Upper Respiratory Infection: Causes, Symptoms, and Relief
Know about the upper respiratory infection, what exactly it is, uri versus respiratory infections, causes, how it spreads, recognising signs and symptoms, who is at rosk, diagnosis, treatment options and prevention.

Written by Dr. D Bhanu Prakash
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 13th Jan, 2026
Introduction
That all-too-familiar tickle in the back of your throat, the sudden onset of sneezing, and the general feeling of being unwell chances are, you're experiencing an upper respiratory infection (URI). This article delves deep into the world of upper respiratory infections, exploring the viruses that cause them, how they spread, and the tell-tale signs your body is fighting one off. We'll also guide you through effective relief strategies, crucial prevention tips, and most importantly, when it's time to consult a doctor.
What Exactly is an Upper Respiratory Tract Infection?
An upper respiratory infection is an acute illness affecting the mucosal surfaces of your upper airway. This includes everything from your nose and sinuses down to your throat (pharynx) and voice box (larynx). Think of it as your body's frontline becoming inflamed and irritated by an invading pathogen, primarily a virus. While we often use terms like "common cold" interchangeably, a cold is actually a type of URI, but URIs also encompass sinusitis, pharyngitis, laryngitis, and the flu.
Consult Top Specialists for Personalised Tips
The Anatomy of Your Upper Respiratory System
Your upper respiratory tract is a sophisticated air-processing system. Air enters through your nostrils, where nasal hairs and mucus trap large particles. It then moves to the sinuses, which help humidify the air and give your voice resonance. The air passes through the pharynx (throat), a muscular tube that also serves as a pathway for food, and then the larynx (voice box), which contains your vocal cords, before heading down your trachea to your lungs. When a virus invades any part of this system, it causes inflammation, leading to the classic symptoms of a URI, like congestion, sore throat, and a hoarse voice.
URI vs. Lower Respiratory Infection: Knowing the Difference
The key difference lies in the location. Upper respiratory infections are generally less severe and affect the areas mentioned above. Lower respiratory infections (LRIs), such as bronchitis and pneumonia, impact the airways and structures of the lungs themselves (bronchi, bronchioles, alveoli). LRIs often present with deeper, more persistent coughs, shortness of breath, and wheezing, and can be more serious, especially for vulnerable populations.
The Usual Suspects: Primary Causes of URIs
The primary causes include:
Viral Villains: The Rhinovirus and Its Companions
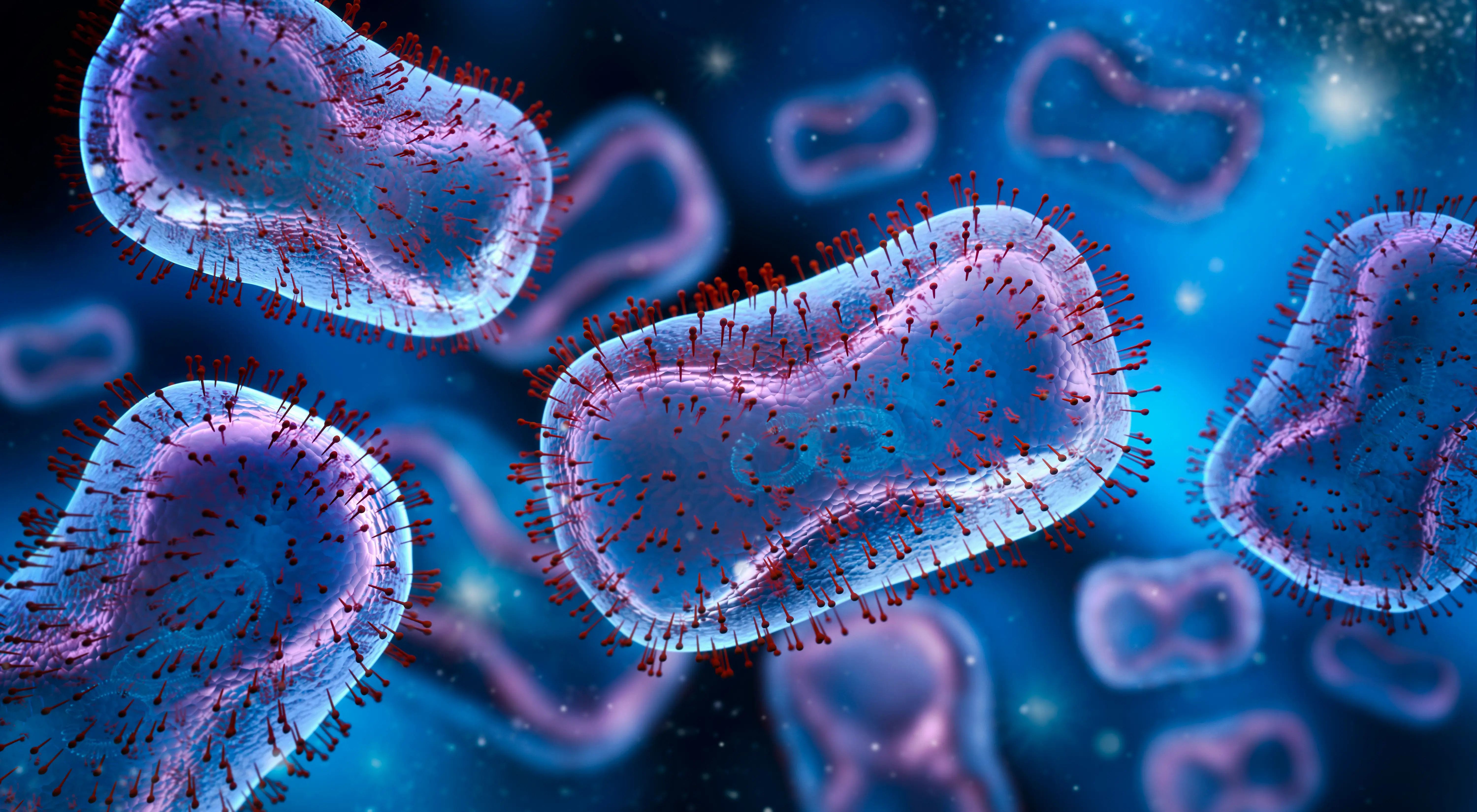
Over 200 different viruses can cause a URI, but the champion is the rhinovirus, responsible for 10-40% of all common colds. Other frequent offenders include:
Coronaviruses: Not just SARS-CoV-2 (which causes COVID-19), but several other common strains cause typical cold symptoms.
Influenza Viruses: Cause the flu, which is a more severe type of URI with a sudden onset of high fever and body aches.
Respiratory Syncytial Virus (RSV): Common in children but can also affect adults, often mimicking a bad cold.
Adenoviruses: Can cause a range of illnesses, from colds to sore throat, bronchitis, and pneumonia.
Parainfluenza Viruses: A common cause of croup in young children and colds in adults.
These viruses invade the cells lining your respiratory tract, hijacking their machinery to replicate, which damages the cells and triggers your body's inflammatory immune response.
Less Common Culprits: Bacterial and Other Causes
While viruses are the dominant cause, bacteria can sometimes be the primary pathogen or cause a secondary bacterial sinus infection following a viral cold. The most common bacterial cause is Streptococcus pyogenes, which leads to strep throat. Allergies and environmental irritants (like smoke or pollution) can also cause inflammation that mimics URI symptoms but is not infectious.
How Upper Respiratory Infections Spread Like Wildfire
Understanding transmission is key to prevention. URI viruses are highly contagious and spread through several routes.
Direct Contact Transmission
This is one of the most common ways. If an infected person covers their mouth to cough or sneeze and then touches a doorknob, you touch that same doorknob and then rub your eye or nose, you've directly transferred the virus to your own mucous membranes.
Airborne Droplet Transmission
When an infected person talks, coughs, or sneezes, they expel tiny droplets containing the virus into the air. If you are nearby (typically within 6 feet), you can inhale these droplets directly into your respiratory tract.
Contaminated Surface Transmission
Viruses can survive on hard surfaces like plastic and stainless steel for several hours. Touching a contaminated remote control, keyboard, or handrail and then touching your face is a major vector for spread.
Recognising the Signs: Common URI Symptoms
The signs of an upper respiratory tract infection can vary depending on the specific virus and the individual, but they follow a general pattern.
Early Warning Signs
The initial phase often includes a scratchy or sore throat, mild fatigue, a slight chill, and a runny nose with clear mucus.
Full-Blown Symptom Profile
As the infection progresses, symptoms typically peak and may include:
Nasal congestion and sinus pressure
Increased mucus production (runny nose), which may turn thicker and yellow/green as your immune system fights the infection—this is normal and not always a sign of a bacterial sinus infection.
Sneezing and coughing
Hoarseness or laryngitis
Mild to moderate headache
Watery eyes
Low-grade fever (more common in children)
From Annoying to Severe: A Spectrum of Discomfort
For most healthy adults, a URI is a miserable but self-limiting experience. However, the inflammation and mucus can lead to secondary issues like ear infections (from blocked Eustachian tubes) or sinus infections if drainage is completely blocked.
Who is Most at Risk of Catching a URI?
While anyone can get a cold, some factors significantly increase risk and severity.
Lifestyle and Environmental Risk Factors
Close Quarters: Working in offices, attending school, flying on aeroplanes, or living in dormitories increases exposure.
Season: Cold and flu season (fall and winter) sees a spike as people spend more time indoors with recirculated air.
Smoking: Damages the cilia (tiny hairs) in your respiratory tract that sweep away pathogens, making smokers more susceptible to infections and longer recovery times.
Lack of Sleep: Compromises immune function.
Underlying Health Conditions That Increase Vulnerability
It includes:
Weakened Immune System: From conditions like HIV/AIDS, cancer treatments, or immunosuppressant drugs.
Chronic Heart or Lung Disease: Such as asthma or COPD.
Age: Young children with immature immune systems and older adults with declining immune function are at higher risk.
How Are Upper Respiratory Infections Diagnosed?
The diagnosis of upper respiratory tract infections:
When a Doctor's Visit is Necessary
Most URIs don't require a formal diagnosis. However, you should seek medical advice if symptoms are severe, persist for more than 10 days, or if you experience high fever, difficulty breathing, or severe headache. If your condition does not improve after trying home methods, book a physical visit to a doctor with Apollo24|7 for a proper evaluation.
What to Expect During the Examination
A doctor will typically perform a physical exam, checking your ears, nose, throat, and listening to your lungs. They will review your symptoms and medical history. In most cases, this is sufficient. If strep throat is suspected, a rapid strep test may be performed. For other concerns, they might recommend specific tests; Apollo24|7 offers convenient home collection for tests like a CBC (Complete Blood Count) to check for signs of bacterial infection if needed.
Easing the Discomfort: Treatment and Home Remedies
Since viruses cause most URIs, antibiotics are ineffective. Treatment focuses on managing symptoms of a URI and supporting your body's natural healing process.
Supportive Care and Home Management
Hydration: Drink plenty of fluids like water, broth, and herbal tea. This thins mucus, soothes a sore throat, and prevents dehydration.
Rest: Your body needs energy to fight the virus. Prioritise sleep and reduce physical activity.
Humidity: Use a cool-mist humidifier or take a steamy shower to moisten nasal passages and ease congestion and cough.
Saltwater Gargle: Can soothe a sore throat.
Saline Nasal Sprays: Help moisturise nasal passages and flush out irritants.
Over-the-Counter (OTC) Medication Options
Pain Relievers/Fever Reducers: Acetaminophen or ibuprofen for aches and fever.
Decongestants (e.g., pseudoephedrine) can shrink swollen nasal passages. Use with caution and not for more than a few days.
Cough Suppressants: (e.g., dextromethorphan) for dry, hacking coughs.
Expectorants: (e.g., guaifenesin) help loosen thick mucus, making it easier to cough up.
Always read labels carefully and consult a pharmacist if you have other health conditions or are taking other medications.
Preventing the Spread: Your Best Defense Against URIs
Personal Hygiene: The First Line of Defense
Handwashing: Frequently wash hands with soap and water for at least 20 seconds, especially after being in public.
Hand Sanitiser: Use alcohol-based sanitiser when soap isn't available.
Avoid Touching Your Face: Keep your hands away from your eyes, nose, and mouth.
Disinfect Surfaces: Regularly clean high-touch areas like phones and countertops.
Respiratory Etiquette: Cough and sneeze into your elbow or a tissue, not your hands.
Boosting Your Immune System Naturally
A robust immune system is your best armour. Maintain it with:
A balanced diet rich in fruits and vegetables.
Regular, moderate exercise.
Consistent, quality sleep (7-9 hours for adults).
Managing stress levels.
When to Seek Professional Medical Advice
While most URIs resolve on their own, it's crucial to recognise red flags. Consult a doctor online with Apollo24|7 for further evaluation if you or your child experiences:
Difficulty breathing or shortness of breath.
Symptoms that worsen or fail to improve after 10 days.
A high fever (over 103°F or 39.4°C for adults; any fever in infants under 12 weeks).
Severe symptoms like a stiff neck, severe headache, or confusion.
Dehydration (e.g., dizziness, little urination).
Conclusion
An upper respiratory infection*, while incredibly common and often disruptive, is usually a self-contained battle that your body is well-equipped to win. Understanding that viruses are the primary cause empowers you to focus on effective symptomatic relief and patience, rather than seeking unnecessary antibiotics. The journey from the first sneeze to full recovery hinges on supportive care: ample rest, fluids, and smart use of OTC remedies. By listening to your body and knowing when to seek professional guidance, you can navigate cold and flu season with greater confidence and ease. Remember, a proactive
Consult Top Specialists
Consult Top Specialists for Personalised Tips

Dr. Kiran K J
General and Laparoscopic Surgeon
18 Years • MBBS, MS, FMAS, DMAS (Fellow & Dip in Min. Access surg.), FALS- Bariatric & Robotic Surgery
Bengaluru
Apollo Hospitals Bannerghatta Road, Bengaluru
(50+ Patients)

Dr. Praveen Sodhi
General Surgeon
20 Years • MBBS, MS Lap., Gastro, Anorectal & Breast Surg.
Delhi
Apollo Hospitals Indraprastha, Delhi
(175+ Patients)

Dr. Nikhilesh Krishna
Bariatrician
7 Years • MS, FMAS, FALBS
Chennai
Apollo Hospitals Greams Road, Chennai
Dr. Saket Goel
General Surgeon
27 Years • MBBS, MS (Surg.)
Delhi
Apollo Hospitals Indraprastha, Delhi
(125+ Patients)

Dr. Sunil Kaul
General Surgeon
30 Years • MBBS, MS, FICS, FIMSA, FMAS
Delhi
Apollo Hospitals Indraprastha, Delhi
(25+ Patients)
Consult Top Specialists

Dr. Kiran K J
General and Laparoscopic Surgeon
18 Years • MBBS, MS, FMAS, DMAS (Fellow & Dip in Min. Access surg.), FALS- Bariatric & Robotic Surgery
Bengaluru
Apollo Hospitals Bannerghatta Road, Bengaluru
(50+ Patients)

Dr. Praveen Sodhi
General Surgeon
20 Years • MBBS, MS Lap., Gastro, Anorectal & Breast Surg.
Delhi
Apollo Hospitals Indraprastha, Delhi
(175+ Patients)

Dr. Nikhilesh Krishna
Bariatrician
7 Years • MS, FMAS, FALBS
Chennai
Apollo Hospitals Greams Road, Chennai
Dr. Saket Goel
General Surgeon
27 Years • MBBS, MS (Surg.)
Delhi
Apollo Hospitals Indraprastha, Delhi
(125+ Patients)

Dr. Sunil Kaul
General Surgeon
30 Years • MBBS, MS, FICS, FIMSA, FMAS
Delhi
Apollo Hospitals Indraprastha, Delhi
(25+ Patients)