TARE Y90 Targeted Liver Cancer Therapy Guide
Learn about TARE Y90, a targeted therapy for liver cancer, how it works, its benefits, and what patients can expect during the procedure.

Written by Dr. J T Hema Pratima
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 13th Jan, 2026

Introduction
Facing a liver cancer diagnosis can feel overwhelming, especially when traditional surgery isn't a viable option. Fortunately, modern medicine offers advanced, minimally invasive treatments that target tumours with precision. TARE Y90 treatment, or Transarterial Radioembolisation, is a groundbreaking form of internal radiation therapy designed specifically for liver cancers. This innovative procedure delivers microscopic radioactive beads directly to the tumour, maximising damage to cancer cells while sparing the surrounding healthy liver tissue. If you or a loved one are exploring alternatives to surgery, this guide will walk you through everything you need to know about TARE Y90, from how it works and who it's for, to what you can expect during and after the procedure. We'll break down the complex science into understandable information to help you make informed decisions about your care.
What is TARE Y90 Radioembolisation?
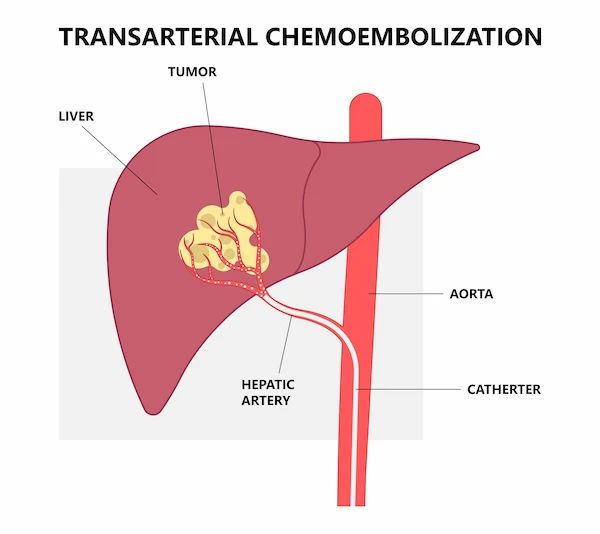
TARE Y90 is a highly specialised procedure performed by interventional radiologists to treat liver tumours. It's a two-pronged attack: it blocks the blood supply to the tumour (embolisation) while simultaneously delivering a high dose of radiation directly to it.
The "Y90" stands for Yttrium-90, a radioactive isotope. This isotope is embedded into tiny glass or resin beads called microspheres. These microspheres are so small, about one-third the width of a human hair, that they can be injected into the very small arteries that feed the liver tumour.
The Science Behind the Treatment: Radiation Microspheres
The genius of TARE Y90 lies in its biology. Liver tumours derive almost all their blood supply from the hepatic artery, while healthy liver tissue gets most of its supply from the portal vein. By injecting the radioactive microspheres through the hepatic artery, they travel directly to the tumour's doorstep. The beads then get lodged in the tiny vessels around the tumour, where they emit beta radiation, a powerful, short-range radiation for about two weeks. This radiation destroys the cancer cells from within, with minimal exposure to the rest of the body.
TARE vs. Other Liver Cancer Treatments
It's common to confuse TARE with other liver-directed therapies like TACE (Transarterial Chemoembolisation). While both are minimally invasive and delivered through the arteries, they work differently. TACE delivers chemotherapy drugs directly to the tumour and blocks its blood supply. TARE Y90, however, uses radiation instead of chemotherapy. This key difference often means TARE has a different side effect profile and can be suitable for patients who may not tolerate chemotherapy well.
Consult an Interventional Radiologist for the best advice
Who is a Candidate for TARE Y90 Therapy?
TARE Y90 is not a one-size-fits-all solution. It is specifically designed for patients with tumours that are confined to the liver, whether they originated there or spread from another organ.
Primary Liver Cancer (Hepatocellular Carcinoma - HCC)
For patients with HCC, TARE Y90 treatment is often recommended when the tumour is inoperable due to its size, location, or number, or if the patient's liver function isn't strong enough to withstand surgery. It can be used as a "bridge" to keep the cancer controlled while waiting for a liver transplant.
Secondary Liver Cancer (Metastases)
This is a common application. When cancers like colorectal cancer or neuroendocrine tumours spread to the liver, TARE can be a powerful tool to control that growth. It's often integrated with systemic chemotherapy to attack cancer both in the liver and throughout the body.
A key determinant is the BCLC Staging System (Barcelona Clinic Liver Cancer), which classifies liver cancer based on tumour stage, liver function, and overall health. TARE Y90 is typically indicated for intermediate-stage (BCLC B) patients, but its use is expanding into other stages based on ongoing research. Ultimately, a multidisciplinary team of oncologists, hepatologists, and interventional radiologists will determine if you are a good candidate for TARE Y90.
The TARE Y90 Procedure: A Step-by-Step Guide
The TARE procedure is typically performed in two separate outpatient sessions, usually a week or two apart.
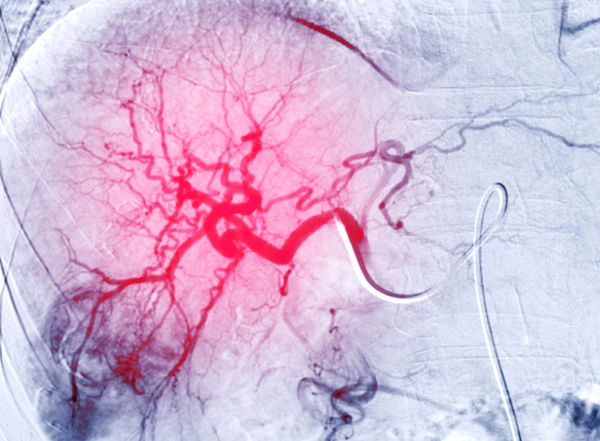
Phase 1: The Mapping Angiogram
This first step is crucial for planning and safety. The interventional radiologist inserts a thin catheter into an artery in the groin or wrist and guides it to the liver arteries using live X-ray (fluoroscopy). They inject a contrast dye to map the precise blood flow to the liver and the tumour.
The Role of Technetium-99m MAA Scan: During this mapping procedure, they inject a tiny amount of a radioactive tracer (Technetium-99m MAA) that mimics the size of the future Y90 microspheres. A subsequent scan shows where these particles would travel. This ensures no risk of the beads traveling to other organs like the lungs or stomach and allows the medical team to calculate the perfect dosage of radiation for the treatment day.
Phase 2: The Actual Y90 Treatment Day
The process for the treatment day is very similar to the mapping angiogram. Using the roadmap created in Phase 1, the radiologist guides the catheter to the exact spot. Then, instead of the tracer, they inject millions of Yttrium-90 microspheres. The procedure itself takes about 1-2 hours. You will be under sedation or light anaesthesia for comfort but will not require a general anesthetic. Most patients go home the same day after a short observation period.
Benefits and Advantages of Choosing TARE
The benefits of TARE Y90 are significant, making it a preferred option for many patients and clinicians.
Targeted Approach and Healthy Tissue Preservation
This is its biggest advantage. By delivering radiation directly to the tumour site, the success rate of radioembolisation in controlling local disease is high, while the impact on healthy liver tissue is minimised. This is vital for patients who already have compromised liver function.
Outpatient Procedure and Minimal Downtime
Unlike major surgery, TARE requires only a small puncture in the skin, not a large incision. This translates to a shorter hospital stay (often just a few hours), less pain, a lower risk of infection, and a faster recovery time after radioembolisation. Many patients can return to light activities within a week.
Potential Risks and Side Effects
Like any medical procedure, TARE Y90 carries potential risks. However, serious complications are rare when performed by an experienced team.
Common Side Effects (Post-Embolisation Syndrome)
This is a common group of symptoms that mimic the flu and are not a sign of something going wrong. They include:
• Fatigue
• Mild fever
• Nausea and abdominal pain
• Loss of appetite
These side effects of Y90 therapy are usually temporary and can be managed with medication. They typically resolve within a week or two.
Rare but Serious Complications
These are uncommon (<5% of cases) but can include:
• Radiation-induced liver disease (where the healthy part of the liver becomes inflamed).
• Ulcers in the stomach or intestine if beads accidentally travel there.
• Lung injury if a significant number of beads shunt to the lungs (which is why the mapping angiogram is so critical).
Your medical team will take every precaution to prevent these complications.
What to Expect After TARE Y90 Treatment
Understand the recovery process, possible side effects, and follow-up care after undergoing TARE Y90 therapy for liver cancer.
Immediate Recovery and Going Home
You will need someone to drive you home. You might feel tired and have some mild abdominal cramping. Doctors recommend resting for the first few days and staying well-hydrated. You will be given instructions on caring for the puncture site and managing any discomfort.
Follow-Up Care and Monitoring Effectiveness
You won't feel the radiation working, and it may take weeks or months to see the full effects. Follow-up is key. Your team will monitor you with periodic blood tests (tumour markers like AFP for HCC or CEA for colorectal mets) and imaging scans (like MRI or CT) every 3 months to see how the tumour is responding. If your recovery is unusually difficult or symptoms worsen, it's important to consult your doctor. For ongoing management, you can easily consult an oncologist online with Apollo24|7 to discuss your scan results and next steps.
Conclusion
TARE Y90 treatment represents a significant leap forward in the battle against liver cancer. It offers a powerful, targeted, and minimally invasive option for patients who may have previously felt they had few choices. By understanding the procedure, its benefits, and what to expect, you can actively participate in your treatment journey with confidence. While this guide provides a comprehensive overview, it is not a substitute for professional medical advice. If you have been diagnosed with liver cancer, discuss all potential treatment options, including TARE Y90, with your healthcare team to create a plan that is tailored to your individual needs and offers the best possible outcome.
Consult an Interventional Radiologist for the best advice
Consult an Interventional Radiologist for the best advice

Dr. Gandham Sohini
Radiologist
3 Years • MBBS,MD(Radiology)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir

Dr Sanket Kasliwal
Radiologist
6 Years • MBBS DMRE
Pune
Apollo Clinic, Kharadi, Pune

Dr. Savith Kumar
Interventional Radiologist
11 Years • MBBS, MD, FRCR, MMed, DM,
Bengaluru
Apollo Hospitals Bannerghatta Road, Bengaluru
Dr. Karthik H V
Radiologist
2 Years • MBBS MD(Radio-Diagnosis),DNB
Mysuru
Apollo Clinic, Mysore, Mysuru

Dr. Abid Hussain Gullenpet
Radiologist
23 Years • MBBS, DMRD, FRCR
Bengaluru
Apollo Clinic, JP nagar, Bengaluru
Consult an Interventional Radiologist for the best advice

Dr. Gandham Sohini
Radiologist
3 Years • MBBS,MD(Radiology)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir

Dr Sanket Kasliwal
Radiologist
6 Years • MBBS DMRE
Pune
Apollo Clinic, Kharadi, Pune

Dr. Savith Kumar
Interventional Radiologist
11 Years • MBBS, MD, FRCR, MMed, DM,
Bengaluru
Apollo Hospitals Bannerghatta Road, Bengaluru
Dr. Karthik H V
Radiologist
2 Years • MBBS MD(Radio-Diagnosis),DNB
Mysuru
Apollo Clinic, Mysore, Mysuru

Dr. Abid Hussain Gullenpet
Radiologist
23 Years • MBBS, DMRD, FRCR
Bengaluru
Apollo Clinic, JP nagar, Bengaluru
More articles from Liver Cancer
Frequently Asked Questions
1. Is the TARE Y90 treatment painful?
The procedure itself is not painful due to sedation. Afterwards, some patients experience manageable abdominal cramping or discomfort, similar to a heavy feeling, which is usually controlled with over-the-counter pain relievers.
2. What is the typical life expectancy after Y90 radioembolisation?
There is no single answer, as it depends heavily on the original cancer type, tumour burden,
3. How much does the TARE procedure cost?
The cost of TARE procedure can vary widely based on geographic location, the hospital, and insurance coverage. It is a complex treatment involving expensive materials. It's essential to consult with your insurance provider and the hospital's billing department to understand your specific financial responsibility.
4. How successful is TARE Y90?
Success rates of radioembolisation are high for controlling tumour growth within the liver. Studies show high rates of tumour response (shrinkage) and disease control. It is often measured by how well it stabilizes the cancer and prolongs survival, rather than always achieving a complete cure.
5. Can TARE Y90 cure liver cancer?
While it can sometimes completely eradicate tumours, especially smaller ones, its primary goal is often to control the disease, shrink tumours, and prolong life. In some cases, it can successfully 'downstage' a tumour to the point where it becomes operable or eligible for a transplant, which can be curative.