this sharp pain around my heart and now it's getting really tough to breathe. What could be causing this, and should I be worried?
take tablet zerodol for 3 days
Answered by 1 Apollo Doctors
I'm 35 and recently got some blood work done. My LDL is at 123, triglycerides are 100, and my cholesterol is 178. I'm pretty worried about the LDL number. Are these levels okay, or should I be concerned? Can you help clear up my doubt?
Based on the provided readings, your LDL level of 123 mgdL falls within the optimal range for LDL cholesterol (less than 100 mgdL is considered optimal). Your triglyceride level of 100 mgdL is also within the normal range (less than 150 mgdL is considered normal). Additionally, your total cholesterol level of 178 mgdL is within the desirable range (less than 200 mgdL is considered desirable). Overall, your lipid profile seems to be within normal limits. However, it is always important to consider other risk factors for heart disease and consult with your healthcare provider for a comprehensive evaluation.
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.