- male
- 25 Years
- 22/01/2025
I've been having these heart palpitations for about 4 years now, where my heart just suddenly starts pounding, fluttering, or even racing out of nowhere, even when I'm not doing anything physical. The first time it happened was during a cricket practice right after I started jogging, and since then, it's been an on-and-off thing. It freaks me out whenever it happens, and I'm really worried about what it means for my future. Most of the time, I try not to think about it, and my heartbeat stays normal, but then, bam, it starts racing again when I'm just chilling. This issue made me quit sports, so I turned to yoga, which kind of helps since I'm focusing more on my breathing. The weird thing is, the first time I got an ECG, it showed my heart rate was at 122 beats per minute. The doctor back then just told me to avoid stress, but then my mom passed away, which was super stressful, and it made the palpitations worse. But it's strange because I don't have chest pain or dizziness. What do you make of this? Should I be really worried?
Answered by 1 Apollo Doctors
It sounds like you have been dealing with heart palpitations for a while now, which can be quite distressing. Based on your description, it seems like you may be experiencing episodes of supraventricular tachycardia (SVT), which can cause the fluttering, pounding, and racing sensations in your heart. One medication that is commonly used to help control heart palpitations like SVT is Verapamil. The usual dosage for Verapamil in cases of SVT is around 120-240 mg per day, divided into 3-4 doses. Additionally, if you are still experiencing palpitations despite lifestyle changes like yoga, your doctor may consider prescribing you a beta-blocker such as Metoprolol. The typical starting dose for Metoprolol in cases of palpitations is 25-50 mg twice a day. It is important to follow up with your doctor regularly to monitor your condition and adjust your treatment plan as needed. Remember to also continue practicing stress-reducing techniques like yoga to help manage your symptoms.
Dr. Dhankecha Suggests...
Consult a Cardiologist
Answered 04/07/2025
0
0

More Cardiology Health Queries
View allI've been dealing with high blood pressure for the past two months and have been taking metoprolol 50 mg since the first month. Initially, everything was going well, and my blood pressure was 11070, but lately, over the past week, my diastolic pressure is sticking around 85 to 90. It seems like the meds aren't working as well now. I've increased to 50 mg twice a day. What should I do?
Its important to effectively manage your blood pressure, especially if it has started to rise again despite medication. It might be necessary to adjust your treatment plan. Continue monitoring your blood pressure regularly, and consider keeping a log of your readings to discuss with your doctor. In addition to adjusting your dose of Metoprolol, your healthcare provider might consider adding another antihypertensive medication to your regimen. There are several classes of medications that can be used in combination with beta-blockers, such as ACE inhibitors, calcium channel blockers, or diuretics. I recommend scheduling an appointment with your healthcare provider to review your current treatment plan and discuss potential adjustments. They can also evaluate for any underlying factors that might be contributing to the increased blood pressure.
Answered by 1 Apollo Doctors
I'm a bit worried about my blood pressure. It was moderately high a month ago, and now I'm taking Natrilix, 1.5 mg Indapamide. Is it safe for me to have a can of beer every six months, or should I be concerned? I came across some stuff online that's got me scared, and my doctor is currently out of the country.
Avoid alcohol
Answered by 1 Apollo Doctors
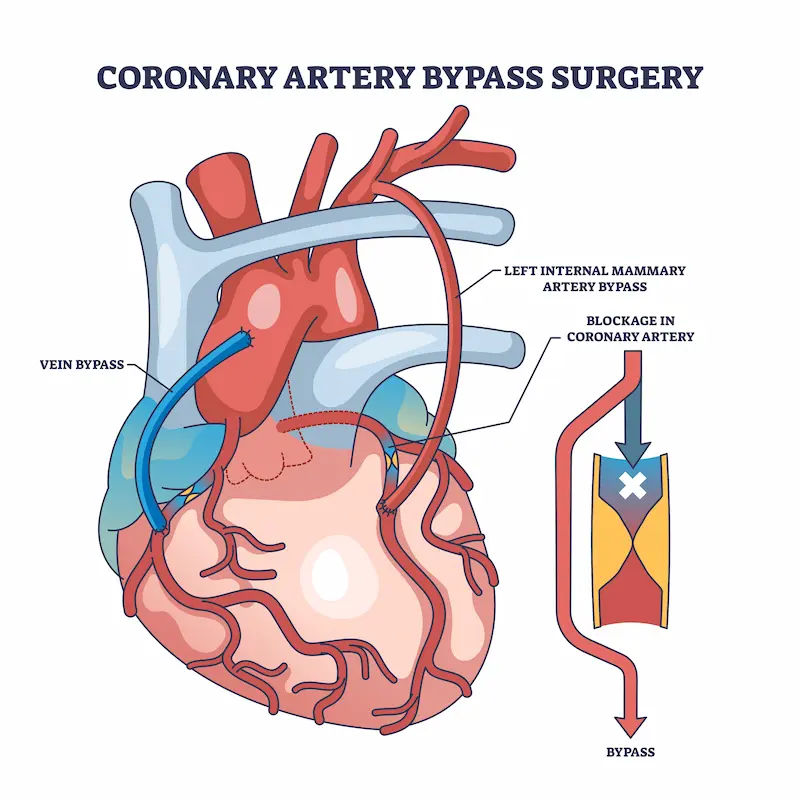
Is a blood pressure reading of 13565 with a heart rate of 76 normal for someone who has stents in both left and right arteries since April 2021 and also has diabetes along with other health issues? I'm a little concerned about whether these numbers are okay given the circumstances.
The blood pressure reading of 13565 is within the normal range. For individuals with a history of heart issues, such as having stents placed in the arteries, it is important to closely monitor blood pressure. In this case, the blood pressure reading is considered normal. However, it is always advisable to continue monitoring blood pressure regularly and follow up with her healthcare provider for further guidance.
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.