Guide to Prostate Diseases And Its Management
Understand prostate diseases, their causes, symptoms, and treatment options. Learn about effective management approaches for better prostate health.

Written by Dr. Shaik Abdul Kalam
Reviewed by Dr. Dhankecha Mayank Dineshbhai MBBS
Last updated on 13th Jan, 2026
Navigating prostate health can feel overwhelming, especially with the wealth of sometimes conflicting information available. Whether you're experiencing symptoms yourself or are concerned about a loved one, understanding the basics of prostate diseases is the first step toward effective management and peace of mind. The prostate, a small walnut-shaped gland, plays a crucial role in male reproductive health, but it's also prone to issues as men age. This guide will demystify the three primary conditions like Benign Prostatic Hyperplasia (BPH), prostatitis, and prostate cancer, breaking down their symptoms, diagnosis processes, and the wide range of management strategies available. Our goal is to empower you with knowledge, so you can have informed conversations with your doctor and take proactive control of your health.
Understanding the Prostate Gland
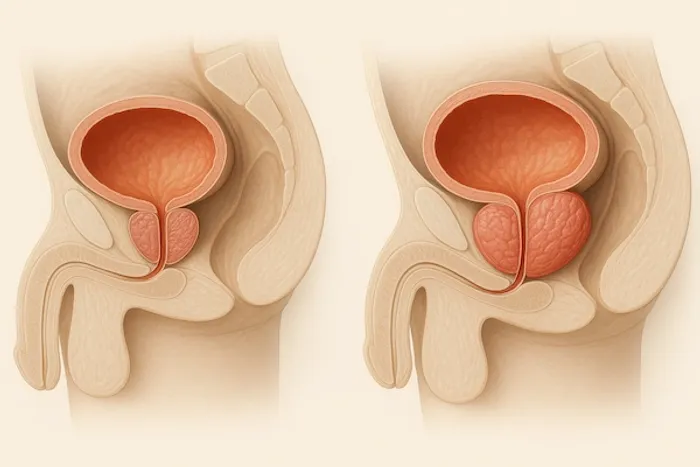
The prostate is a small gland located just below the bladder and in front of the rectum in men. It surrounds the urethra, the tube through which urine and semen exit the body. Its primary function is to produce fluid that nourishes and transports sperm, making it a key component of the male reproductive system.
Why Prostate Health Matters as You Age
For most young men, the prostate causes no issues. However, around age 40-50, the gland often begins to enlarge, a natural process of aging. This growth can lead to various conditions that impact urinary and sexual function. Prioritizing prostate health through awareness and regular check-ups is essential for maintaining quality of life in later years.
Consult a Top Specialist
Common Prostate Diseases: An Overview
Below are a few common prostate diseases,
Benign Prostatic Hyperplasia (BPH) - The Enlarged Prostate
BPH is a non-cancerous enlargement of the prostate. It is extremely common, affecting about 50% of men by age 60 and up to 90% by age 85. Because the prostate surrounds the urethra, its growth squeezes this tube, leading to bothersome urinary symptoms of BPH like a weak stream, urgency, and frequent nighttime urination (nocturia).
Prostatitis - Inflammation and Infection
Prostatitis refers to the inflammation of the prostate gland. Unlike BPH, it's not always related to age and can affect younger men. It can be caused by a bacterial infection (acute or chronic bacterial prostatitis) or be non-bacterial (chronic pelvic pain syndrome). Symptoms often include pelvic pain, painful urination, and flu-like symptoms in acute cases.
Prostate Cancer - Causes and Risk Factors
Prostate cancer is one of the most common cancers in men. It occurs when cells in the prostate mutate and multiply uncontrollably. Key risk factors include age (risk increases significantly after 50), family history, and race (African-American men are at higher risk). While often slow-growing, early detection is critical for successful treatment options for chronic prostatitis and cancer alike.
Recognizing the Symptoms: When to See a Doctor
Below are a few symptoms,
Urinary Symptoms of BPH
The signs of an enlarged prostate are primarily urinary. Watch for:
A weak or interrupted urine stream.
A feeling of not completely emptying the bladder.
Dribbling at the end of urination.
Increased frequency of urination, especially at night (nocturia).
Urgency or difficulty starting urination.
Painful Signs of Prostatitis
Prostatitis symptoms can be acute and severe or chronic and nagging:
Pain or burning sensation during urination (dysuria).
Pain in the groin, lower abdomen, or lower back.
Painful ejaculation.
Flu-like symptoms with fever and chills (in acute bacterial prostatitis).
Early Warning Signs of Prostate Cancer
Early-stage prostate cancer may cause no symptoms. When symptoms do appear, they can mimic BPH, including urinary difficulties. More advanced cancer might cause blood in the urine or semen, erectile dysfunction, or pain in the hips, back, or chest. If symptoms persist beyond two weeks, consult a doctor online with Apollo24|7 for further evaluation.
Getting a Diagnosis: The Steps to Clarity
Below are a few ways of getting prostate diseases diagnosed,
The Digital Rectal Exam (DRE) Explained
A DRE is a quick, in-office procedure where a doctor inserts a gloved, lubricated finger into the rectum to feel the back of the prostate. It allows them to assess the gland's size, shape, and texture and check for any hard lumps or abnormalities that might suggest cancer.
The PSA Test: Understanding Your Numbers
The Prostate-Specific Antigen (PSA) test is a blood test that measures the level of PSA, a protein produced by the prostate. Elevated levels can indicate BPH, prostatitis, or prostate cancer. It's not a perfect test, but it's a crucial screening tool. Your doctor will interpret the results in the context of your age, prostate size, and other factors. Apollo24|7 offers convenient home collection for tests like PSA, making monitoring your levels easier.
Advanced Diagnostics: MRI and Biopsy
If initial tests suggest a problem, further steps may include:
MRI Fusion Biopsy: An advanced imaging technique that creates a detailed map of the prostate, allowing for more precise targeting of suspicious areas during a biopsy.
Biopsy: A procedure where small samples of prostate tissue are removed (usually with a needle) and examined under a microscope for cancer cells. This is the only definitive way to diagnose prostate cancer.
Managing Benign Prostatic Hyperplasia (BPH)
Below are a few ways of managing benign prostatic hyperplasia,
Lifestyle Changes for BPH Relief
Mild symptoms can often be managed with simple changes:
Reducing intake of caffeine and alcohol, especially in the evening.
Avoiding fluids a few hours before bedtime.
Bladder training techniques and double voiding.
Medications for Shrinking the Prostate
Two main classes of drugs are used:
1. Alpha-blockers (e.g., Tamsulosin): Relax prostate and bladder neck muscles to improve urine flow.
2. 5-alpha reductase inhibitors (e.g., Finasteride): Shrink the prostate gland by blocking the hormone that causes its growth.
Minimally Invasive Procedures for BPH
For men who don't respond to medication, several minimally invasive options can relieve symptoms without major surgery, such as Rezūm Water Vapor Therapy or UroLift.
TURP: The Gold Standard Surgery
Transurethral Resection of the Prostate (TURP) is the most common surgery for BPH. A surgeon uses an instrument inserted through the urethra to trim away excess prostate tissue. It is highly effective but can have side effects like retrograde ejaculation.
Treating Prostatitis: Beating the Inflammation
Below are a few ways of treating prostatis,
Antibiotics for Bacterial Prostatitis
A course of antibiotics is the primary treatment for bacterial prostatitis. Acute infections may require a few weeks of medication, while chronic bacterial prostatitis can require a longer course, sometimes lasting several months.
Managing Chronic Pelvic Pain Syndrome
This complex condition is trickier to treat as there's no infection. A multi-faceted approach is often needed, including:
Alpha-blocker medications.
Anti-inflammatory drugs.
Physical therapy to relax pelvic floor muscles.
Stress management and warm sitz baths.
Prostate Cancer Treatment Pathways
Treatment is highly personalized, depending on the cancer's aggressiveness (Gleason score), stage, and the patient's age and overall health.
Active Surveillance for Low-Risk Cancer
For slow-growing, early-stage cancers, immediate treatment may cause more harm than good. Active surveillance involves closely monitoring the cancer with regular PSA tests, DREs, and occasional biopsies, only treating if the cancer shows signs of progression.
Radical Prostatectomy: Surgical Removal
This surgery involves removing the entire prostate gland and some surrounding tissue. It is a common curative option for localized cancer. Techniques now include robotic-assisted surgery, which offers greater precision and potentially faster recovery.
Radiation Therapy Options
Radiation uses high-energy beams to kill cancer cells. It can be delivered externally (External Beam Radiation) or internally via radioactive seeds implanted in the prostate (Brachytherapy). It is often used as a primary treatment or after surgery.
Hormone Therapy and Emerging Treatments
For advanced cancer, hormone therapy aims to stop the body from producing testosterone, which fuels cancer growth. Newer emerging treatments for advanced prostate cancer include immunotherapy, targeted therapy, and precision medicine, which are changing the outlook for many men.
Prevention and Proactive Prostate Health
Below are a few ways for prevention and proactive prostate health,
Diet and Nutrition for a Healthy Prostate
While no diet guarantees prevention, evidence suggests a heart-healthy diet is also a prostate-healthy diet. Focus on:
Lycopene: Found in cooked tomatoes, watermelon, and grapefruit.
Cruciferous Vegetables: Broccoli, cauliflower, and Brussels sprouts.
Healthy Fats: Especially omega-3s from fish like salmon.
Soy and Legumes.
Limit red meat and high-fat dairy products.
The Role of Regular Exercise
Regular physical activity helps maintain a healthy weight, reduces inflammation, and is linked to a lower risk of BPH and aggressive prostate cancer. Aim for at least 30 minutes of moderate exercise most days of the week.
Importance of Regular Screening and Check-ups
Open communication with your doctor is vital. Discuss your risk factors and the pros and cons of PSA screening starting at age 50 (or earlier if you have a family history or are African-American). If your condition does not improve after trying these methods, book a physical visit to a doctor with Apollo24|7 for a comprehensive evaluation.
Living Well with a Prostate Condition
Managing Side Effects of Treatment
Treatments for prostate diseases, especially cancer, can cause side effects like urinary incontinence and erectile dysfunction. These are often manageable with pelvic floor exercises (Kegels), medications, devices, or counseling. It's important to discuss these possibilities with your doctor beforehand.
Mental and Emotional Wellbeing
A prostate diagnosis can be stressful. Seeking support from family, friends, support groups, or a mental health professional can be incredibly beneficial. You are not alone on this journey.
Conclusion
Taking charge of your prostate health is a powerful and proactive step toward ensuring long-term well-being. While diseases of the prostate are a common part of aging for many men, they are not inevitable, and they are certainly manageable. Understanding the differences between BPH, prostatitis, and prostate cancer empowers you to recognize potential warning signs early. Modern medicine offers a robust spectrum of management strategies, from watchful waiting and lifestyle adjustments to advanced surgical and radiation techniques. The most important action you can take is to engage in an open, ongoing dialogue with a healthcare professional. They can guide you through appropriate screening, help interpret results, and tailor a treatment plan that aligns with your personal health goals and lifestyle. Don't let uncertainty or fear prevent you from taking action, your health is worth it.
Consult a Top Specialist
Consult a Top Specialist

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Swaroopa Rani
General Physician/ Internal Medicine Specialist
9 Years • MBBS, MD (Internal Medicine)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Shiv Krishna Mitra
General Practitioner
15 Years • MBBS GEN. MED. PGDRM, MCH
Kolkata
Samaritan Clinic, Kolkata

Dr Aakash Andgi
General Physician/ Internal Medicine Specialist
9 Years • MBBS MD
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Nilotpal Mitra
General Physician/ Internal Medicine Specialist
20 Years • MBBS, PGDGM ( Geriatric Medicine), ACMDC (an Advance course in Diabetes and cardiovascular diseases from PHFI and WHF )
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
More articles from General Medical Consultation
Frequently Asked Questions
1. What is the main cause of an enlarged prostate (BPH)?
The exact cause isn't fully understood, but it is primarily linked to hormonal changes that occur as men age. Specifically, it's believed to be related to changes in the balance of hormones like testosterone and dihydrotestosterone (DHT).
2. Can prostatitis be sexually transmitted?
While most types of prostatitis are not STIs, acute bacterial prostatitis can sometimes be caused by bacteria associated with sexually transmitted infections like chlamydia or gonorrhea. It's important to get an accurate diagnosis to receive the correct prostate infection treatment.
3. Does having BPH increase my risk of prostate cancer?
No, research indicates that having BPH does not directly increase your risk of developing prostate cancer. However, because the symptoms can be similar, it's crucial to see a doctor to get a proper diagnosis and rule out cancer.
4. What are the warning signs of prostate cancer I shouldn't ignore?
Early-stage prostate cancer often has no symptoms. As it advances, symptoms can include urinary problems (similar to BPH), blood in the semen or urine, erectile dysfunction, and pain in the back, hips, or pelvis. Any persistent changes in urinary or sexual function warrant a doctor's visit.
5. Are there natural ways to lower my PSA level?
Some studies suggest that certain lifestyle changes may help maintain healthy PSA levels, including eating a diet rich in tomatoes (lycopene), fatty fish, and vegetables; exercising regularly; and managing stress. However, a high PSA level requires medical evaluation to determine the cause, as it could indicate a serious condition.




