- Male
- 58 Years
- 22/01/2025
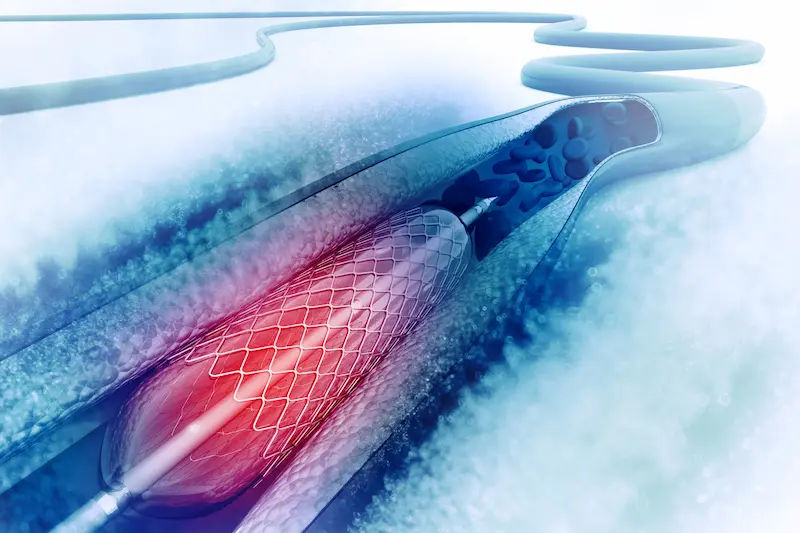
I'm really concerned about my dad's health. Last year in July, he had angioplasty and the doctor put two stents in one artery and one stent in another. He's been following the doctor's diet and taking his meds regularly. Is there still a chance his blood vessels might get blocked again?
Answered by 1 Apollo Doctors
It is important for your father to continue taking his prescribed medications and follow the doctor's diet chart to reduce the risk of blockage in the blood vessels. To further prevent blockage, the following medications are commonly prescribed after angioplasty: 1. Antiplatelet agents such as Aspirin or Clopidogrel to prevent blood clots - Dosage as per doctor's prescription 2. Statins such as Atorvastatin or Rosuvastatin to lower cholesterol levels - Dosage as per doctor's prescription 3. ACE inhibitors or ARBs to control blood pressure and improve heart function - Dosage as per doctor's prescription 4. Beta-blockers to reduce the heart's workload and lower blood pressure - Dosage as per doctor's prescription Regular follow-up appointments with the cardiologist are also important to monitor your father's heart health and make any necessary adjustments to his treatment plan.
Dr. Dhankecha Suggests...
Consult a Cardiologist
Answered 04/07/2025
0
0

More Cardiology Health Queries
View allI've been having this burning sensation on the left side of my chest, and today I noticed there's some swelling under my ribs. It's really worrying me since I remember 2 years ago, I went through a bunch of heart checkups, and everything was fine. The doctor back then said it was because of my poor lifestyle. But now, I'm not sure what's causing this pain again. Could you suggest what might be going on and which specialist I should see?
no need to worry follow your doctors advice
Answered by 1 Apollo Doctors
I'm a bit concerned about my heart health. A year and a half ago, I was diagnosed with sinus arrhythmia, and my doctor put me on Vodafone 100. Since then, I've been taking the medication regularly, but my recent Holter report shows sinus bradycardia. Everything else like my lipid, liver, thyroid, and kidney profiles are normal, so I'm confused about what's going on. Could this be related to the medication, or is there something else I should be aware of? What steps should I take next?
Its time to switch or taper the drug that you are using,visit Cardiologist for appropriate management
Answered by 1 Apollo Doctors
I'm feeling like there's a weight on my chest, and every so often, it really hurts. I've had COVID twice but I'm on the mend now. I was thinking of getting a chest x-ray, but I noticed there are different kinds, like AP view and lateral view. I'm not sure which one I should go for. Can you help?
Patient is advised complete blood count,esr,C-reactive protein and chest x-ray pa view.
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.