- male
- 50 Years
- 20/02/2025
I'm really worried about my incomplete RBBB turning into a complete RBBB in the future. Are there treatments like an angiogram or angioplasty that can help prevent this from happening? Is there any way to make my RBBB go back to normal, like it was before, so there's no block at all?
Answered by 1 Apollo Doctors
Its reversible,visit Cardiologist for appropriate management and have a regular follow up
Dr. Ibrahim Suggests...
Consult a Cardiologist
Answered 04/07/2025
0
0


Ask Apollo
AI powered Health Chatbot
Understanding Incomplete Right Bundle Branch Block (RBBB)
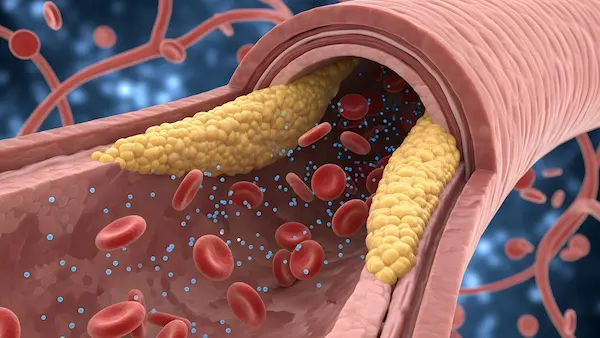
- Incomplete RBBB: A condition where electrical impulses are delayed in the right bundle branch of the heart. It is often benign and may not require treatment.
Causes and Risks of Progression to Complete RBBB
- Progression Factors: Underlying heart conditions like hypertension or coronary artery disease can contribute to progression.
Diagnostic Evaluation
- Cardiac Evaluation: Essential tests include ECG and echocardiogram.
- Angiogram: Considered if coronary artery disease is suspected.
Treatment and Management Options
- General Approach: Focus on monitoring and managing any underlying conditions.
- Angioplasty: Used for coronary artery disease, not directly for RBBB.
- Medications and Lifestyle: Support heart health through prescribed medications and lifestyle changes.
Possibility of Reversal of Incomplete RBBB
- Reversal: Often does not revert completely. Focus on controlling contributing factors to prevent progression.
When to Consult a Cardiologist
- Specialist Evaluation: Important for personalized advice and follow-up.
Summary and Reassurance
- Reassurance: Incomplete RBBB is generally benign. Regular check-ups and a heart-healthy lifestyle are crucial.
Recommended next steps
Consult a Cardiologist
Answered 10/09/2025
0
0
More Cardiology Health Queries
View allI'm really concerned because I have a history of minoxidil poisoning and now I'm experiencing chest pain even when I'm just resting. I also feel like my heart starts beating really fast out of nowhere, like palpitations. I don't have a smoking history, so I'm not sure what's causing this. Could this be related to the past poisoning, or should I be worried about something else?
Getting chest pain while resting and palpitations like symptoms can be concerning. It is important to seek medical attention immediately. In the meantime, you can take aspirin 325mg for chest pain as it can help with heart-related issues. Please do not delay in seeking medical help.
Answered by 1 Apollo Doctors
I'm really concerned because my heart beat rate has been around 100-110 bpm throughout the day, but when I'm resting, like right after I wake up, it's at 80 bpm. Are these numbers something I should be worried about? Ive had an ECG treadmill test and an electrolyte test, and my doctor said they were all normal. I'm still worried, so what should I do about this high heart rate?
get thyroid profile done
Answered by 1 Apollo Doctors
Which arm to measure blood pressure right or left?
Both the arms can be used for BP measurement and sometimes, your doctor might take two readings from two arms to check for any variations too. Generally, it's best to take your blood pressure from your left arm if you are right-handed.
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.