Endometriosis Diagnosis and Treatment A Comprehensive Guide
Know about endometriosis, what it is, signs, symptoms, causes, diagnosis, treatment options and how to live well with endometriosis and more.

Introduction
For millions of women and individuals assigned female at birth, severe period pain is often dismissed as "normal." Endometriosis is a complex and often misunderstood disorder where tissue similar to the uterine lining grows outside the uterus, causing inflammation, scar tissue, and immense pain. The path to an endometriosis diagnosis is notoriously long, averaging 7-10 years from symptom onset. This delay can be frustrating and isolating. This comprehensive guide demystifies the journey, explaining the symptoms that should prompt a doctor's visit, the steps involved in reaching a definitive diagnosis, and the multifaceted treatment options available to manage the condition and reclaim your quality of life.
What is Endometriosis? Beyond "Bad Periods"
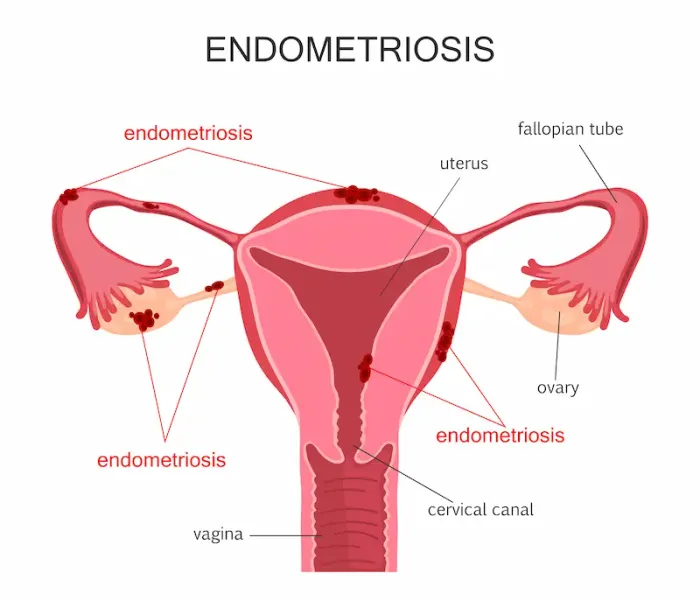
Endometriosis is far more than just a painful period. It is a full-body inflammatory condition where tissue resembling the endometrium (the lining of the uterus) implants and grows in places it shouldn't, most commonly on the ovaries, fallopian tubes, the outer surface of the uterus, and the pelvic lining. Unlike the uterine lining that sheds during menstruation, this misplaced tissue has no way to exit the body. This leads to internal bleeding, inflammation, the formation of scar tissue (adhesions), and painful lesions. These adhesions can bind pelvic organs together, causing chronic pain and fertility issues. Understanding that it's a systemic disease, not just a gynaecological one, is the first step toward effective management and treatment.
Consult a Gynaecologist for Personalised Advice
How Endometriosis Tissue Behaves
This rogue tissue acts similarly to the uterine lining—it thickens, breaks down, and bleeds with each menstrual cycle. However, because it's trapped inside the body, it irritates the surrounding tissues, triggering a chronic inflammatory response. This process can eventually develop into scar tissue and cysts (known as endometriomas or "chocolate cysts" on the ovaries). The inflammation can also produce chemicals that irritate nearby nerve endings, directly causing the severe pain associated with the condition.
Recognising the Signs: Symptoms That Lead to Suspicion
The symptoms of endometriosis are varied and can mimic other conditions like irritable bowel syndrome (IBS) or pelvic inflammatory disease (PID), which is a primary reason for diagnostic delays. Paying attention to your body is crucial.
The Classic Symptom: Debilitating Pelvic Pain
The most common symptom is chronic pelvic pain, often directly correlated with the menstrual cycle. However, pain is not limited to periods. Many experiences:
1. Dysmenorrhea: Extremely painful menstrual cramps that worsen over time and aren't relieved by standard painkillers.
2. Chronic Pelvic Pain: Aching or cramping throughout the month, not just during menstruation.
3. Dyspareunia: Pain during or after sexual intercourse.
4. Pain with Bowel Movements or Urination: Most common during menstrual periods.
Beyond Pain: Gastrointestinal and Urinary Symptoms
Endometriosis implants on the bowel or bladder can cause a range of issues often mistaken for other ailments, including:
1. Bloating, constipation, diarrhoea, or nausea, especially around your period (often called "endo belly").
2. Painful urination or blood in the urine during menstruation.
3. Fatigue, lethargy, and a general feeling of being unwell.
The Heartbreaking Link: Endometriosis and Infertility
For many, the first sign of a problem is difficulty getting pregnant. It's estimated that 30-50% of women with endometriosis may experience infertility. The inflammation and scar tissue can distort pelvic anatomy, impair egg quality, block fallopian tubes, or disrupt implantation. Importantly, not everyone with endometriosis is infertile, and many treatment paths can help achieve pregnancy.
The Diagnostic Odyssey: Why It Often Takes Years
Receiving a formal endometriosis diagnosis can feel like an odyssey. There is no simple blood test or non-invasive scan that can definitively confirm it, leading to a process of elimination.
The Initial Consultation and Medical History
This is the most critical step. Be prepared to detail your symptoms meticulously. A doctor may ask you to keep a symptom diary tracking your pain levels, cycle, bowel habits, and other issues. This history often provides the strongest clues. If your condition does not improve after trying over-the-counter methods, book a physical visit to a doctor with Apollo24|7 for a thorough evaluation.
The Physical and Pelvic Examination
During a pelvic exam, your doctor will manually feel (palpate) areas in your pelvis for abnormalities, such as cysts on your ovaries or scars behind your uterus. However, it's often normal unless there are large cysts or significant scarring.
Imaging Tests - Ultrasound and MRI
1. Transvaginal Ultrasound: This test uses sound waves to create images of your reproductive organs. It can identify endometriomas (ovarian cysts associated with endometriosis), but it often cannot see superficial implants or adhesions.
2. Magnetic Resonance Imaging (MRI): An MRI scan can provide more detailed images and may help in planning surgery by identifying deeper implants, but it is not a definitive diagnostic tool.
Can Ultrasound Diagnose Endometriosis?
While a transvaginal ultrasound is a valuable tool, it cannot rule out endometriosis. A "normal" ultrasound does not mean you don't have the condition. It is best at detecting endometriotic cysts (endometriomas) on the ovaries.
The Gold Standard - Diagnostic Laparoscopy
The only way to confirm and formally diagnose endometriosis is through a minimally invasive surgical procedure called laparoscopy. A surgeon inserts a tiny camera through a small incision in the abdomen to visually identify the presence, location, and extent of endometrial implants and scar tissue. This procedure also allows for simultaneous treatment, as the surgeon can often remove the tissue during the same operation.
Navigating Your Treatment Options: From Management to Surgery
There is no absolute cure for endometriosis, but highly effective treatments can manage pain and improve fertility. The approach is highly personalised based on symptom severity, future pregnancy plans, and age.
Goal-Oriented Treatment: Pain Relief vs. Fertility
Your treatment path depends on your primary goal:
1. For Pain Management: The focus is on reducing inflammation and suppressing estrogen, which fuels endometrial growth.
2. For Fertility: The focus shifts to surgically removing implants and scar tissue to restore anatomy, followed by fertility treatments.
Pharmaceutical Options: Pain Meds and Hormonal Therapy
1. Pain Medications: NSAIDs like ibuprofen or naproxen are first-line for managing pain and inflammation.
2. Hormonal Therapies: These aim to reduce or eliminate menstruation, slowing endometrial tissue growth.
• Hormonal Birth Control: Pills, patches, or rings to make periods lighter and less painful.
• Gonadotropin-releasing hormone (GnRH) agonists and antagonists: These induce a temporary medical menopause to shrink implants.
• Progestin Therapy: IUDs, implants, or pills that can halt periods and slow tissue growth.
Surgical Intervention: Laparoscopic Excision and Ablation
• Laparoscopic Excision Surgery: Considered the gold standard treatment, this involves cutting out (excising) the endometriosis implants and scar tissue completely while preserving healthy organs. This offers the best long-term pain relief.
• Ablation: This involves destroying the surface of the implants with a laser or electric current. It is less effective than excision for deep infiltrating disease, as it may not remove tissue buried deeper.
Hysterectomy: Is It a Cure for Endometriosis?
A hysterectomy (removal of the uterus), sometimes with removal of the ovaries (oophorectomy), is a last-resort option for severe cases when other treatments have failed. It is not a guarantee of a cure, especially if endometriosis implants remain outside the uterus. This decision is major and irreversible, so it requires extensive discussion with your doctor.
Living Well with Endometriosis: Holistic Management Strategies
Medical treatment is one pillar of management. A holistic approach can significantly improve daily life.
Diet and Nutrition for Inflammation Reduction
While no specific diet cures endometriosis, an anti-inflammatory diet may help manage symptoms. This includes reducing red meat, gluten, and processed foods while increasing intake of omega-3 fatty acids (found in fish), fibre-rich fruits and vegetables, and iron-rich leafy greens to combat anaemia from heavy bleeding.
The Role of Physical Therapy and Gentle Exercise
Pelvic floor physical therapy is a game-changer for many. Endometriosis causes pelvic muscles to become incredibly tight and painful (a condition called hypertonic pelvic floor). A specialist can teach exercises and techniques to release these muscles, reducing pain. Gentle exercises like walking, yoga, and swimming can also help manage pain and reduce stress.
Mental Health and Building a Support System
Living with a chronic, invisible illness is emotionally taxing. Therapy, counselling, and support groups (online or in-person) can provide crucial emotional tools and reduce feelings of isolation. Connecting with others who understand the struggle is invaluable.
Conclusion
The path to an endometriosis diagnosis and treatment is often long and challenging, but it is a journey toward validation and reclaiming control over your life and health. Understanding the symptoms from debilitating pelvic pain to gastrointestinal distress and infertility empowers you to advocate for yourself with healthcare providers. While the diagnostic process, culminating in laparoscopy, may seem daunting, it is the crucial step toward accessing effective treatment options, whether hormonal, surgical, or holistic. If you suspect you have symptoms, take the first step and consult a healthcare professional for a personalised evaluation.
Consult a Gynaecologist for Personalised Advice
Consult a Gynaecologist for Personalised Advice

Dr. Abhishek Daga
Obstetrician and Gynaecologist
20 Years • MBBS, MS (Obstetrics & Gynaecology)
Kolkata
Gynae Care Fertility Centre, Kolkata
(150+ Patients)

Dr Divya G
Obstetrician and Gynaecologist
13 Years • MBBS, MS (OG) ,MRCOG( U.K),FMAS
Chennai
Apollo Medical Centre Kotturpuram, Chennai

Dr. Vineet Mishra
Infertility Specialist
36 Years • MD, Phd, DSc
Ahmedabad
Apollo Hospitals - Gandhinagar, Ahmedabad, Ahmedabad

Dr. Sreeparna Roy
Obstetrician and Gynaecologist
8 Years • MBBS , MS (OBSTETRICS & GYNAECOLOGY), Fellowship in Infertility, Endoscopy & Ultrasonography), Fellowship in Laparoscopy & Hysteroscopy,DRM
Kolkata
Dr Utsa Basu Clinic, Kolkata

Dr. Saraswathi Girish
Obstetrician and Gynaecologist
21 Years • MBBS , DNB,FRM(Fellowship in Reproductive Medicine)
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru
Consult a Gynaecologist for Personalised Advice

Dr. Abhishek Daga
Obstetrician and Gynaecologist
20 Years • MBBS, MS (Obstetrics & Gynaecology)
Kolkata
Gynae Care Fertility Centre, Kolkata
(150+ Patients)

Dr Divya G
Obstetrician and Gynaecologist
13 Years • MBBS, MS (OG) ,MRCOG( U.K),FMAS
Chennai
Apollo Medical Centre Kotturpuram, Chennai

Dr. Vineet Mishra
Infertility Specialist
36 Years • MD, Phd, DSc
Ahmedabad
Apollo Hospitals - Gandhinagar, Ahmedabad, Ahmedabad

Dr. Sreeparna Roy
Obstetrician and Gynaecologist
8 Years • MBBS , MS (OBSTETRICS & GYNAECOLOGY), Fellowship in Infertility, Endoscopy & Ultrasonography), Fellowship in Laparoscopy & Hysteroscopy,DRM
Kolkata
Dr Utsa Basu Clinic, Kolkata

Dr. Saraswathi Girish
Obstetrician and Gynaecologist
21 Years • MBBS , DNB,FRM(Fellowship in Reproductive Medicine)
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru
More articles from Endometriosis
Frequently Asked Questions
1. At what age does endometriosis usually start?
Symptoms most commonly begin during adolescence, shortly after a person starts their period. However, due to diagnostic delays, it is often not officially diagnosed until a person is in their 20s or 30s.
2. Can you have endometriosis with a normal ultrasound?
Yes, absolutely. A normal ultrasound does not rule out endometriosis. Ultrasound is good at spotting cysts (endometriomas) but often misses superficial implants and adhesions. Laparoscopy is required for a definitive diagnosis.
3. What is the best pain relief for endometriosis flare-ups?
Over-the-counter NSAIDs (like ibuprofen or naproxen) are often the first line of defense for managing inflammation and pain. For severe pain, a doctor may prescribe stronger medications. Heat therapy (heating pads) is also very effective for relaxing pelvic muscles and relieving cramping.
4. Does pregnancy cure endometriosis?
No, pregnancy is not a cure. The high levels of progesterone during pregnancy can suppress the activity of endometrial implants, leading to a temporary relief of symptoms for some people. However, symptoms typically return after childbirth and the return of menstrual cycles.
5. What is the difference between endometriosis and adenomyosis?
They are sister conditions but located in different places. Endometriosis is when the tissue grows outside the uterus. Adenomyosis is when similar tissue grows into the muscular wall of the uterus. It is possible to have both conditions simultaneously.