Cancer Treatment and Sexual Health: Reclaiming Intimacy
Learn how cancer treatment can impact sexual health and discover ways to address changes, improve intimacy, and reclaim connection with your partner.

Written by Dr. Vasanthasree Nair
Reviewed by Dr. Dhankecha Mayank Dineshbhai MBBS
Last updated on 13th Jan, 2026

Introduction
A cancer diagnosis and its subsequent treatment are life-altering experiences that affect every part of your being, including your sexuality. It's completely normal to experience changes in your sexual response, your desire, arousal, and ability to orgasm. Yet, this topic is often overlooked in clinical discussions, leaving many survivors feeling isolated and unsure. This article aims to break that silence. We will explore the physical and emotional reasons behind these changes, offer practical advice for different situations, and provide a roadmap for reclaiming intimacy and sexual wellness after cancer. Remember, you are not alone in this journey, and there are many ways to adapt and find new paths to pleasure and connection.
Understanding the Connection: Cancer Treatment and Your Body
Cancer treatments are designed to target and eliminate cancer cells, but they can also affect healthy cells and tissues, leading to a range of side effects that directly and indirectly impact your sexual health. Understanding this connection is the first step toward addressing it.
The Physical Impact on Sexual Response
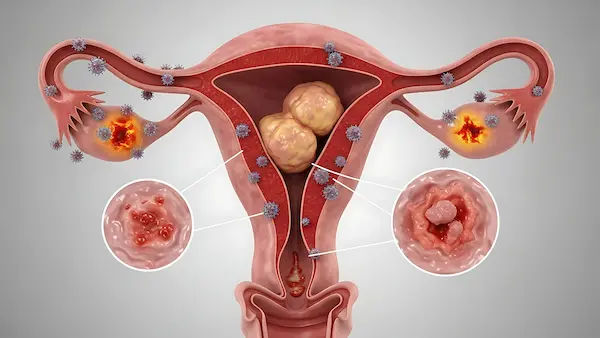
The physical side effects are often the most direct. Chemotherapy and radiation can cause fatigue that drains your energy for sex, nerve damage that reduces sensation, and hormonal changes that plummet your libido. Surgeries in pelvic areas (for prostate, bladder, colorectal, or cervical cancers) can damage nerves and blood vessels crucial for arousal and orgasm. For breast cancer patients, surgery can affect sensitivity in erogenous zones. These physical changes are real and valid, but they are also often manageable with the right approach and medical guidance. If you experience persistent physical symptoms like pain or numbness, consulting a doctor online with Apollo24|7 can be a good first step to discuss your concerns privately.
The Emotional and Psychological Toll
The impact isn't just physical. The emotional rollercoaster of a cancer diagnosis anxiety, depression, fear of recurrence, and changes in body image can significantly dampen sexual desire. You might not feel attractive or confident due to scars, weight changes, or hair loss. The stress itself can suppress the hormonal signals needed for sexual response. It's crucial to acknowledge that your mental health is deeply intertwined with your sexual health. Addressing these emotional challenges is as important as treating the physical ones.
How Different Cancer Treatments Affect Sexual Response
Each treatment modality affects the body differently, leading to unique challenges for your sexual response.
Surgery: Direct Physical Changes
Surgery can alter your body in ways that directly affect sexual function. A prostatectomy often leads to erectile dysfunction due to nerve damage. A hysterectomy can shorten the vagina or affect lubrication. Mastectomy can change how you perceive your body and experience physical touch. The key is to understand the specific physical changes caused by your surgery and work with your healthcare team to find solutions, which may include nerve-sparing surgical techniques or post-operative rehabilitation.
Chemotherapy and Radiation: Systemic Side Effects
These systemic treatments cause widespread side effects. Chemotherapy can throw you into early menopause if you're a woman, causing vaginal dryness and pain. For men, it can reduce testosterone levels, leading to low libido after chemo. Radiation to the pelvic area can cause scarring, narrowing of the vagina, or damage to blood vessels, affecting both men and women. The cumulative fatigue from these treatments often leaves little energy for sexual activity. Managing these side effects proactively, like using vaginal moisturisers during radiation, can make a significant difference.
Hormone Therapy: Shifting Your Body's Chemistry
For hormone-sensitive cancers (like breast and prostate), hormone therapy is common. These treatments work by drastically reducing oestrogen or testosterone, the very hormones that drive sexual desire. For women, this can mean intense vaginal dryness and pain during intercourse. For men, it can cause erectile dysfunction and a complete loss of libido. While these effects can be challenging, they are a known consequence of the treatment, and numerous strategies exist to manage them and maintain intimacy in other ways.
Consult a Sexologist for the best advice
Specific Challenges for Women and People Assigned Female at Birth
Women often face a distinct set of challenges related to hormonal changes and pelvic health.
Managing Vaginal Dryness and Painful Intercourse
Vaginal dryness (or vaginal atrophy) is one of the most common issues after chemo or hormone therapy. This isn't just minor discomfort; it can make penetration painful. Solutions are available:
- Vaginal Moisturisers: Used regularly (e.g., 2-3 times a week) to maintain moisture.
- Lubricants: Used during sexual activity to reduce friction.
- Vaginal Oestrogen: In some cases, low-dose local oestrogen creams or rings may be safe and effective, even for breast cancer survivors. This is a decision to make carefully with your oncologist.
Addressing Changes in Libido and Arousal
With lowered oestrogen, you may find it takes longer to become aroused, and orgasms might feel different or be harder to achieve. This is where redefining intimacy becomes crucial. Focusing on sensual touch, massage, and outercourse (sexual stimulation without penetration) can take the pressure off performance and rediscover pleasure. If your condition does not improve after trying these methods, book a physical visit to a gynaecologist with Apollo24|7 for a personalised assessment.
Specific Challenges for Men and People Assigned Male at Birth
For men, treatments often directly impact the mechanisms of erection and ejaculation.
Erectile Dysfunction After Cancer Treatment
Erectile dysfunction (ED) is very common, especially after prostate surgery or radiation. Nerve damage or reduced blood flow can prevent erections. The good news is that there are many effective treatments:
- Oral Medications (PDE5 inhibitors): Drugs like sildenafil (Viagra) can be very helpful if the nerves are intact.
- Vacuum Erection Devices: Mechanical pumps that draw blood into the penis.
Injections or Implants: More invasive but highly effective options.
Early intervention is key. "Penile rehabilitation" programs start soon after surgery to promote blood flow and preserve tissue health.
Loss of Libido and Other Sexual Concerns
Hormone therapy for prostate cancer can cause a severe drop in testosterone, leading to a loss of libido that no ED pill can fix. It's important to separate desire from performance. Intimacy can still be fulfilling without an erection or orgasm. Open communication with your partner about these changes is essential. Furthermore, treatments can affect fertility and the ability to ejaculate, which are important topics to discuss with your doctor before treatment begins.
Rebuilding Intimacy and Sexual Wellness After Cancer
Reclaiming your sexual life is a process of exploration and adaptation.
Communication is Key: Talking to Your Partner and Your Doctor
This is the most critical tool. Talk to your partner about your fears, desires, and what feels good now. Be honest and patient. Equally important is talking to your healthcare team. Many patients hesitate, but doctors are there to help. Be specific: "Since my treatment ended, I have no desire for sex, and it's causing stress in my relationship." This opens the door for targeted help, whether it's a referral to a sexual health specialist, a therapist, or a prescription.
Practical Strategies and Medical Interventions
- Start Slowly: Reintroduce intimacy without pressure. Begin with cuddling, kissing, and massage.
- Expand Your Definition of Sex: Sex is more than intercourse. Focus on sensual pleasure and emotional connection.
- Seek Professional Help: A sex therapist or counsellor specialising in cancer survivorship can provide invaluable guidance.
- Pelvic Floor Physical Therapy: For both men and women, this can help address pain and improve sexual function by strengthening pelvic muscles.
Conclusion
The journey through cancer and beyond can profoundly reshape your relationship with your body and your sexuality. While cancer treatment can undoubtedly affect your sexual response, it does not have to define your intimate life forever. By understanding the causes, communicating openly, and exploring new approaches to intimacy and pleasure, you can reclaim this important aspect of your well-being. The path may look different than before, but it can be equally, if not more, fulfilling. Remember, seeking help is a sign of strength. Take the first step today by having a conversation with your partner or reaching out to a healthcare professional who can guide you toward a future of connection and joy. If you're struggling to navigate these changes, consider consulting a specialist through Apollo24|7 to discuss a personalised plan for your sexual wellness.
Consult a Sexologist for the best advice
Consult a Sexologist for the best advice

Dr. Rohit Bhattar
Uro Oncologist
14 Years • MBBS, MS, MCh (Urology), Fellowship in Uro-oncology and Robotic Urology (United Kingdom)
Ahmedabad
Apollo Hospitals Gandhinagar, Ahmedabad
(100+ Patients)

Dr. Utsa Basu
Diabetologist
14 Years • MBBS , MD
Barasat
Diab-Eat-Ease, Barasat
(75+ Patients)

Dr. Rik Sadhukhan
Ayurveda Practitioner
8 Years • BAMS
Kolkata
Vedhive Ayurveda, Ballygunge, Kolkata

Dr. Anjan Das
Ayurveda Practitioner
8 Years • Ayurvedacharya ( B.A.M.S )
Dumdum
Vedhive Ayurveda Clinic, Dumdum

Dr. Shiv Prakash Singh
Ayurveda Practitioner
19 Years • BAMS
Kolkata
Vedhive Ayurveda College Street, Kolkata
Consult a Sexologist for the best advice

Dr. Rohit Bhattar
Uro Oncologist
14 Years • MBBS, MS, MCh (Urology), Fellowship in Uro-oncology and Robotic Urology (United Kingdom)
Ahmedabad
Apollo Hospitals Gandhinagar, Ahmedabad
(100+ Patients)

Dr. Utsa Basu
Diabetologist
14 Years • MBBS , MD
Barasat
Diab-Eat-Ease, Barasat
(75+ Patients)

Dr. Rik Sadhukhan
Ayurveda Practitioner
8 Years • BAMS
Kolkata
Vedhive Ayurveda, Ballygunge, Kolkata

Dr. Anjan Das
Ayurveda Practitioner
8 Years • Ayurvedacharya ( B.A.M.S )
Dumdum
Vedhive Ayurveda Clinic, Dumdum

Dr. Shiv Prakash Singh
Ayurveda Practitioner
19 Years • BAMS
Kolkata
Vedhive Ayurveda College Street, Kolkata
More articles from Cancer
Frequently Asked Questions
How long after cancer treatment will my sexual function return to normal?
There's no single timeline. It depends on the type and duration of treatment, your overall health, and your age. For some, function improves within months; for others, it may take a year or more, or a 'new normal' may need to be established. Patience and proactive management are key.
Are there any safe medications or supplements to improve libido after cancer?
Always consult your oncologist before taking any new supplement, as some can interfere with treatment or recovery. For libido, addressing underlying issues like fatigue or depression is often the first step. Prescription medications exist but must be carefully evaluated for your specific cancer history.
Is it safe to have sex during chemotherapy or radiation?
It can be, but you need to take precautions. Your immunity may be low, so protection against infection is important. If you have a partner, using condoms can protect them from exposure to chemotherapy drugs excreted in bodily fluids. Always check with your medical team for specific guidance.
What can I do if penetration is painful after radiation therapy?
Vaginal dilators, used regularly, can help prevent the vagina from narrowing and becoming less flexible. Using a high-quality lubricant and moisturiser is essential. A pelvic floor physical therapist can provide specialised techniques to manage pain during intercourse.
My partner is a cancer survivor and has no interest in sex. How can I support them?
Focus on emotional intimacy without pressure. Express your love and affection through non-sexual touch, conversation, and shared activities. Encourage open communication and suggest attending a doctor's appointment together to discuss options as a team, showing your support.