Guide to Alcohol-Related Liver Diseases & How to Stay Safe
Learn about alcohol-related liver diseases, from fatty liver to cirrhosis. Understand risk factors, symptoms, diagnosis, and prevention strategies to protect your liver and stay safe.

Introduction
Your liver is your body's ultimate multitasker—processing nutrients, filtering toxins, and fighting infection, all without a whisper of complaint. This silence is both a blessing and a curse, especially when it comes to alcohol. Alcohol-related liver disease (ALD) is a stealthy, progressive condition that often reveals itself only after significant damage is done. The good news? It is also one of the most preventable forms of liver disease. This guide will walk you through the journey of how alcohol affects your liver, from the earliest stages of fat accumulation to the severe scarring of cirrhosis. We'll help you understand your personal risk factors, identify warning signs, and outline a clear path toward prevention, early detection, and treatment. Understanding these liver diseases and their risk is the first crucial step toward taking back control of your health.
Understanding Your Liver: The Body's Silent Powerhouse
Your liver, weighing about three pounds, is your largest internal organ and your metabolic command center. Think of it as a highly sophisticated processing plant that operates 24/7. It's responsible for over 500 vital functions, including converting food into energy, manufacturing essential proteins for blood clotting, and storing vitamins and minerals. Its most critical role, however, is detoxification. Everything you eat, drink, and absorb through your skin is eventually filtered through the liver, which neutralises harmful substances before they can circulate through your body.
This is precisely why the liver is vulnerable to alcohol. When you consume an alcoholic drink, your body prioritises metabolising the alcohol over its other tasks. The liver breaks down about 90% of this alcohol using enzymes. While this process neutralises the immediate threat, it generates toxic byproducts like acetaldehyde. These toxins damage liver cells, promote inflammation, and can lead to permanent scarring over time. The liver's incredible ability to regenerate can keep up with occasional assaults, but chronic, heavy drinking overwhelms this system, setting the stage for serious alcoholic liver damage.
Consult a Hepatologist for the best advice
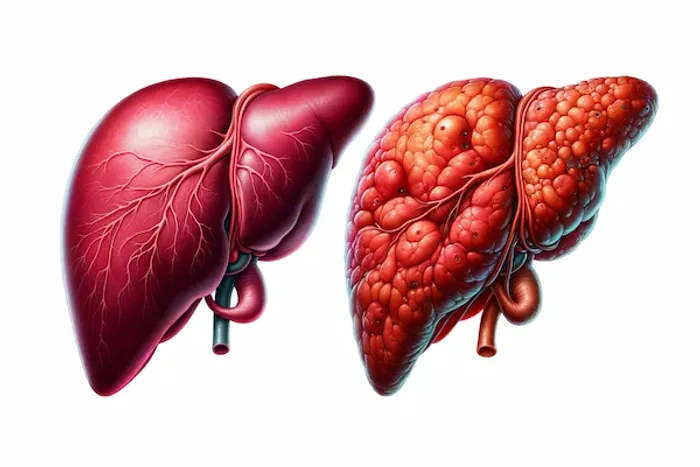
The Spectrum of Alcohol-Related Liver Disease (ALD)
ALD isn't a single event; it's a spectrum of conditions that worsen progressively with continued alcohol use.
Stage 1: Alcoholic Fatty Liver Disease (AFLD)
This is the earliest and most common stage, affecting over 90% of heavy drinkers. It occurs when the liver, busy processing alcohol, starts storing fat within its cells. A key insight often missed is that AFLD is almost entirely reversible. At this stage, there are typically no symptoms, and the damage can be undone within weeks of complete alcohol abstinence, coupled with a healthy diet. It serves as a critical warning sign from your body.
Stage 2: Alcoholic Hepatitis
This stage is characterised by inflammation and cell death in the liver. "Hepatitis" simply means inflammation of the liver. It can range from mild to life-threatening. Symptoms may include loss of appetite, nausea, abdominal pain, jaundice (yellowing of the skin and eyes), and fever. While mild cases can be reversed with abstinence, severe alcoholic hepatitis is a medical emergency with a high mortality rate. It represents a significant escalation from simple fat accumulation.
Stage 3: Alcoholic Cirrhosis
The final and most severe stage is cirrhosis, where widespread scarring (fibrosis) replaces healthy liver tissue. This scar tissue cannot perform any function and blocks the flow of blood through the liver, leading to liver failure. Cirrhosis is generally irreversible, but stopping alcohol immediately can prevent further damage and stabilise the condition. Symptoms of advanced cirrhosis include intense jaundice, swelling in the legs and abdomen (ascites), extreme fatigue, and confusion. Managing this stage focuses on preventing complications and may require evaluation for a liver transplant.
Are You at Risk? Calculating Your Personal Danger Level
Understanding your risk goes beyond just counting drinks.
How Much Alcohol is Too Much? Defining Standard Drinks
The risk of developing ALD is directly related to the amount and duration of alcohol consumption. Guidelines define heavy drinking as:
For men: Consuming more than 4 drinks on any day or more than 14 drinks per week.
For women: Consuming more than 3 drinks on any day or more than 7 drinks per week.
A "standard drink" is key to this calculation: it's 14 grams of pure alcohol, equivalent to 12 oz of regular beer (5% ABV), 5 oz of wine (12% ABV), or 1.5 oz of distilled spirits (40% ABV).
Key Risk Factors Beyond Consumption
Gender and Genetic Predisposition: Women are more susceptible to ALD at lower levels of alcohol consumption than men due to differences in body water content, metabolism, and hormones. Genetics also play a role in how efficiently your body metabolises alcohol.
Co-existing Liver Conditions: Having another form of liver disease, like Hepatitis B or C, drastically accelerates alcohol-induced damage.
Obesity and Poor Nutrition: A high-fat diet and obesity compound the stress on the liver. Malnutrition, common in heavy drinkers who replace food with alcohol, deprives the liver of the nutrients it needs to function and repair itself.
If you are concerned about your drinking patterns and their impact on your health, it is crucial to seek professional guidance. You can consult a hepatologist or a general physician online with Apollo24|7 to discuss your risk factors confidentially and create a personalised plan.
Listening to Your Body: Symptoms You Must Not Ignore
ALD is often "silent" until advanced stages, but subtle signs can appear.
Early Signs (Often Missed)
Unexplained fatigue and general weakness.
A dull ache or discomfort in the upper right abdomen.
Nausea or loss of appetite.
Symptoms of Advanced Liver Disease
Jaundice: Yellowing of the skin and the whites of the eyes.
Ascites: Swelling and fluid buildup in the abdomen.
Oedema: Swelling in the legs, ankles, and feet.
Easy bruising and bleeding: Due to the liver's impaired production of clotting proteins.
Confusion or brain fog (hepatic encephalopathy): Toxins building up in the brain.
If symptoms like jaundice or abdominal swelling appear, it is a medical red flag. Book a physical visit to a doctor with Apollo24|7 immediately for a thorough evaluation.
Getting a Diagnosis: Tests and Doctor Consultations
Early diagnosis can change the outcome. If your doctor suspects ALD, they will recommend a series of tests.
Common Blood Tests and What They Mean (LFTs)
Liver function tests (LFTs) measure enzyme and protein levels. Key markers include elevated AST and ALT (indicating cell damage) and bilirubin (indicating jaundice). An elevated AST/ALT ratio (greater than 2:1) is particularly suggestive of alcoholic liver injury.
Imaging: Ultrasounds, FibroScan, and MRIs
An abdominal ultrasound can easily detect fat accumulation and early signs of cirrhosis. A FibroScan is a specialised, non-invasive ultrasound that measures liver stiffness, which correlates with the level of scarring (fibrosis). MRIs provide even more detailed images.
The Gold Standard: Liver Biopsy
A biopsy, where a small sample of liver tissue is extracted with a needle for analysis, remains the most accurate way to diagnose the stage and severity of liver damage, especially to confirm alcoholic hepatitis or the degree of cirrhosis.
Apollo24|7 offers convenient home collection for essential blood tests like liver function tests (LFTs), making the first step in diagnosis easier and more accessible.
Get Your Health Assessed
Conclusion
The path of alcohol-related liver disease is predictable and, for the most part, preventable. Your liver possesses a remarkable capacity for healing, but it requires you to make conscious choices. Understanding the risk factors and stages of these diseases empowers you to take action before it's too late. Remember, the most powerful step you can take is moderation or abstinence. Coupled with a nutritious diet and regular health check-ups, you can safeguard your liver's health for years to come. Your body's silent powerhouse relies on you to be its voice. Listen to it, protect it, and if you have any concerns, don't hesitate to seek professional medical advice. Your future health is worth it.
Consult a Hepatologist for the best advice
Consult a Hepatologist for the best advice

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(175+ Patients)

Dr. Akshatha Manjunath
General Surgeon
8 Years • MBBS, MS
Bangalore
Apollo Clinic Bellandur, Bangalore

Dr. Pukhraj Singh Jeji
Gastroenterology/gi Medicine Specialist
13 Years • MBBS, MD ( Internal Medicine ), DM ( Gastroenterology ), Consultant - Gastroenterology
Bhubaneswar
Apollo Hospitals Old Sainik School Road, Bhubaneswar

Dr. Sushith C
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Aswin S. Krishna
Hepatologist
10 Years • MBBS, MD (Internal Medicine,MMC), DM (Hepatology, MMC), PDF(Fellowship in Liver Transplanatation)
Chennai
Apollo Hospitals Greams Road, Chennai
(125+ Patients)