The Sobering Link Between Binge Drinking and Liver Disease
Know about the alcohol and liver diseases. What is the link between them, know about acetaldehyde, signs, symptoms, diagnosis, prevention and management of excessive alcohol consumption. Learn about treatment options and more.

Introduction
That Friday night feeling often includes a few extra drinks. You tell yourself it’s just a one-off, a way to unwind from the week. But when these "one-offs" become a pattern of binge drinking, you're playing a dangerous game with one of your body's most vital organs: your liver. Many people associate liver disease with a lifetime of heavy daily drinking, but emerging research shows that repeated episodes of binge drinking can be just as damaging, if not more so in some cases. This article cuts through the confusion to explore the direct and sobering connection between binge drinking and alcoholic liver disease. Your liver is resilient, but it has its limits.
What Exactly is Binge Drinking? More Than Just a "Big Night"
We often use the term "binge" casually, but in medical terms, it has a specific definition. Understanding this is the first step in recognising your own risk.
The Standard Medical Definition
The National Institute on Alcohol Abuse and Alcoholism (NIAAA) defines binge drinking as a pattern of consumption that brings your blood alcohol concentration (BAC) to 0.08 grams per deciliter or above.
This typically translates to:
- For men: 5 or more standard drinks within 2 hours.
- For women: 4 or more standard drinks within 2 hours.
A "standard drink" is 14 grams of pure alcohol, found in a 12-oz beer (~5% ABV), a 5-oz glass of wine (~12% ABV), or 1.5 oz of distilled spirits (~40% ABV). It's not about the type of drink, but the total amount of alcohol consumed in a short window.
Consult a Top General Practitioner for Personalised Advice
How Binge Drinking Differs from Alcohol Use Disorder
It's a common misconception. You can binge drink without being alcohol-dependent. Many binge drinkers are not daily consumers; they might not even drink during the week. This pattern is often seen in college students or working professionals who "save up" their drinking for the weekend. However, this behaviour is a significant risk factor for developing Alcohol Use Disorder (AUD) down the line and causes acute and chronic harm independently.
Your Liver: The Body's Silent Powerhouse
To understand the damage, you must first appreciate the liver's incredible role. It's not just a filter; it's a multifunctional metabolic factory.
Key Functions: Filtering, Metabolising, and Storing
Your liver performs over 500 essential functions, including:
- Detoxification: Processing and removing toxins, drugs, and alcohol from the blood.
- Metabolism: Breaking down fats, proteins, and carbohydrates for energy.
- Synthesis: Producing vital proteins like albumin and clotting factors.
- Storage: Holding onto key vitamins and minerals like iron and glycogen.
How the Liver Processes Alcohol
The liver is the primary site for alcohol metabolism. It uses two key enzymes:
1. Alcohol dehydrogenase (ADH): Converts alcohol to acetaldehyde, a highly toxic and carcinogenic compound.
2. Aldehyde dehydrogenase (ALDH): Quickly converts the toxic acetaldehyde into acetate, which is eventually broken down into water and carbon dioxide for elimination.
This process is efficient in moderation but becomes a major problem during a binge.
How Binge Drinking Overwhelms and Injures Your Liver?
When you binge drink, you flood your system with more alcohol than your liver can process efficiently.
The Toxic Byproduct: Acetaldehyde
During a binge, the ADH enzyme works overtime, creating a massive backlog of acetaldehyde. Since the ALDH enzyme can only work so fast, this toxic substance builds up in the liver. This acetaldehyde is 30 times more toxic than alcohol itself. It damages liver cells, promotes inflammation, and impairs the liver's ability to break down fats, leading to their accumulation.
Inflammation and Oxidative Stress
The presence of excess alcohol and acetaldehyde triggers your body's immune response, sending inflammatory cells to the liver. This causes swelling and damage known as hepatitis. Simultaneously, alcohol metabolism generates reactive oxygen species (ROS), or free radicals, causing oxidative stress. This oxidative stress further damages liver cell structures, including mitochondria and DNA, accelerating cell death.
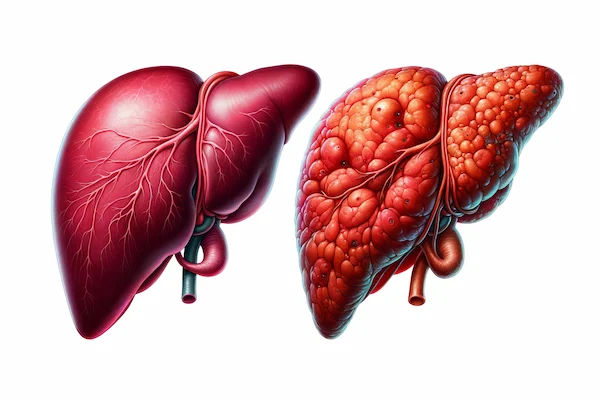
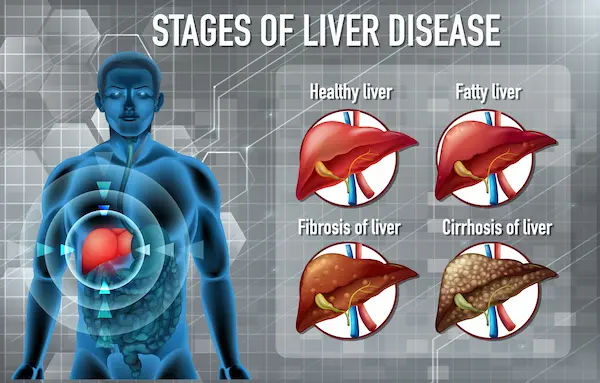
The Progressive Stages of Alcoholic Liver Disease (ALD)
ALD doesn't happen overnight. It's a spectrum of disease that progresses through three main stages if drinking continues.
Stage 1: Alcoholic Fatty Liver Disease (Steatosis)
This is the earliest and most common alcohol-related liver injury. It involves a build-up of fat inside liver cells (hepatocytes).
Key facts:
- Cause: The toxic byproducts of alcohol metabolism disrupt the liver's normal process of breaking down and exporting fat.
- Reversibility: This stage is almost universally reversible with complete abstinence from alcohol, often within 4-6 weeks.
- Symptoms: It is largely silent, with few to no symptoms. Some people may experience mild fatigue or vague discomfort in the upper right abdomen.
Stage 2: Alcoholic Hepatitis
This is not the same as infectious hepatitis (viral hepatitis). Alcoholic hepatitis refers to acute inflammation and swelling of the liver caused by heavy alcohol use.
Key facts:
- Cause: The ongoing insult from alcohol and acetaldehyde leads to significant inflammation, causing liver cells to die.
- Symptoms: This can range from mild to life-threatening. Symptoms may include jaundice (yellowing of skin and eyes), fever, nausea, vomiting, abdominal pain and tenderness, and loss of appetite.
- Outcome: With severe alcoholic hepatitis, mortality can be as high as 40% within six months. Abstinence is critical. Mild to moderate cases can improve with stopping alcohol.
Stage 3: Alcoholic Cirrhosis
The final and most severe stage, cirrhosis, is the scarring (fibrosis) of the liver. Scar tissue replaces healthy liver tissue, blocking blood flow and severely impairing function. Key facts:
- Irreversibility: While further damage can be halted, the scarring from cirrhosis is generally permanent and irreversible.
- Symptoms: Symptoms of advanced liver disease become prominent: intense jaundice, ascites (fluid buildup in the abdomen), easy bruising and bleeding, confusion (hepatic encephalopathy), and variceal bleeding.
- Prognosis: Cirrhosis is a major health risk. Management focuses on treating complications, and in end-stage cases, a liver transplant may be the only option.
Recognising the Symptoms: When Your Liver is Calling for Help
The liver is a non-complaining organ until it's severely damaged. Knowing the signs is crucial.
Early Signs Often Missed
The symptoms of early alcoholic liver disease are vague and easily attributed to other things:
- Persistent fatigue and low energy
- A general feeling of being unwell (malaise)
- Unexplained digestive issues
- Discomfort or a feeling of fullness in the upper right abdomen
Symptoms of Advanced Liver Disease
When the liver is failing, the signs are unmistakable and require immediate medical attention:
- Jaundice: Yellow tint to the skin and the whites of the eyes.
- Ascites: Swelling and fluid buildup in the abdominal cavity.
- Oedema: Swelling in the legs, ankles, and feet.
- Spider Angiomas: Spider-like blood vessels visible on the skin.
- Confusion and Slurred Speech: A sign of toxins affecting the brain (hepatic encephalopathy).
- Dark Urine and Pale Stools: Changes in waste elimination.
If you are experiencing any of these advanced symptoms, it is imperative to consult a doctor immediately. You can book a priority consultation online with a specialist on Apollo24|7 for an urgent evaluation.
How is Alcohol-Related Liver Damage Diagnosed?
If you have a history of binge drinking, getting assessed is a proactive step.
Blood Tests and Liver Function Tests (LFTs)
A simple blood test can check your liver function.
Key markers include:
- ALT (Alanine Transaminase) and AST (Aspartate Transaminase): Enzymes that leak into the blood when liver cells are injured. In ALD, AST is often higher than ALT.
- GGT (Gamma-Glutamyl Transferase): A very sensitive marker for alcohol-related liver injury.
- Bilirubin: A high level causes jaundice and indicates the liver is not processing waste properly.
- Albumin and INR: Measure the liver's ability to make proteins needed for blood clotting and other functions.
Apollo24|7 offers convenient home collection for these crucial liver function tests, making it easy to get checked without a lab visit.
Imaging: Ultrasound, CT Scan, and FibroScan
- Ultrasound: Often the first imaging test to detect fat accumulation (fatty liver) and signs of cirrhosis.
CT/MRI Scans: Provide more detailed images of the liver's structure. - FibroScan® (Transient Elastography): A specialised, non-invasive ultrasound that measures liver stiffness, which correlates with the amount of scarring (fibrosis).
Treatment and Management: Can the Damage Be Reversed?
The course of treatment depends entirely on the stage of the disease.
The Absolute Foundation: Complete Alcohol Abstinence
This is the single most important treatment for alcoholic liver disease. For fatty liver, it can lead to complete reversal. For hepatitis and cirrhosis, it stops further progression and can significantly improve outcomes. Quitting alcohol cold turkey can be dangerous for heavy drinkers; medical supervision for detox is often recommended.
Nutritional Support and Medications
- Nutrition: Malnutrition is common. A healthy, nutrient-dense diet is vital. In severe cases, vitamin supplements (especially B vitamins) are given.
- Medications: Corticosteroids may be used to reduce inflammation in severe alcoholic hepatitis. Other drugs may be prescribed to manage complications like itching, fluid retention, and hepatic encephalopathy.
Liver Transplant: A Last Resort
For patients with end-stage liver failure who have stopped drinking (typically for at least 6 months) and have no other options, a transplant may be considered. It's a major surgery with a long recovery and lifelong medication.
Prevention and Reducing Your Risk: It's Never Too Late
The best treatment is always prevention.
Understanding "Safe" Drinking Limits (If They Exist)
According to dietary guidelines, if alcohol is consumed, it should be in moderation—up to 1 drink per day for women and 2 drinks per day for men. However, it's critical to understand that no level of drinking is completely safe from a health perspective. The goal should be to stay well within these limits and avoid binge episodes entirely.
Strategies for Cutting Down or Quitting
- Set a Limit: Decide how many drinks you'll have before you start and stick to it.
- Pace Yourself: Sip your drink slowly. Have a glass of water between alcoholic beverages.
- Eat Food: Never drink on an empty stomach. Food slows the absorption of alcohol.
- Find Alternatives: Explore the growing market of non-alcoholic beers, wines, and cocktails for social situations.
- Seek Support: If you find it difficult to cut down, talk to your doctor. Resources like counselling and support groups (e.g., Alcoholics Anonymous) can be incredibly effective.
Conclusion
The connection between binge drinking and alcoholic liver disease is clear, direct, and backed by robust medical evidence. Dismissing a weekend binge as harmless fun is a dangerous gamble with an organ you cannot live without. The good news is that the liver possesses a remarkable ability to heal itself, especially when given the chance through abstinence in the early stages. Your future self will thank you for the care you show your body today. If you're concerned about your drinking patterns or experiencing any potential symptoms of liver damage, the most important step is to have an honest conversation with a healthcare professional. You can easily consult with a gastroenterologist or general physician online via Apollo24|7 to discuss your concerns and get personalised advice.
Consult a Top General Practitioner for Personalised Advice
Consult a Top General Practitioner for Personalised Advice

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr Syed Mateen Pasha
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Debajyoti Goswami
Obstetrician and Gynaecologist
10 Years • MBBS,D.G.O(DNB),Adv. Infertility Tech.(AIIMS),Fellowship in Diabetes(U.K),Comprehensive Abortion Care(Govt. Of W.B), Certificate in Clinical Embryology(AIIMS, BHUBANESWAR)
Bankura
D.G Clinic, Bankura
(25+ Patients)

Dr. Avinash Pasuparthy
General Practitioner
5 Years • MBBS
Visakhapatnam
Apollo Clinic Vizag, Visakhapatnam
Consult a Top General Practitioner for Personalised Advice

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr Syed Mateen Pasha
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Debajyoti Goswami
Obstetrician and Gynaecologist
10 Years • MBBS,D.G.O(DNB),Adv. Infertility Tech.(AIIMS),Fellowship in Diabetes(U.K),Comprehensive Abortion Care(Govt. Of W.B), Certificate in Clinical Embryology(AIIMS, BHUBANESWAR)
Bankura
D.G Clinic, Bankura
(25+ Patients)

Dr. Avinash Pasuparthy
General Practitioner
5 Years • MBBS
Visakhapatnam
Apollo Clinic Vizag, Visakhapatnam
More articles from Alcoholic Liver Disease
Frequently Asked Questions
Is binge drinking once a week enough to cause liver damage?
Yes, repeated weekly binge drinking can absolutely cause liver damage over time. Each binge causes acute injury (fat accumulation and inflammation). While the liver can repair itself between episodes, chronic repetition overwhelms its regenerative capacity, leading to permanent scarring.
Can you die from alcoholic hepatitis?
Yes, severe acute alcoholic hepatitis is a life-threatening medical emergency. It has a high mortality rate, especially if drinking continues. Immediate hospitalisation and treatment are required.
How long do you have to abstain from alcohol to reverse a fatty liver?
The liver begins to heal surprisingly quickly. For simple alcoholic fatty liver disease, significant improvement can be seen within a few weeks, and it is often completely reversible within 4 to 6 weeks of strict abstinence, coupled with a healthy diet.
What is the difference between alcoholic fatty liver and non-alcoholic fatty liver (NAFLD)?
Both conditions result in fat accumulation in the liver. The primary difference is the cause: Alcoholic Fatty Liver is caused by alcohol consumption, while NAFLD is associated with metabolic syndrome—obesity, insulin resistance, and high cholesterol—in people who drink little to no alcohol.
Are there any medications to help repair liver damage from alcohol?
There are no magic pills to 'repair' the liver. The most effective medicine is abstinence. However, doctors may prescribe medications to manage the complications of liver disease (like water pills for fluid retention) or steroids to reduce severe inflammation in hepatitis. Nutritional