Kidney Failure: Signs, Causes And Management
Learn about kidney failure—its signs, causes, and effective management. Discover how to detect early symptoms, slow disease progression, and make informed choices about dialysis or transplant.

_2.webp?tr=q-80,f-webp,w-350,dpr-2,c-at_max 700w)
Introduction
Kidney problems often creep up quietly—many people don’t notice symptoms until kidney function is already reduced. Understanding the signs of kidney failure, what leads to it, and which management steps actually work can help you protect your health and quality of life.
In this guide, you’ll learn how to spot early warnings, what tests confirm a diagnosis, the main causes behind kidney failure, and proven strategies to slow or prevent worsening. We’ll cover day-to-day kidney failure management—from medications and diet to avoiding hidden risks—plus what to expect if dialysis or transplant becomes necessary. You’ll also find practical tips for preventing acute kidney injury, a sudden decline that can happen during illness or after procedures.
Whether you’re newly diagnosed, supporting a loved one, or simply want to lower your risk, this article brings together trusted, up-to-date advice to help you make confident decisions and work closely with your healthcare team. If symptoms persist beyond two weeks or you’re worried about kidney health, consult a doctor online with Apollo 24|7 for further evaluation.
Understanding Kidney Failure vs CKD vs AKI
Here’s how doctors distinguish between different types of kidney problems and why it matters for treatment planning:
What “kidney failure” really means
The term “kidney failure” can refer to very low kidney function requiring dialysis or transplant (kidney replacement therapy), but many people use it more broadly to mean “severe kidney problems.” Clinicians prefer precise terms.
- Chronic kidney disease (CKD) is a long-term decline in kidney function or evidence of kidney damage (for example, albumin in urine) lasting more than three months. End-stage kidney disease (ESKD) usually means kidney function is low enough that dialysis or transplant is needed.
- Acute kidney injury (AKI) is a sudden drop in function—over hours to days—often triggered by illness, dehydration, medications, or surgery.
Chronic kidney disease (CKD) vs acute kidney injury (AKI)
- CKD progresses over years. Many people are asymptomatic until later stages, which is why screening of high-risk groups is so important.
- AKI can happen to anyone, even with previously normal function, and can be reversible if addressed promptly. Unfortunately, AKI raises the risk of developing CKD later. Recognising and preventing AKI is a powerful part of kidney failure management.
CKD stages and what eGFR numbers mean
CKD stages are based on estimated glomerular filtration rate (eGFR) and albuminuria (protein in urine).
- eGFR ≥90: Normal
- 60–89: Mildly reduced
- 30–59: Moderate (stage 3)
- 15–29: Severe (stage 4)
- <15: Kidney failure/ESKD (stage 5)
Albumin-to-creatinine ratio (ACR) adds critical risk information—more albumin in urine means higher risk for progression and heart problems.
Why wording matters for care decisions
The distinction between CKD, AKI, and ESKD guides testing, treatment choices, and urgency. It also affects lifestyle recommendations, medication adjustments, and planning for dialysis or transplant.
Consult Top Specialists
Early Signs and Symptoms of Kidney Failure
Here’s what to watch for so you can take action before kidney damage progresses:
Subtle early signs you might miss
- Early kidney disease is often silent. Subtle changes can include fatigue, night-time urination, ankle swelling, foamy urine (a sign of protein), poor appetite, and elevated blood pressure. Many people attribute these to ageing or stress.
- If you have diabetes, hypertension, or a family history, ask for kidney screening—even if you feel well..
Red flags that need urgent attention
Seek urgent evaluation for sudden swelling, shortness of breath, chest pain, very little urine output, severe nausea or vomiting, confusion, or persistent severe fatigue. These can indicate advanced CKD complications or AKI and may require hospital care.
When to seek medical care and what to expect
- If you notice ongoing swelling, rising blood pressure, or foamy urine for more than two weeks, connect with a clinician.
- You’ll likely have blood tests (creatinine/eGFR) and urine tests (ACR, urinalysis). Imaging may be ordered if obstruction or structural issues are suspected. Apollo 24|7 offers convenient home collection for tests like eGFR, ACR, and HbA1c, which can be useful if you have diabetes-related kidney risks.
- If symptoms persist beyond two weeks, consult a doctor online with Apollo 24|7 for further evaluation.
What Leads to Kidney Failure: Common Causes and Risk Factors
Here’s a closer look at what typically causes kidney failure and how to manage or prevent these triggers:
Diabetes and high blood pressure: the big two
Diabetes and hypertension account for the majority of CKD and kidney failure worldwide. In the UK and globally, most cases trace back to these two conditions. High blood glucose and high pressure damage the kidney’s filters (glomeruli) over time, causing albumin leakage and scarring.
Glomerular diseases and autoimmune causes
Diseases such as IgA nephropathy, focal segmental glomerulosclerosis (FSGS), lupus nephritis, and vasculitis inflame or scar kidney filters. They may cause blood or protein in urine, swelling, and rising blood pressure. Early diagnosis and targeted therapy (for example, immunosuppressants or renin–angiotensin system blockers) can slow progression.
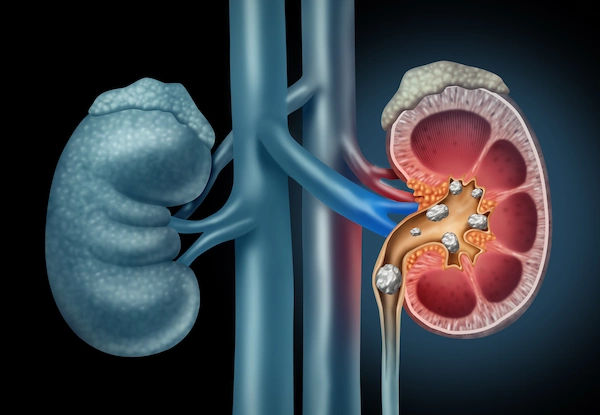
Structural problems: PKD, stones, obstruction
Polycystic kidney disease (PKD) is a genetic condition where cysts enlarge and damage kidneys. Recurrent kidney stones, enlarged prostate (BPH), or long-term obstruction (for example, strictures) can also lead to kidney failure by increasing pressure within the urinary tract and causing infections.
Recurrent infections, medications, and toxins
- Frequent kidney infections (pyelonephritis) can scar the kidneys. Certain medications—especially nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen—can reduce blood flow to the kidneys and raise risk, particularly in people with CKD, heart failure, or dehydration.
- Some antibiotics, contrast dyes, and herbal supplements can also harm kidneys. If you have CKD, discuss all over-the-counter drugs with your clinician and remember: avoid NSAIDs in kidney disease.
How Doctors Diagnose Kidney Problems
Here’s how diagnosis works—from simple blood tests to advanced imaging:
Blood tests: creatinine and eGFR
- Serum creatinine is used to estimate eGFR, adjusted for age and sex. eGFR trends are more informative than single values. A drop in eGFR or a rise in creatinine over days suggests AKI; gradual changes over months suggest CKD.
- Your clinician may also check electrolytes, bicarbonate, haemoglobin, and cholesterol to assess complications and cardiovascular risk.
Urine tests: albumin-to-creatinine ratio (ACR) and urinalysis
- Urine ACR detects small amounts of protein (albumin) that can signal early kidney damage—even when eGFR is near normal. Persistent ACR elevation (over three months) confirms CKD.
- A standard urinalysis can detect blood, protein, infection, or crystals (suggesting stones). Albumin-to-creatinine ratio testing at home via lab collection services (for example, Apollo 24|7) can help monitor trends between clinic visits.
Imaging and biopsy: when and why
- Ultrasound can reveal kidney size, cysts, stones, obstruction, or scarring. CT or MRI may be used in complex cases; contrast-enhanced studies require careful risk–benefit assessment in CKD to avoid AKI.
- Kidney biopsy helps diagnose glomerular diseases, guiding targeted treatment.
Risk scoring and staging your kidney health
Combining eGFR with ACR more accurately predicts progression and heart risk. Tools based on KDIGO risk heat maps help guide follow-up and management intensity. Ask your clinician where you fall on the “GFR–albuminuria grid.”
Management Essentials: Slowing CKD Progression
Here’s how to slow kidney decline and preserve function for as long as possible:
Blood pressure and sugar control (ACEi/ARBs, SGLT2, finerenone)
- Blood pressure: Tight control slows CKD; many guidelines support aiming for a systolic target near 120 mmHg (using standardised measurement) when tolerated. ACE inhibitors or ARBs lower pressure and reduce proteinuria—a protective effect for kidneys.
- Diabetes: Beyond glucose control, SGLT2 inhibitors (for example, empagliflozin, dapagliflozin) reduce CKD progression and kidney failure risk—even in some people without diabetes—based on major trials such as DAPA-CKD and EMPA-KIDNEY.
- Finerenone: For CKD and type 2 diabetes, finerenone (a nonsteroidal MRA) further lowers kidney and heart risks when added to ACEi/ARB therapy.
- Practical tip: Start low, go slow. Some medicines transiently lower eGFR; your clinician will monitor labs after medication changes.
Diet and lifestyle: sodium, protein, weight, and smoking
- Sodium: Aim for less than 2,000 mg per day. A low-sodium renal diet reduces blood pressure and swelling.
- Protein: Moderate intake (about 0.8 g/kg/day) is often recommended in CKD not on dialysis; very high-protein diets can increase kidney workload.
- Weight and activity: Sustained, gentle weight loss and regular walking lower blood pressure and improve insulin sensitivity—protective for kidneys.
- Smoking: Quitting slows CKD progression and protects blood vessels.
- Hidden phosphorus: Look for “phosphate additives” in processed foods and soft drinks; they worsen bone–mineral problems in CKD.
Medication review and avoiding nephrotoxins
- Avoid NSAIDs whenever possible in CKD; use alternatives recommended by your clinician.
- Review proton pump inhibitors (PPIs), contrast dyes, certain antibiotics, and herbal supplements.
- For contrast imaging, discuss hydration plans and alternative imaging if appropriate.
- Keep a medication list for every appointment; include all over-the-counter and herbal products.
Managing Symptoms and Complications
Here’s how to manage common CKD-related symptoms and secondary issues:
Anaemia, bone–mineral disease, and acidosis
- Anaemia: Low erythropoietin leads to fatigue and weakness. Management includes iron repletion and, if needed, erythropoiesis-stimulating agents; target haemoglobin is individualised.
- Bone/mineral: Disturbed calcium, phosphorus, and PTH can cause bone pain and fractures. Strategies include dietary phosphorus control, phosphate binders, vitamin D analogues, and calcimimetics as guided by labs.
- Acidosis: Low bicarbonate levels can accelerate CKD. Oral bicarbonate may help maintain a safe range.
Fluid and electrolyte balance (potassium, sodium, phosphorus)
- Potassium: High potassium (hyperkalaemia) can be dangerous. Limit high-potassium foods if levels are elevated, consider newer potassium binders, and adjust medications as needed.
- Sodium: Restrict to control blood pressure and oedema.
- Phosphorus: Avoid processed foods with phosphate additives; consider binders if required.
In later-stage CKD, potassium management often requires both diet changes and medication adjustments rather than diet alone.
Itching, sleep, and mental health support
- Itching (pruritus): Can be intense in advanced CKD; emollients, antihistamines, gabapentinoids, or newer agents may help.
- Sleep: Restless legs and insomnia are common; treatment improves quality of life.
- Mental health: Anxiety and low mood frequently accompany chronic illness. Counselling, peer support, and mindfulness practices can be powerful—don’t hesitate to ask for help.
Acute Kidney Injury: Recognise and Respond
Here’s how to spot and prevent sudden kidney injury:
Triggers: dehydration, infection, contrast dye, and surgery
- AKI often follows severe infection (sepsis), vomiting or diarrhoea, heat illness, blood loss, or medications that reduce kidney perfusion (NSAIDs, some blood pressure tablets during dehydration).
- Procedures using contrast dye raise risk, especially in CKD. Heatwaves are an under-recognised trigger; stay hydrated and cool in hot weather, especially if you work outdoors.
Sick day rules and prevention strategies
- Temporarily pause certain medicines during vomiting, diarrhoea, or poor oral intake (for example, ACEi/ARB, diuretics, metformin, SGLT2 inhibitors) until you’re eating and drinking normally—confirm a personalised plan with your clinician.
- Use oral rehydration solutions during illness.
- Before elective imaging or surgery, discuss AKI risk, hydration plans, and medication holds.
- Carry a “kidney wallet card” listing your baseline eGFR, risks, and sick day rules to reduce treatment errors during emergencies.
Hospital care and recovery timelines
AKI is managed by treating the cause, optimising fluids, carefully adjusting medications, and monitoring electrolytes. Recovery varies—some return to baseline, others develop CKD. Follow-up labs within weeks of discharge are crucial to track recovery and avoid missed progression.
When Kidney Function Falls: Preparing for Dialysis or Transplant
Here’s what to expect when kidney function drops significantly:
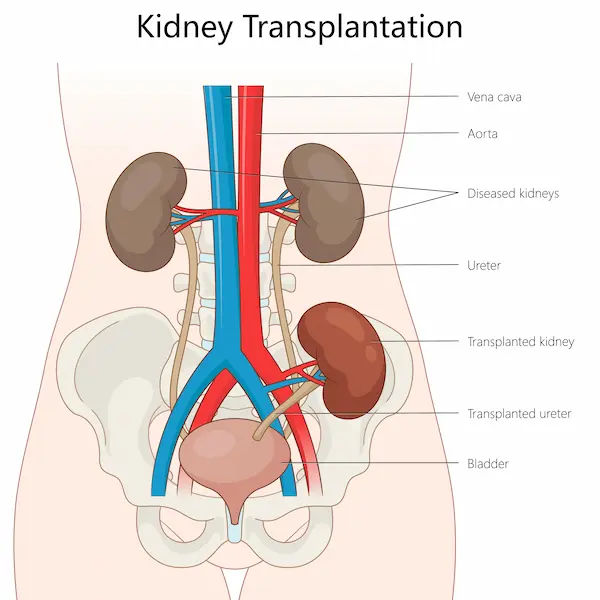
Treatment options: dialysis, transplant, conservative care
- Dialysis: Haemodialysis (in-centre or home) and peritoneal dialysis are options. Decision-making should start months before ESKD to allow smooth transition.
- Transplant: Generally offers longer survival and better quality of life than dialysis for eligible patients. Living donor transplant can reduce wait times.
- Conservative care: For some, focusing on symptom control without dialysis is appropriate. Shared decision-making is essential.
Access planning, timing, and quality of life
- Haemodialysis requires vascular access (arteriovenous fistula preferred) placed weeks to months before starting dialysis.
- Peritoneal dialysis requires a catheter and training but can be done at home and is often compatible with work schedules.
- Many people continue working or studying with the right dialysis modality and support. Ask to meet a dialysis educator early.
Transplant evaluation, waiting lists, and living donation
- Evaluation includes cardiac testing, infection screening, and cancer checks. Living donors (family or friends) can be evaluated confidentially. Paired exchange programmes can match incompatible pairs.
- While waiting, optimise fitness, vaccinations, and adherence to medications.
Prevention: Protecting Your Kidneys for Life
Here’s how to keep your kidneys healthy long term:
Who should be screened and how often
If you have diabetes, high blood pressure, heart disease, obesity, or a family history of kidney disease, ask for yearly eGFR and ACR testing. People over 60 may also benefit from periodic screening. Apollo 24|7 offers home collection for urine ACR and kidney panels, which can be convenient for regular monitoring.
Vaccines, infections, and heart–kidney protection
Vaccinations (flu, COVID-19, pneumococcal, hepatitis B when appropriate) reduce infection-related AKI. Treat UTIs promptly. Manage cholesterol and stop smoking to protect both kidney and heart health—these organs share many risks.
Heatwaves, hydration, and workplace/environmental risks
During hot weather or physically demanding work, schedule breaks, hydrate, and use shade or cooling. Aim for steady hydration, not over-drinking. Overhydration won’t “flush” kidneys and can worsen sodium balance; think “Goldilocks hydration”—not too little, not too much.
Conclusion
Kidney disease doesn’t happen overnight, and neither does kidney protection. The most powerful steps—controlling blood pressure and blood sugar, taking kidney-protective medicines, choosing a low-sodium diet, staying active, and avoiding nephrotoxic drugs—work best when started early and sustained over time. Learn to recognise subtle symptoms and red flags, and don’t skip routine screening if you have risk factors. Prevention and early management can delay or even avoid kidney failure for many people. If kidney function declines, you still have choices. From optimising medications to planning for dialysis or transplant, a shared, proactive care plan keeps you in the driver’s seat.
New therapies such as SGLT2 inhibitors and finerenone have changed the outlook for many with CKD, and practical strategies like sick day rules can prevent sudden setbacks. The key is partnership with your healthcare team and steady habits at home. If you’re concerned about symptoms, want a CKD diet check-in, or need help understanding your lab results, consult a doctor online with Apollo 24|7. If your condition doesn’t improve after trying these methods, book a physical visit to a doctor with Apollo 24|7. Apollo 24|7 also offers home collection for kidney panels, ACR, and diabetes labs to simplify follow-up. Small steps, taken consistently, add up to major kidney protection.
Consult Top Specialists
Consult Top Specialists

Dr. Manju Kamal
Nephrologist
12 Years • MBBS,MD(General Medicine), DNB,DM(Nephrology)
Angamaly
Apollo Hospitals Karukutty, Angamaly

Dr Madhav Desai
Nephrologist
22 Years • MBBS, MD, DM (Nephrology)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Sunil Jawale
Nephrologist
17 Years • MBBS, MD (Internal Medicine), DM (Nephrology)
Pune
Apollo Hospitals Pune, Pune
Dr. Umesh Chandra Sahu
Nephrologist
32 Years • MBBS,MD ( General Medicine ). Sr. Consultant ( Nephrology )
Rourkela
Apollo Hospitals, Rourkela, Rourkela

Dr Santosh Kumar
Nephrologist
13 Years • MD (Internal Medicine) DNB (Nephrology), MRCP – Nephrology (UK)
Lucknow
Apollomedics Super Speciality Hospital, Lucknow
Consult Top Specialists

Dr. Manju Kamal
Nephrologist
12 Years • MBBS,MD(General Medicine), DNB,DM(Nephrology)
Angamaly
Apollo Hospitals Karukutty, Angamaly

Dr Madhav Desai
Nephrologist
22 Years • MBBS, MD, DM (Nephrology)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Sunil Jawale
Nephrologist
17 Years • MBBS, MD (Internal Medicine), DM (Nephrology)
Pune
Apollo Hospitals Pune, Pune
Dr. Umesh Chandra Sahu
Nephrologist
32 Years • MBBS,MD ( General Medicine ). Sr. Consultant ( Nephrology )
Rourkela
Apollo Hospitals, Rourkela, Rourkela

Dr Santosh Kumar
Nephrologist
13 Years • MD (Internal Medicine) DNB (Nephrology), MRCP – Nephrology (UK)
Lucknow
Apollomedics Super Speciality Hospital, Lucknow
More articles from Kidney Failure
Frequently Asked Questions
What are early symptoms of kidney failure I should watch for?
Early symptoms can be subtle: fatigue, swelling, foamy urine, and rising blood pressure. If these persist, ask for an eGFR and albumin-to-creatinine ratio test. Early detection helps kidney failure management succeed.
How often should I check my kidney function if I have diabetes?
At least once a year for eGFR and ACR; more often if abnormal. SGLT2 inhibitors and ACEi/ARBs can reduce progression—ask if they’re right for you.
Which painkillers are safer if I have CKD?
Avoid NSAIDs in kidney disease when possible. Acetaminophen (paracetamol) is often preferred for occasional pain, but confirm with your clinician, especially if you have liver disease.
What’s the best diet for CKD?
A low sodium renal diet plan with moderate protein, plenty of whole foods, and limited processed foods (especially phosphate additives). Potassium or phosphorus limits depend on your labs—don’t restrict them unless advised.
How do I choose between dialysis and transplant?
Transplant often offers better survival and quality of life if you’re eligible. Dialysis choices include in-center hemodialysis, home hemodialysis, and peritoneal dialysis. Discuss pros/cons early with your care team to match your lifestyle and goals.