Pressure Inside Your Eyes: The Silent Threat to Your Optic Nerve
Learn how intraocular pressure affects your eyes, why it threatens the optic nerve, and how early detection of glaucoma can protect your vision.

Written by Dr. J T Hema Pratima
Reviewed by Dr. Dhankecha Mayank Dineshbhai MBBS
Last updated on 13th Jan, 2026
Introduction
Have you ever considered the pressure inside your eyes? Unlike a headache or muscle strain, this isn't something you can feel, yet it plays a critical role in one of your most precious senses: your sight. Healthy eyes maintain a delicate balance of fluid, creating a stable pressure that keeps the eyeball properly formed and functioning. However, when this balance is disrupted and pressure inside the eyes rises, it can silently compress and damage the optic nerve—the vital cable that transmits visual information from your eye to your brain. This damage, known as glaucoma, is a leading cause of irreversible blindness worldwide. The insidious part? It often progresses with no symptoms until significant, permanent vision loss has occurred. This guide will demystify intraocular pressure, explain how it threatens your optic nerve, and arm you with the knowledge to protect your vision for years to come.
What is Intraocular Pressure (IOP) and Why Does It Matter?
Intraocular pressure (IOP) is the fluid pressure inside your eye. Think of your eye as a ball that needs to be inflated to maintain its shape and allow light to focus correctly. This pressure is maintained by a clear fluid called aqueous humour, which circulates in the front part of your eye.
The Delicate Balance: Aqueous Humour Production and Drainage
Your eye is a marvel of constant renewal. The ciliary body behind your iris continuously produces aqueous humour. This fluid flows forward, nourishing the lens and cornea, and then must drain out through a tiny, spongy meshwork called the trabecular meshwork, located at the angle where the iris and cornea meet. A healthy eye maintains a perfect equilibrium between how much fluid is produced and how much is drained. High intraocular pressure occurs when this drainage system doesn't function properly, causing fluid to build up—much like a sink with a clogged drain.
How is Eye Pressure Measured? Understanding the Numbers
During a comprehensive eye exam, an ophthalmologist measures your IOP using a test called tonometry. The most common method uses a quick puff of air onto the surface of your eye (non-contact tonometry), while another method involves gently touching the eye's surface with a small device after numbing it with drops (applanation tonometry).
Pressure is measured in millimetres of mercury (mmHg). The generally accepted normal eye pressure range is between 10 and 21 mmHg. However, this is not a universal rule. Some people can have pressures above 21 mmHg without any signs of damage (ocular hypertension), while others can develop glaucoma with pressures in the normal range (normal-tension glaucoma). This is why a full optic nerve examination is crucial.
When Pressure Becomes a Problem: From Ocular Hypertension to Glaucoma
Not everyone with high eye pressure develops glaucoma, but it is the single biggest risk factor. It's important to distinguish between the two conditions.
What is Ocular Hypertension? (High Pressure Without Damage)
Ocular hypertension simply means your intraocular pressure is consistently higher than normal, but an ophthalmologist detects no signs of optic nerve damage or vision loss. Think of it as a warning sign. Individuals with ocular hypertension are considered "glaucoma suspects" and require regular monitoring to ensure the elevated pressure doesn't begin to cause damage over time.
What is Glaucoma? (The Optic Nerve Damage)
Glaucoma is not just high eye pressure; it is an eye disease characterised by specific damage to the optic nerve. This nerve is a bundle of over a million nerve fibres that acts like an internet cable, carrying images from the retina to the brain. Sustained high pressure inside the eyes compresses and damages these fragile nerve fibres, leading to their gradual death.
Consult a Ophthalmologist for the best advice
Open-Angle Glaucoma: The Most Common Type
This form accounts for at least 90% of cases. The drainage angle where the iris and cornea meet remains "open," but the trabecular meshwork becomes less efficient at draining fluid over time. Pressure builds slowly and painlessly, causing gradual peripheral vision loss.
Angle-Closure Glaucoma: A Medical Emergency
This less common type occurs when the iris bulges forward, suddenly blocking the drainage angle. Fluid can't escape, causing a rapid, painful increase in pressure. Symptoms include severe eye pain, headache, nausea, vomiting, and blurred vision. This is an acute attack requiring immediate medical attention to prevent permanent blindness.
How High Pressure Damages the Optic Nerve
The mechanism by which high IOP causes harm is twofold: direct mechanical compression and reduced blood flow.
The Mechanism of Damage: Compression and Blood Flow
The optic nerve head is the weakest point in the eye's coat. When pressure inside the eyes rises, it physically pushes against this sensitive area. This compression:
- Directly Crushes Nerve Fibres: The high force mechanically damages and kills the delicate axons of the retinal ganglion cells that make up the optic nerve.
- Impairs Blood Flow: The elevated pressure can also compress the tiny blood vessels that supply the optic nerve head with oxygen and nutrients. This ischaemic insult starves the nerve cells, further accelerating their demise.
The Progressive Nature of Vision Loss in Glaucoma
The damage occurs gradually and peripherally first. The nerve fibres that carry information from your side vision are typically affected first. You might not notice this slow loss, as your brain is remarkably good at compensating. Over years, the field of vision narrows, creating "tunnel vision." If the entire optic nerve is destroyed, it results in complete blindness. This damage is irreversible, which is why early detection is paramount.
Symptoms: Why Glaucoma is the "Silent Thief of Sight"
The Lack of Early Warning Signs
Primary open-angle glaucoma has no early symptoms. There is no pain, redness, or noticeable change in vision in its initial stages. The only way to detect it before significant damage occurs is through a comprehensive, dilated eye exam performed by an eye care professional.
Recognising Symptoms of Advanced Glaucoma and Acute Attacks
As glaucoma progresses, symptoms may include:
- Gradual loss of peripheral vision, usually in both eyes.
- Tunnel vision in the advanced stages.
In the case of an acute angle-closure attack, symptoms are severe and sudden:
- Intense eye pain and headache
- Nausea and vomiting
- Seeing haloes around lights
- Sudden blurred vision
- Eye redness
This is a medical emergency. Seek immediate care.
Who is at Risk? Key Risk Factors for High Eye Pressure
While anyone can develop glaucoma, certain factors significantly increase your risk:
- Age: Being over 60.
- Race: African-Caribbeans and Hispanics are at higher risk for open-angle glaucoma, and Asians are at higher risk for angle-closure glaucoma.
- Family History: Having a parent or sibling with glaucoma.
- Medical Conditions: Diabetes, high blood pressure, heart disease, and sickle cell anaemia.
- Eye Conditions: Severe eye injury, certain retinal diseases, extreme short-sightedness or long-sightedness.
- Prolonged Corticosteroid Use: Especially corticosteroid eye drops.
How is High Eye Pressure and Glaucoma Diagnosed?
A simple eye pressure test is not enough. Diagnosis requires a comprehensive eye exam that includes:
The Comprehensive Dilated Eye Exam
Drops are used to widen your pupils, allowing the doctor a clear view of your retina and optic nerve.
Tonometry: The Pressure Test
The measurement of your intraocular pressure.
Ophthalmoscopy and Imaging: Examining the Optic Nerve
The doctor examines the colour and shape of your optic nerve for signs of damage, such as increased cupping. Advanced imaging like OCT (Optical Coherence Tomography) can measure the thickness of the nerve fibre layer around the nerve with incredible precision, detecting damage before it affects your vision.
Perimetry: The Visual Field Test
This test maps your complete field of vision, spotting the subtle patterns of peripheral vision loss characteristic of glaucoma.
If you have one or more risk factors, scheduling a comprehensive dilated eye exam is the most important step you can take. You can consult an ophthalmologist online with Apollo24|7 to discuss your risk and book an in-person examination.
Treatment Options: Lowering Pressure to Protect Your Vision
While damaged vision cannot be restored, all current treatments aim to lower eye pressure to prevent further damage to the optic nerve.
Prescription Eye Drops: The First Line of Defence
These are the most common initial treatment. They work either by reducing the production of aqueous humour or by improving its outflow through the drainage angle. Consistency is critical—they must be used daily as prescribed.
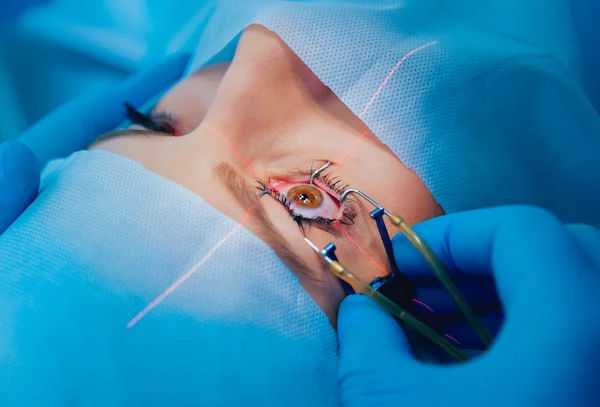
Laser Therapy: Trabeculoplasty and Iridotomy
- Laser Trabeculoplasty: Used for open-angle glaucoma. The laser applies tiny burns to the trabecular meshwork, which helps increase drainage.
- Laser Iridotomy: Used for angle-closure glaucoma. The laser creates a tiny hole in the iris to improve fluid flow and prevent an acute attack.
Surgical Procedures: Trabeculectomy and MIGS
When drops and laser are insufficient, surgery can create a new drainage channel for fluid to leave the eye.
- Trabeculectomy: A traditional surgery creating a new drainage flap.
- MIGS (Minimally Invasive Glaucoma Surgery): A newer category of procedures that use microscopic devices and incisions to reduce pressure with a higher safety profile and faster recovery time.
Can You Prevent High Eye Pressure?
You cannot prevent glaucoma itself, but you can prevent vision loss from it. The key is early detection and treatment.
- Get Regular Comprehensive Eye Exams: This is non-negotiable. The American Academy of Ophthalmology recommends a baseline exam at age 40, with follow-ups as recommended by your doctor. Those with risk factors may need to start earlier and be seen more frequently.
- Know Your Family History.
- Exercise Safely: Regular, moderate exercise may help reduce IOP.
- Protect Your Eyes: Use protective eyewear to prevent serious injury.
- Manage Systemic Health: Control conditions like diabetes and hypertension.
Conclusion
The pressure inside your eyes is a silent metric of your ocular health, and its imbalance poses a grave threat to the intricate optic nerve. Understanding that glaucoma is a sneak thief, robbing you of sight without warning, empowers you to take proactive steps. The journey to preserving your vision begins with awareness and is secured through action—specifically, scheduling regular, comprehensive eye exams. These exams are the singular most effective tool we have to catch elevated pressure and early nerve damage in their tracks. If you are diagnosed, modern treatments are highly effective at managing intraocular pressure and halting the disease's progression. Don't wait for symptoms to appear; by then, it's often too late. Prioritise your eye health today to safeguard your vision for all your tomorrows. If it's been over two years since your last exam, or if you have any risk factors, consult an eye specialist online with Apollo24|7 to book an appointment.
Consult a Ophthalmologist for the best advice
Consult a Ophthalmologist for the best advice

Dr. Zennat Tajmin Shah
Ophthalmologist
24 Years • MBBS,DNB (Ophthalmology)
Kolkata
Titanium Eye Care, Kolkata

Dr. Karan Paswan
Ophthalmologist
7 Years • MBBS,MS (Ophthalmology)
Kolkata
VDC Clinic, Kolkata
Dr Aishwarya M Angadi
Ophthalmologist
5 Years • MBBS, MS
Pune
Apollo Clinic, Nigdi, Pune
Dr Kanse Vaibhav
Ophthalmologist
10 Years • MBBS, DO, MS, DNB
Pune
Apollo Clinic, Nigdi, Pune
Dr. Monika Sharma
Ophthalmologist
10 Years • ENT/ Otorhinolaryngologist
Gurugram
Apollo Cradle, Miracles, Gurugram Sector 82, Gurugram
Consult a Ophthalmologist for the best advice

Dr. Zennat Tajmin Shah
Ophthalmologist
24 Years • MBBS,DNB (Ophthalmology)
Kolkata
Titanium Eye Care, Kolkata

Dr. Karan Paswan
Ophthalmologist
7 Years • MBBS,MS (Ophthalmology)
Kolkata
VDC Clinic, Kolkata
Dr Aishwarya M Angadi
Ophthalmologist
5 Years • MBBS, MS
Pune
Apollo Clinic, Nigdi, Pune
Dr Kanse Vaibhav
Ophthalmologist
10 Years • MBBS, DO, MS, DNB
Pune
Apollo Clinic, Nigdi, Pune
Dr. Monika Sharma
Ophthalmologist
10 Years • ENT/ Otorhinolaryngologist
Gurugram
Apollo Cradle, Miracles, Gurugram Sector 82, Gurugram
More articles from Eye Problem
Frequently Asked Questions
What is considered a dangerous eye pressure level?
There's no single 'dangerous' number for everyone. While 21 mmHg is the upper threshold of normal, a pressure of 22 mmHg might be harmful for one person but not for another. The danger level is determined by how much pressure your individual optic nerve can tolerate without being damaged, which is why a full examination is essential.
Can you feel high eye pressure?
Typically, no. Open-angle glaucoma, the most common type, causes no pain or noticeable symptoms in its early stages. You cannot 'feel' your intraocular pressure rising. The only exception is during an acute angle-closure attack, which is painful and a medical emergency.
Are there any natural ways to reduce eye pressure?
While medical treatment is necessary for diagnosed glaucoma, some lifestyle changes may support eye health. Regular, aerobic exercise (e.g., brisk walking, jogging) can slightly lower IOP. A healthy diet rich in leafy greens and omega-3s is beneficial. However, these should never replace prescribed treatment. Always discuss any new regimens with your doctor.
What is the difference between ocular hypertension and glaucoma?
Ocular hypertension means your eye pressure is higher than normal, but your optic nerve shows no signs of damage. Glaucoma means that high pressure (or sometimes normal pressure) has already caused damage to the optic nerve, resulting in vision loss. Everyone with glaucoma has a pressure problem, but not everyone with high pressure has glaucoma.
How often should I get my eyes checked for glaucoma?
The American Academy of Ophthalmology recommends a baseline comprehensive eye exam at age 40. Based on the results, your doctor will recommend a schedule. If you have no risk factors, every 2-4 years may be sufficient. If you have risk factors, you may need exams every 1-2 years or even more frequently after age 55.