Hormones and Fertility: A Complete 2025 Guide
Know about the hormones and fertility guide, what it is, menstrual cycle phases, male hormones, common causes of infertility in men and women and more.


Introduction
Hormones are your body’s chemical messengers, and when it comes to fertility, they call the plays. From triggering ovulation to preparing the uterus for implantation, hormones like FSH, LH, estrogen, and progesterone coordinate a monthly cycle that makes pregnancy possible. On the male side, testosterone, FSH, and LH drive sperm production and quality. When even one signal is off, conception can take longer or require treatment. In this complete guide for the general public, we’ll unpack how hormones shape fertility for women and men, what common imbalances look like, how and when to test, and which treatments and daily habits can restore hormone balance. You’ll see where age, stress, sleep, weight, and environmental exposures fit in, and get clear, actionable steps to move forward.
Why Hormones Matter for Fertility
Hormones are the link between your brain and reproductive organs. In women, the hypothalamus (in your brain) releases GnRH in pulses, stimulating the pituitary gland to release FSH and LH. FSH nudges ovarian follicles to grow and produce estradiol; LH triggers ovulation. After ovulation, the corpus luteum makes progesterone to prime the uterine lining. In men, the same brain–pituitary signals (FSH and LH) prompt the testes to make testosterone and nurture sperm cells through a roughly 72–90 day maturation process.
Consult a Top Endocrinologist for Personalised Advice
Think of the system as a music ensemble—the hypothalamus is the conductor, the pituitary the first violin, and the ovaries/testes the orchestra. If one instrument is out of tune, the performance suffers. An imbalance in thyroid hormone, prolactin, or insulin, for instance, can dampen ovulation or lower sperm quality. Likewise, exogenous testosterone can shut down sperm production by telling the pituitary “we’ve got enough,” reducing LH and FSH.
Infertility is a couple’s condition. Roughly one in six adults globally experience infertility at some point, and male factors contribute in about 40–50% of cases—either alone or alongside female factors. That’s why both partners benefit from evaluation. A well-timed set of hormone and semen tests can pinpoint modifiable issues, guide targeted treatment, and avoid unnecessary delays.
The Menstrual Cycle, Explained by Hormones
The phases include:
Follicular phase: FSH, estradiol, and follicle selection
Day 1 is the first day of your period. Under the pituitary’s FSH, a cohort of follicles begins to grow; one becomes “dominant.” Rising estradiol thickens the uterine lining and feeds back to fine-tune FSH. In many cycles, the follicular phase lasts 10–17 days, but this is the most variable phase, especially under stress, illness, or travel—factors that change GnRH pulse frequency and can delay ovulation.
Ovulation: LH surge timing and signs
As estradiol peaks, it flips feedback from negative to positive—provoking a sharp LH surge. Ovulation typically occurs about 24–36 hours after the LH surge. Cervical mucus becomes clear and stretchy; some people note mild mid-cycle pain. Urine LH predictor kits detect this surge at home, but if fluid intake is high or surges are brief, you can miss it. In PCOS, chronically elevated LH can make results confusing—monitoring trends and pairing with basal temperature or ultrasound can help.
Luteal phase: progesterone and implantation window
After ovulation, the corpus luteum releases progesterone, stabilising and differentiating the uterine lining and slightly raising basal body temperature. The luteal phase is more consistent, often 12–14 days. If pregnancy occurs, hCG rescues the corpus luteum; if not, progesterone falls and a period follows. Mid-luteal progesterone (about 7 days after ovulation) helps confirm ovulation—more reliable than a fixed “day 21” unless you have a classic 28-day cycle.
Typical testing windows and what your results mean (with caveats)
- Day 2–4: FSH, LH, and estradiol provide a baseline snapshot of ovarian response. Elevated day-3
- FSH can suggest reduced ovarian reserve, but interpretation depends on estradiol level and lab standards.
- Any cycle day: AMH for ovarian reserve; stable across the cycle but varies by lab method.
- About 7 days post-ovulation: Serum progesterone to confirm ovulation. Values vary; a single low value may reflect timing rather than failure to ovulate.
- Unique insight: Many apps assume a 28-day cycle. If your cycle length varies, anchoring hormone tests to ovulation (e.g., progesterone 7 days after a positive LH test) is far more accurate than testing on fixed calendar days.
Male Hormones and Fertility
The role of male hormones and their relation to fertility
FSH/LH, testosterone, and inhibin B in sperm production
In men, LH stimulates Leydig cells to make testosterone; FSH acts on Sertoli cells to support sperm development. Local (intratesticular) testosterone needs to be high to sustain spermatogenesis. Inhibin B, made by Sertoli cells, feeds back to the pituitary about sperm production efficiency. Low sperm count with low/normal LH/FSH suggests a testicular production problem; low LH/FSH points to a brain–pituitary (secondary) cause.
What affects sperm quality: heat, stress, toxins, meds
Sperm mature over months, so exposures matter. Heat (saunas, hot tubs), tight scrotal temperature increases (laptops on lap, prolonged cycling without breaks), smoking, heavy alcohol, cannabis, certain environmental chemicals (phthalates), and chronic stress can lower count and motility. Some medications—exogenous testosterone, anabolic steroids, opioids, and some antipsychotics—suppress the brain–pituitary signals needed for sperm production.
When male hormone testing is useful (and when semen analysis comes first)
The first test is a semen analysis. If abnormal on at least two samples, male hormone labs (total testosterone, LH, FSH, ± prolactin, ± estradiol, ± TSH) can clarify the cause. If symptoms include low libido, erectile dysfunction, breast changes, or known pituitary disease, testing sooner is reasonable. Stopping exogenous testosterone is crucial; recovery of sperm can take 3–12 months.
Common Hormonal Causes of Infertility (Women)
The correlation of hormones with infertility in women is
PCOS and anovulation
Polycystic ovary syndrome (PCOS) is a leading cause of anovulation and irregular cycles, affecting about 6–12% of people with ovaries. Hallmarks include irregular or absent ovulation, signs of androgen excess (acne, excess hair), and polycystic ovarian morphology on ultrasound. Insulin resistance is common and can heighten ovarian androgen production, disrupting follicle maturation. Many individuals with PCOS ovulate irregularly—conceiving is possible but less predictable without treatment.
Thyroid disorders (hypo/hyperthyroidism)
Thyroid hormones influence GnRH pulses, SHBG levels, and ovulation. Hypothyroidism can cause irregular cycles, anovulation, and increased miscarriage risk; hyperthyroidism can also disrupt cycles and luteal function. Treating thyroid disease and aiming for TSH in the normal range—often <2.5 mIU/L in those trying to conceive—improves outcomes.
Hyperprolactinemia
Prolactin inhibits GnRH, reducing FSH/LH and ovulation. Causes include pituitary microadenomas, medications (e.g., risperidone), hypothyroidism, and stress. Symptoms may include irregular or absent periods and galactorrhea. Dopamine agonists (cabergoline, bromocriptine) typically restore ovulation and improve fertility.
Primary ovarian insufficiency (POI)
POI is impaired ovarian function before age 40, presenting with irregular or absent periods and menopausal-range FSH. It can be sporadic or linked to autoimmune or genetic factors. Spontaneous ovulation and pregnancy can occur but are unpredictable; donor eggs are a common path to parenthood.
Luteal phase defects: what the evidence says
“Luteal phase defect” has been proposed as a cause of infertility or miscarriage based on low progesterone or biopsy criteria. However, diagnostic tests are inconsistent, and major societies do not recommend routine biopsy-based diagnosis. If ovulation is confirmed and cycles are otherwise normal, empiric luteal support is generally reserved for assisted reproduction or recurrent pregnancy loss settings under specialist care.
Lifestyle, Stress, Sleep, and Weight: Hormones in Daily Life
Let's see how hormones influence the lifestyle, stress, sleep and weight.
Cortisol, circadian rhythm, and menstrual regularity
Chronic stress elevates cortisol, which can suppress GnRH pulses and delay ovulation. Shift work and circadian disruption are linked to cycle irregularities and lower fecundability in some studies. Practical tweaks consistent sleep and wake times, daylight exposure in the morning, and dim light in the evening help stabilise circadian cues that influence reproductive hormones.
Insulin resistance, leptin, and ovulation
Insulin resistance increases ovarian androgen production, contributing to follicle arrest in PCOS. Weight loss of 5–10% in those with higher BMI can restore ovulation in many cases, largely via improved insulin sensitivity. At lower BMI, leptin deficiency from relative energy deficiency can suppress GnRH—restoring adequate energy intake often normalises cycles. This energy balance lens explains why both high and very low BMI can impair fertility.
Environmental and Medication Factors
The environmental and medication factors include:
Endocrine disruptors (BPA, phthalates) and reproductive hormones
Plasticisers (BPA, phthalates) and certain pesticides can interact with hormone receptors. Observational studies associate higher exposure with reduced oocyte yield, altered ovarian reserve markers, and decreased semen quality, though causality and effect sizes vary. Reducing exposure to stainless steel/Glass for food storage, avoiding microwaving plastic, and minimising fragranced products may be prudent while trying to conceive.
Medications that alter hormones
- Exogenous testosterone and anabolic steroids suppress LH/FSH and sperm production; avoid if trying to conceive.
- Some antipsychotics, metoclopramide, and opioids can raise prolactin and suppress ovulation or reduce testosterone.
- Glucocorticoids (long-term/high-dose) can impair HPG axis function.
- Discuss any medication changes with your clinician; abrupt discontinuation can be harmful.
Alcohol, tobacco, cannabis: what we know and don’t
Heavy alcohol and smoking clearly impair fertility parameters; minimising or avoiding is advisable preconception. Cannabis data are mixed, but some studies indicate altered sperm parameters and ovulatory changes; cautious reduction is sensible when trying to conceive [2][6].
How to Test Your Hormones for Fertility
These tests for hormones include:
Core labs
- Day 2–4: FSH, LH, estradiol to assess baseline function.
- AMH: any day; reflects ovarian reserve quantity, not egg quality.
- Mid-luteal progesterone: about 7 days after ovulation confirmation (not rigid “day 21”).
- TSH and free T4: screen for thyroid disease; treat abnormal results before/during attempts to conceive.
- Prolactin: morning, fasting, minimal stress; repeat if mildly elevated.
- Androgens (total/free testosterone, DHEAS): if PCOS or clinical signs of androgen excess.
- Glucose/insulin or HbA1c: screen for insulin resistance/metabolic health.
Apollo 24|7 offers convenient home collection for tests like TSH, prolactin, AMH, vitamin D, and HbA1chelpful if scheduling is tight or you prefer at-home sampling.
Semen analysis and when to add male hormone labs
Start with two semen analyses a few weeks apart. If abnormal, add male hormones: total testosterone (morning), LH, FSH, ± prolactin, ± estradiol, ± TSH. If testosterone is low, repeat to confirm and evaluate SHBG, especially if obesity or thyroid issues are present.
At-home tools: LH kits, basal temperature, apps
- LH ovulation predictor kits identify the fertile window; test around midday, reduce fluids beforehand for better detection.
- Basal body temperature rises after ovulation; helpful for confirming but not predicting.
- Wearables/apps can supplement but should not replace clinical testing when cycles are irregular or conception is delayed.
If symptoms persist beyond two cycles of careful tracking without clear ovulation, consult a doctor online with Apollo24|7 for tailored evaluation and next steps.
Treatment Options: Fixing Hormonal Roadblocks
PCOS ovulation induction, metformin, lifestyle
Letrozole is first-line for ovulation induction in PCOS and improves live-birth rates compared to clomiphene in many studies [1][7]. Metformin benefits metabolic health and may enhance ovulation in insulin-resistant individuals. Lifestyle interventions (weight optimisation, exercise) amplify medication effects.
Thyroid replacement and optimising TSH
Treat overt hypothyroidism with levothyroxine; optimise TSH before attempting conception. Subclinical hypothyroidism decisions depend on TSH level, thyroid antibodies, and clinical context; shared decision-making is key. Hyperthyroidism requires directed therapy (antithyroid meds, endocrinology input) before pregnancy [8][9].
Treating high prolactin (dopamine agonists)
Cabergoline or bromocriptine normalises prolactin, restores ovulation, and is compatible with conception. For macroadenomas or resistance to medication, endocrine and neurosurgical input may be needed.
Hypogonadotropic hypogonadism and male therapies
Avoid exogenous testosterone. hCG (to stimulate Leydig cells) ± FSH injections can induce spermatogenesis in many cases; clomiphene may be considered in select men with secondary hypogonadism. Varicocele repair can improve semen parameters in specific scenarios.
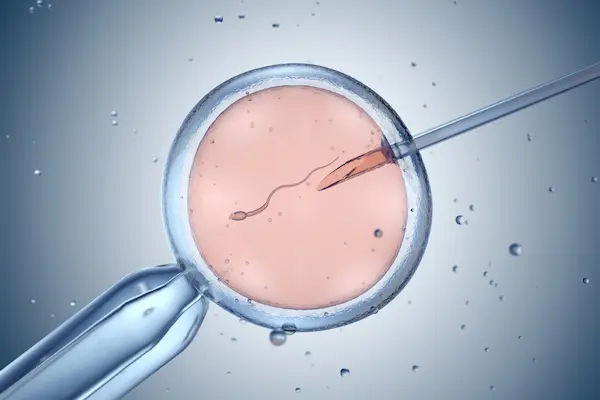
What IVF/ICSI hormonal protocols do and when they’re recommended
When first-line approaches fail or when age/ovarian reserve suggests lower natural fecundity, IVF uses controlled ovarian stimulation with FSH/LH analogues to recruit multiple follicles, followed by egg retrieval and fertilisation (IVF or ICSI). Progesterone supports the luteal phase after embryo transfer. Protocols are tailored to ovarian reserve and prior response.
If your condition does not improve after trying these methods, book a physical visit to a doctor with Apollo24|7 to discuss next steps, including assisted reproduction options.
Age, Ovarian Reserve, and Realistic Timelines
AMH and antral follicle count: what they do—and don’t—predict
AMH reflects the number of small follicles; lower AMH often means a lower response to stimulation, but doesn’t directly predict natural conception in a given month. Antral follicle count via ultrasound complements AMH. Neither test measures egg quality, strongly driven by age [1].
Female age vs. egg quality; male age and sperm DNA fragmentation
Egg quality decreases with age due to chromosomal errors during meiosis, dropping chances of monthly conception and increasing miscarriage risk after 35–37. Male age also matters: sperm DNA fragmentation and certain risks gradually rise with paternal age, though declines in male fertility are typically less steep.
Setting timelines: when to try, test, and escalate care
- Under 35: seek evaluation after 12 months of trying.
- Age 35–39: evaluate after 6 months.
- Age 40+: consider immediate evaluation.
Red flags needing earlier care: irregular/absent periods, known PCOS or thyroid disease, prior chemo/radiation, endometriosis, recurrent miscarriage, or male factor signs. If in doubt, consult a doctor online with Apollo 24|7 for personalised guidance.
Natural Ways to Support Hormonal Balance
The natural ways to support hormonal balance is
Nutrition patterns, vitamin D, omega-3s
A Mediterranean-style diet (vegetables, fruits, legumes, whole grains, olive oil, fish) is linked with better fertility outcomes in observational studies. Vitamin D sufficiency supports overall reproductive health; deficiency is common. Apollo24|7 offers convenient home collection for vitamin D testing. Omega-3 intake supports anti-inflammatory pathways; choose low-mercury fish or supplements verified for purity.
Exercise dose, sleep targets, stress skills
Moderate exercise improves insulin sensitivity and ovulatory function; excessive endurance training with low energy availability can disrupt cycles. Aim for 7–9 hours of sleep; prioritise regularity. Stress-reduction techniques (mindfulness, CBT, yoga) don’t “fix” hormones alone, but they improve adherence to behaviour changes that do.
Supplements: what has promising data (and what doesn’t)
- Inositol (myo-/D-chiro) may improve ovulation in PCOS via insulin signalling.
- CoQ10 shows mixed but promising data for ovarian response and sperm parameters; evidence is suggestive, not definitive.
- Be cautious with DHEA and herbal blends; evidence varies and interactions exist. Discuss with a clinician before starting.
When to See a Doctor
The criteria for seeing a doctor include:
Time-based criteria by age; red flags
- Under 35: 12 months of unprotected intercourse without pregnancy.
- 35–39: 6 months.
- 40 or above: immediate assessment.
- Red flags: irregular cycles, amenorrhea, galactorrhea, severe acne/hirsutism, known thyroid disease, pelvic surgery, endometriosis, chemotherapy, erectile dysfunction, or known varicocele.
What to bring and expect from a hormonal workup
Cycle history, prior labs, medications/supplements, lifestyle patterns, and both partners’ health history. Expect a plan including cycle-timed hormone tests, ultrasound, and semen analysis. If needed, additional endocrine tests will be added.
Getting labs and support conveniently
Use Apollo24|7 to book lab tests with home collection and to consult a doctor online for interpretation. If symptoms persist beyond two weeks or cycles are consistently irregular, consult a doctor online with Apollo24|7 for further evaluation.
Conclusion
Hormones are the hidden choreography behind fertility, coordinating everything from follicle development and ovulation to sperm production and uterine readiness. When the cues are clear and synchronised, conception is more likely; when they’re muffled or mistimed, cycles can become unpredictable and sperm parameters can slip. The encouraging news is that most hormonal barriers are identifiable and treatable. With informed testing—anchored to your cycle and symptoms—plus targeted treatment and practical lifestyle steps, many individuals and couples move from uncertainty to a clear plan. To make this easier, you can book hormone panels and consult a doctor online with Apollo 24|7, including home collection for key tests like TSH, prolactin, AMH, vitamin D, and HbA1c. With the right information and support, you can align your hormones with your goals and take confident next steps.
Consult a Top Endocrinologist for Personalised Advice
Consult a Top Endocrinologist for Personalised Advice

Dr. Sushith C
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Amrutha G
General Physician/ Internal Medicine Specialist
10 Years • MBBS,DNB(family medicine), Diabetologist-CCEBDM,CCGDM
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru

Dr. Nilotpal Mitra
General Physician/ Internal Medicine Specialist
20 Years • MBBS, PGDGM ( Geriatric Medicine), ACMDC (an Advance course in Diabetes and cardiovascular diseases from PHFI and WHF )
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
Dr Sumanth R
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Nupur Tandon
General Physician/ Internal Medicine Specialist
16 Years • MBBS, PG DIPLOMA IN Diabetes Management, Specialist in diabetes and thyroid disorders (CCEBDM)
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru
(25+ Patients)
Consult a Top Endocrinologist for Personalised Advice

Dr. Sushith C
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Amrutha G
General Physician/ Internal Medicine Specialist
10 Years • MBBS,DNB(family medicine), Diabetologist-CCEBDM,CCGDM
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru

Dr. Nilotpal Mitra
General Physician/ Internal Medicine Specialist
20 Years • MBBS, PGDGM ( Geriatric Medicine), ACMDC (an Advance course in Diabetes and cardiovascular diseases from PHFI and WHF )
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
Dr Sumanth R
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Nupur Tandon
General Physician/ Internal Medicine Specialist
16 Years • MBBS, PG DIPLOMA IN Diabetes Management, Specialist in diabetes and thyroid disorders (CCEBDM)
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru
(25+ Patients)
More articles from Infertility
Frequently Asked Questions
Which hormone is most important for fertility?
There isn’t a single “most important” hormone. For women, FSH, LH, estradiol, and progesterone work together to drive ovulation and implantation. For men, FSH, LH, and testosterone underpin sperm production. Thyroid and prolactin also influence both sexes. This interplay explains why a comprehensive fertility hormones test is useful.
Does a low AMH mean I can’t get pregnant?
No. AMH reflects ovarian reserve quantity, not egg quality or the ability to conceive this month. Many people with low AMH still conceive naturally, especially at younger ages. AMH is more predictive of response to IVF stimulation than of natural fertility.
Can stress really stop ovulation?
High or chronic stress can disrupt GnRH pulses and delay or suppress ovulation. While stress alone isn’t always the primary cause, improving sleep, circadian rhythm, and coping skills can help restore regular cycles in some individuals. Consider tracking ovulation with LH kits and, if irregularities persist, consult a doctor online with Apollo24|7.
How long after stopping testosterone will male fertility return?
Exogenous testosterone suppresses LH/FSH and spermatogenesis. Recovery can take 3–12 months, sometimes longer, depending on dose and duration. A semen analysis at intervals can track recovery; some men need medications like hCG/FSH under specialist care.
What are the best first tests if we’re not conceiving?
Often: day-3 FSH/LH/estradiol, AMH, TSH/free T4, prolactin, mid-luteal progesterone for the cycling partner, and a semen analysis for the male partner. From there, testing is tailored. Apollo24|7 offers convenient home collection for many of these labs.