What Leads To Signs Of Vaginal Yeast Infection And
Discover what causes vaginal yeast infections, from antibiotics and hormonal changes to diet and lifestyle habits. Learn the signs, symptoms, and when to seek medical help.

That familiar, maddening itch. The uncomfortable burning sensation. If you've experienced a vaginal yeast infection, you know how disruptive it can be. You're not alone; it's estimated that 75% of women will have at least one yeast infection in their lifetime. But what exactly triggers these frustrating symptoms? This article demystifies the signs of a vaginal yeast infection and delves deep into the underlying causes. We'll move beyond the basic list and explore the why—the biological mechanisms that throw your delicate vaginal ecosystem out of balance. From common culprits like antibiotics to the surprising role of your diet and lifestyle, we'll provide a comprehensive guide to help you understand, identify, and prevent this common condition, empowering you to take control of your intimate health.
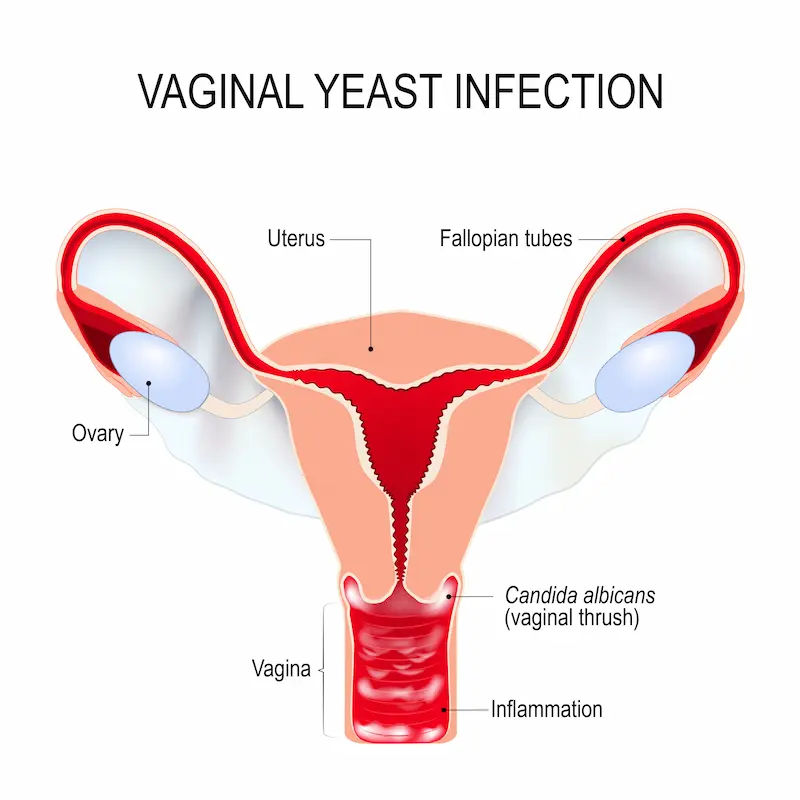
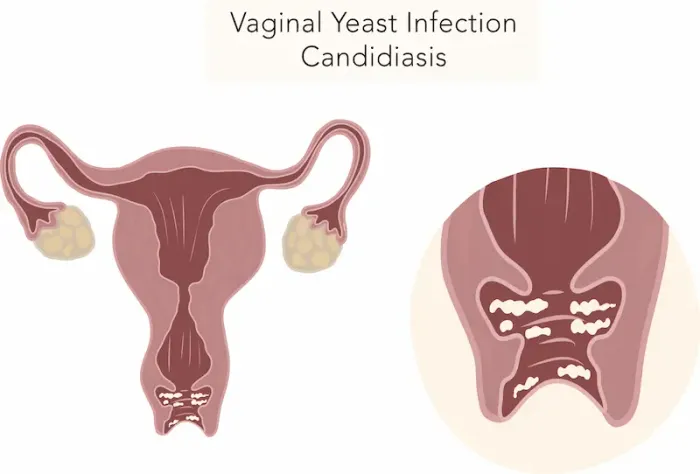
What Exactly Is a Vaginal Yeast Infection?
A vaginal yeast infection, medically known as vulvovaginal candidiasis, is not an invasion by a foreign germ but rather an internal takeover. It's a common fungal infection caused by an overgrowth of yeast cells, primarily the species Candida albicans, that naturally live in your vagina.
The Usual Suspect: Candida Albicans
Think of Candida as a neutral resident that's always present in small, harmless amounts in your vagina, mouth, and gut. It's kept in check by your body's natural defences and, crucially, by other microorganisms.
The Good Guys: Your Vaginal Microbiome
Your vagina is home to a community of bacteria, predominantly beneficial Lactobacilli. These good bacteria act like a protective militia. They maintain a slightly acidic vaginal environment (low pH) by producing lactic acid and hydrogen peroxide, which actively suppresses the uncontrolled growth of yeast. A vaginal yeast infection occurs when something disrupts this delicate balance, allowing Candida to multiply unchecked and cause the irritating symptoms we associate with an infection.
The Most Common Signs and Symptoms
Recognising the signs of a vaginal yeast infection is the first step toward relief. While symptoms can vary in severity, there are several common indicators.
The Hallmark Symptom: Intense Itching
The most prevalent and often most bothersome symptom is intense itching in and around the vagina and vulva (the external genitalia). This itching is a direct inflammatory response to the overgrowth of yeast and the toxins they release.
Understanding Vaginal Discharge Changes
Many women notice a change in their discharge. While normal discharge is clear or whitish and can vary in consistency throughout your cycle, a yeast infection typically causes a thick, white, odourless discharge often described as resembling cottage cheese. However, it's important to note that some women may experience only itching with little to no discharge, or even a watery discharge.
Pain, Redness, and Swelling
The inflammation caused by the infection can lead to:
• Redness and swelling of the vulva.
• A burning sensation, especially during urination (as urine touches the irritated skin) or intercourse.
• General soreness and a rash.Consult a Gynaecologist for Personalised Advice
The Root Causes: What Throws Things Off Balance?
Understanding the causes means understanding what disrupts the microbial peace treaty in your vagina. Here are the primary culprits.
Antibiotics: The Unintended Consequence
This is one of the most common triggers. Broad-spectrum antibiotics, while fighting a bad infection elsewhere in your body, are non-discriminatory. They wipe out the harmful bacteria causing your illness and the beneficial Lactobacilli in your vagina. With the protective bacteria diminished, yeast can flourish, leading to a yeast infection from antibiotics.
Hormonal Fluctuations and Imbalances
Hormones, particularly estrogen, have a significant impact on the vaginal environment. High estrogen levels can promote yeast growth by increasing glycogen (a type of sugar) in vaginal tissues, which yeast feeds on.
Pregnancy and Yeast Infections
Pregnancy causes elevated estrogen levels and changes in the immune system, making women more susceptible to yeast infections during pregnancy.
Birth Control and Menstrual Cycles
High-estrogen birth control pills and hormone therapy can similarly increase risk. Some women also notice a pattern of symptoms flaring up right before their period, another time of hormonal shift.
A Weakened Immune System
• Your immune system is a key player in keeping Candida in its place. Conditions or behaviours that suppress your immune response can open the door for an overgrowth. This includes:
• Unmanaged stress and lack of sleep.
• Chronic illnesses like HIV/AIDS or uncontrolled diabetes.
• Medical treatments like chemotherapy or corticosteroids.
Lifestyle and Dietary Triggers
Your daily habits play a more significant role than you might think.
The Impact of High-Sugar Diets
Yeast thrives on sugar. A diet consistently high in refined sugars and carbohydrates can provide ample fuel for Candida overgrowth, not just in the vagina but throughout the body. This is a key reason why women with diabetes are at higher risk if their blood sugar is not well-controlled.
Clothing and Moisture Traps
Tight-fitting clothing, especially non-breathable synthetic fabrics like nylon or spandex, traps heat and moisture. This creates a warm, dark, and moist environment—the perfect breeding ground for yeast. This includes tight jeans, pantyhose, and wet workout clothes or swimsuits worn for extended periods.
Less Common but Possible Causes
While the above causes are most frequent, other factors can contribute. Douching is a major one; it disrupts the natural pH and flora balance, doing more harm than good. Certain sexual activities can sometimes introduce new strains of yeast or disrupt the environment, though yeast infections are not considered a classic STD. Finally, some women may simply have a genetic predisposition that makes them more susceptible to recurrent yeast infections.
When It's Time to See a Doctor
It's crucial to see a healthcare provider if:
• This is your first time experiencing these symptoms.
• You're unsure if it's a yeast infection or something else (like BV or an STI).
• Your symptoms don't improve after using over-the-counter antifungal treatments.
• You experience recurrent infections (four or more in a year).
• You have a fever, chills, nausea, or lower abdominal pain.
• You have a weakened immune system due to an existing medical condition or medication.
Conclusion: Regaining Control and Confidence
Dealing with the signs of a vaginal yeast infection can be frustrating, but understanding the root causes empowers you to take proactive steps. It’s a story of balance—a delicate ecosystem where bacteria and yeast coexist peacefully until something shifts. By recognising triggers like antibiotics, hormonal changes, and lifestyle factors, you can make informed choices to support your vaginal health. Prioritise breathable clothing, manage sugar intake, consider probiotics, and always complete antibiotic courses as directed. Most importantly, listen to your body and don't hesitate to seek professional medical advice for proper diagnosis and treatment. Taking control of these factors is your best strategy for maintaining comfort and confidence.
Consult a Gynaecologist for Personalised Advice
Consult a Gynaecologist for Personalised Advice

Dr. Sanjan Das
Obstetrician and Gynaecologist
15 Years • MBBS,MS
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru

Dr. Srinka Mukherjee
Obstetrician and Gynaecologist
7 Years • MBBS, MS Obstetrics & Gynaecology
Kolkata
Doctor's World, Kolkata

Dr. Pritam Dey
Obstetrician and Gynaecologist
6 Years • MBBS,MS(OBSTETRICS & GYNAECOLOGY),FMAS
Kolkata
Dr. Pritam Dey's Chamber, Kolkata
(50+ Patients)

Dr. Parul Sharma
Obstetrician and Gynaecologist
8 Years • MBBS, MS (Obstetrics & Gynaecology)
New Delhi
THE DOCTORS NESST, New Delhi

Dr. Mehnaz Rashid
Obstetrician and Gynaecologist
7 Years • MBBS, DNB (Obstetrics & Gynaecology), D.MAS, F.MAS, WALS
Bengaluru
Wellstar Polyclinic and Diagnostic Center, Bengaluru
(275+ Patients)
Consult a Gynaecologist for Personalised Advice

Dr. Sanjan Das
Obstetrician and Gynaecologist
15 Years • MBBS,MS
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru

Dr. Srinka Mukherjee
Obstetrician and Gynaecologist
7 Years • MBBS, MS Obstetrics & Gynaecology
Kolkata
Doctor's World, Kolkata

Dr. Pritam Dey
Obstetrician and Gynaecologist
6 Years • MBBS,MS(OBSTETRICS & GYNAECOLOGY),FMAS
Kolkata
Dr. Pritam Dey's Chamber, Kolkata
(50+ Patients)

Dr. Parul Sharma
Obstetrician and Gynaecologist
8 Years • MBBS, MS (Obstetrics & Gynaecology)
New Delhi
THE DOCTORS NESST, New Delhi

Dr. Mehnaz Rashid
Obstetrician and Gynaecologist
7 Years • MBBS, DNB (Obstetrics & Gynaecology), D.MAS, F.MAS, WALS
Bengaluru
Wellstar Polyclinic and Diagnostic Center, Bengaluru
(275+ Patients)