Guide to Stages Alcoholic Liver Disease And How
Understand the stages of alcoholic liver disease (ALD) – from fatty liver to alcoholic hepatitis and cirrhosis. Learn about symptoms, diagnosis, and crucial management steps to halt progression and improve liver health.

Written by Dr. D Bhanu Prakash
Reviewed by Dr. Mohammed Kamran MBBS, FIDM
Last updated on 13th Jan, 2026
Introduction
The liver is one of the body's most resilient organs, capable of regenerating after minor injuries. However, its ability to withstand damage has a limit, especially when faced with a constant onslaught of alcohol. Alcoholic liver disease (ALD) is a serious and potentially fatal condition that creeps in silently, often showing no obvious signs until significant harm has already been done. Understanding the stages of alcoholic liver disease is the first step toward prevention, early detection, and effective management. This guide will walk you through the three critical phases—from the reversible early stage of fatty liver to the severe scarring of cirrhosis. We'll demystify the symptoms, explain the diagnostic process, and outline the treatment options available at each point. Whether you're concerned for yourself or a loved one, knowledge is power when it comes to protecting your liver health.
Understanding Your Liver: The Body's Detox Powerhouse
Before diving into the disease itself, it's crucial to appreciate the liver's role. This reddish-brown organ, located in the upper right abdomen, is your body's primary filtration system.
The Liver's Vital Functions
The liver performs over 500 essential jobs. Key functions include:
Detoxification: It processes and neutralizes toxins, including alcohol, drugs, and metabolic waste.
Metabolism: It helps break down fats, proteins, and carbohydrates for energy.
Storage: It stores vitamins, minerals, and glycogen (a form of energy).
Synthesis: It produces bile, which is essential for digesting fats, and creates important proteins like albumin and clotting factors.
How Alcohol Damages Liver Cells?
When you drink alcohol, your liver prioritizes its metabolism above all else. This process produces toxic byproducts that damage liver cells, promote inflammation, and cause fat to accumulate. Over time, with heavy, consistent drinking, this damage accumulates, leading to the progressive stages of alcoholic liver disease.
Health Topic Carousel:
Doctor Speciality: General Physician
Text: Consult Top Specialists
The 3 Progressive Stages of Alcoholic Liver Disease
Alcoholic liver disease progresses sequentially through three main stages. The speed of progression varies from person to person, influenced by factors like genetics, gender, nutrition, and overall health.
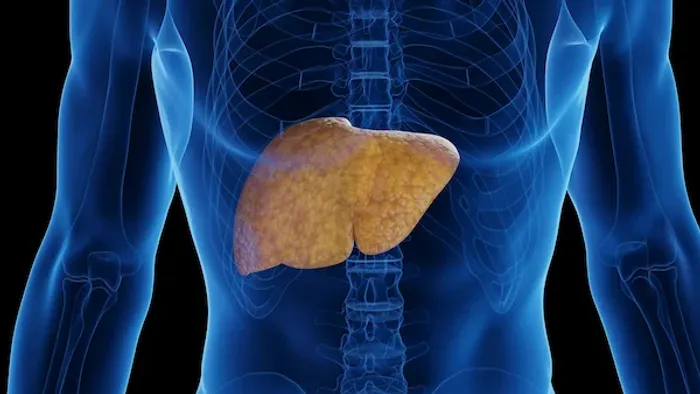
Stage 1: Alcoholic Fatty Liver Disease (AFLD)
This is the earliest and most common stage of alcohol-related liver damage. It occurs in over 90% of heavy drinkers.
What Happens in the Liver?
The liver cells (hepatocytes) become infiltrated with fat droplets. This buildup of fat, known as steatosis, is a direct result of the liver's altered metabolism while processing alcohol.
Common Symptoms (or Lack Thereof)
AFLD is notoriously silent. Most people experience no noticeable symptoms. Some may feel mild fatigue or discomfort in the upper right abdomen, but these signs are easy to ignore or attribute to other causes.
Is It Reversible?
Yes, this is the most crucial point about Stage 1. Alcoholic fatty liver disease is almost entirely reversible. The treatment is straightforward: complete and permanent alcohol abstinence. If a person stops drinking at this stage, the fat can disappear, and the liver can heal itself within a few weeks to months. This makes early detection through routine check-ups incredibly valuable.
Stage 2: Alcoholic Hepatitis
"Hepatitis" simply means inflammation of the liver. If drinking continues beyond the fatty liver stage, the ongoing injury triggers widespread inflammation.
Inflammation and Scarring Begin
This stage involves the swelling and death of liver cells. The body's attempt to repair this damage leads to the initial formation of scar tissue, a process known as fibrosis. Alcoholic hepatitis can range from mild to severe, even life-threatening.
Recognizing the Symptoms
Unlike the silent first stage, symptoms of alcoholic hepatitis are often apparent and can be the first warning sign that prompts someone to seek medical help. They include:
Jaundice (yellowing of the skin and eyes)
Fever
Nausea and vomiting
Loss of appetite and weight loss
Tenderness and pain in the abdomen
Fatigue and weakness
Acute vs. Chronic Hepatitis
Acute Alcoholic Hepatitis is a sudden, severe flare-up that can occur after a bout of heavy drinking.
Chronic Alcoholic Hepatitis is a persistent, long-term inflammation seen in people who continue to drink heavily.
While some of the inflammation can subside with abstinence, the scarring (fibrosis) that occurs may be permanent. The goal of treatment is to stop the progression.
Stage 3: Alcoholic Cirrhosis
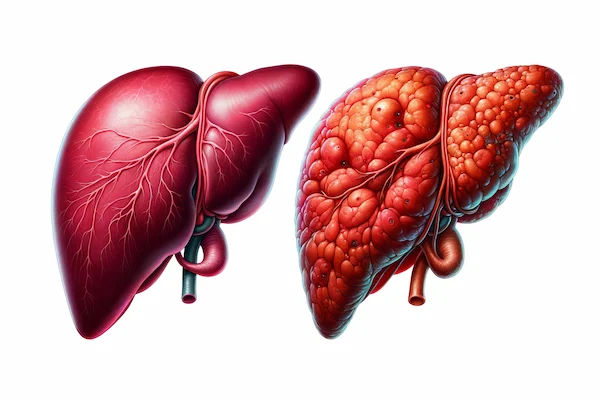
Cirrhosis is the end-stage of liver disease, representing irreversible damage.
The Point of Irreversible Scarring
After years of chronic inflammation, the healthy liver tissue is replaced by extensive bands of scar tissue (fibrosis). This scar tissue nodules the liver, making it hard and shrunken. This extensive scarring is what defines cirrhosis. It can take years or even decades of heavy drinking to reach this point.
Symptoms of Late-Stage Liver Disease
As the liver's function severely declines, symptoms become debilitating:
Advanced Jaundice
Ascites: A buildup of fluid in the abdomen, causing swelling.
Easy bruising and bleeding: Due to impaired production of clotting factors.
Portal Hypertension: Increased blood pressure in the vein leading to the liver, which can cause swollen veins (varices) in the esophagus and stomach that can rupture and bleed dangerously.
Hepatic Encephalopathy: A buildup of toxins in the brain leading to confusion, drowsiness, and slurred speech.
Intense itching.
Complications and Prognosis
Cirrhosis is a major health concern. While the damage is largely irreversible, stopping alcohol completely is vital to prevent further progression and life-threatening complications like liver failure and liver cancer. Management focuses on treating symptoms. In severe cases, a liver transplant may be the only curative option, for which candidates must demonstrate a period of sustained abstinence.
How is Alcoholic Liver Disease Diagnosed?
Early diagnosis can significantly alter the course of the disease. If you have a history of heavy drinking, even without symptoms, it's wise to get evaluated. If you're experiencing any of the symptoms mentioned, especially jaundice or abdominal swelling, consult a doctor online with Apollo24|7 for an initial assessment and guidance on next steps.
Blood Tests and Liver Function Tests (LFTs)
These tests measure levels of liver enzymes (like ALT and AST). Elevated levels indicate inflammation or damage to liver cells. Other markers, like bilirubin (for jaundice) and albumin, assess the liver's functional capacity. Apollo24|7 offers a convenient home collection for these essential liver function tests.
Imaging: Ultrasounds, CT Scans, and FibroScan
Ultrasound: Can easily detect a fatty liver and advanced cirrhosis.
CT/MRI Scans: Provide more detailed images of the liver's structure.
FibroScan: A specialized, non-invasive test that measures liver stiffness, which correlates with the degree of fibrosis or scarring.
The Role of a Liver Biopsy
This is the gold standard for diagnosing the stage of liver disease. A small sample of liver tissue is removed with a needle and examined under a microscope to assess fat, inflammation, and scarring directly.
Treatment and Management at Every Stage
The cornerstone of treatment for alcoholic liver disease at any stage is stopping alcohol consumption. The specific approach then depends on the severity.
The Universal First Step: Complete Alcohol Abstinence
This is non-negotiable. For fatty liver, it can mean a complete cure. For later stages, it halts progression and prevents further complications. Support groups, counseling, and sometimes medication are essential to achieve this.
Nutritional Support and Lifestyle Changes
Malnutrition is common. A healthy, balanced diet rich in proteins and calories is crucial to help the liver regenerate and support overall health. Weight management and controlling other conditions like diabetes are also important.
Medications for Managing Symptoms and Complications
Corticosteroids: May be used to reduce severe inflammation in alcoholic hepatitis.
Diuretics: "Water pills" help reduce fluid buildup in ascites.
Lactulose: A medication used to treat hepatic encephalopathy by reducing ammonia levels.
Liver Transplantation: A Last Resort
For patients with end-stage liver failure who have stopped drinking for a significant period (typically at least six months), a transplant may be an option. It's a complex process with strict criteria.
Prevention and Early Intervention: Your Best Defense
The most effective way to prevent alcoholic liver disease is to drink in moderation or not at all. The recommended limits are no more than one drink per day for women and two for men. If you have any risk factors, such as a family history or other liver conditions, it's even more critical to be cautious. Regular health check-ups that include liver function tests are a proactive way to catch any issues early.
Conclusion
Navigating the stages of alcoholic liver disease underscores a powerful message: early action saves lives. While the journey from a fatty liver to cirrhosis is a dangerous one, it is not inevitable. The liver possesses a remarkable ability to heal, but only if we give it the chance. The most critical step at any stage is to stop the consumption of alcohol. If you recognize yourself or someone you care about in the descriptions of the early stages of this disease, view it as a crucial warning sign and an opportunity for change. If your condition does not improve after trying these methods, or if you need support with alcohol cessation, book a physical visit to a doctor with Apollo24|7. Taking control of your health today can prevent the severe complications of tomorrow and pave the way for a healthier future.
Health Topic Carousel:
Doctor Speciality: General Physician
Text: Consult Top Specialists
Frequently Asked Questions (FAQs)
1. How long does it take to get alcoholic fatty liver disease?
A. Alcoholic fatty liver can develop in as little as a few days to weeks of heavy alcohol consumption. However, it's reversible if drinking stops.
2. Can you die from alcoholic hepatitis?
A. Yes, severe acute alcoholic hepatitis has a high mortality rate. It is a medical emergency that requires immediate hospitalization.
3. What is the life expectancy for someone with alcoholic cirrhosis?
A. Life expectancy varies greatly. With complete abstinence, many people with compensated cirrhosis (where the liver is scarred but still functioning) can live for years. If complications develop (decompensated cirrhosis), the prognosis is more serious, and a transplant may be needed.
4. Is alcoholic liver disease different from non-alcoholic fatty liver disease (NAFLD)?
A. Yes. While both can lead to fatty liver, hepatitis, and cirrhosis, they have different primary causes. NAFLD is linked to metabolic syndrome (obesity, diabetes), not alcohol consumption. However, the damage to the liver can look very similar.
5. Are there any medications to reverse liver damage from alcohol?
A. There are no specific medications that can reverse existing scar tissue (cirrhosis). The most effective "treatment" is abstinence, which allows the liver to heal itself and prevents further damage. Medications are used to manage symptoms and complications.
Consult Top Specialists for Personalised Tips

Dr Aakash Andgi
General Physician/ Internal Medicine Specialist
9 Years • MBBS MD
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr Syed Mateen Pasha
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Ashita Kuruvilla
General Physician/ Internal Medicine Specialist
7 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore
Consult Top Specialists

Dr Aakash Andgi
General Physician/ Internal Medicine Specialist
9 Years • MBBS MD
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr Syed Mateen Pasha
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Ashita Kuruvilla
General Physician/ Internal Medicine Specialist
7 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore