TARE Y90 Treatment; A Patient's Guide to Targeted Liver Cancer Therapy
Learn about TARE Y90 liver cancer treatment, how it works, eligibility, benefits, risks, and what to expect before, during, and after the procedure.

Written by Dr. J T Hema Pratima
Reviewed by Dr. Dhankecha Mayank Dineshbhai MBBS
Last updated on 13th Jan, 2026

Introduction
Facing a liver cancer diagnosis can feel overwhelming, with a flood of information about complex treatment options. If you or a loved one is exploring alternatives to surgery or chemotherapy, you may have come across the term TARE Y90. But what exactly is this advanced treatment? Transarterial Radioembolisation, or TARE Y90, is a highly targeted form of internal radiation therapy designed specifically for liver tumours. Think of it as a microscopic army delivering radiation directly to cancer cells while sparing the surrounding healthy liver tissue. This innovative procedure offers hope for patients with tumours that are difficult to remove surgically or have not responded to other treatments. This comprehensive guide will walk you through everything you need to know about TARE Y90—from how it works and who it's for, to what you can expect during and after the procedure. Our goal is to empower you with clear, patient-friendly information so you can have informed discussions with your healthcare team.
What is TARE Y90 Radioembolisation?
TARE Y90 stands for Transarterial Radioembolisation using Yttrium-90. It's a minimally invasive procedure that falls under the specialty of Interventional Radiology. Unlike external beam radiation, which projects rays through the skin to reach the tumour, TARE Y90 works from the inside out. It’s a two-part word: "Radioembolisation." "Radio" refers to the radiation delivered by Yttrium-90, a radioactive isotope. "Embolisation" means blocking blood flow. Together, the treatment blocks the tiny blood vessels that feed the tumour while simultaneously delivering a high dose of radiation directly to it.
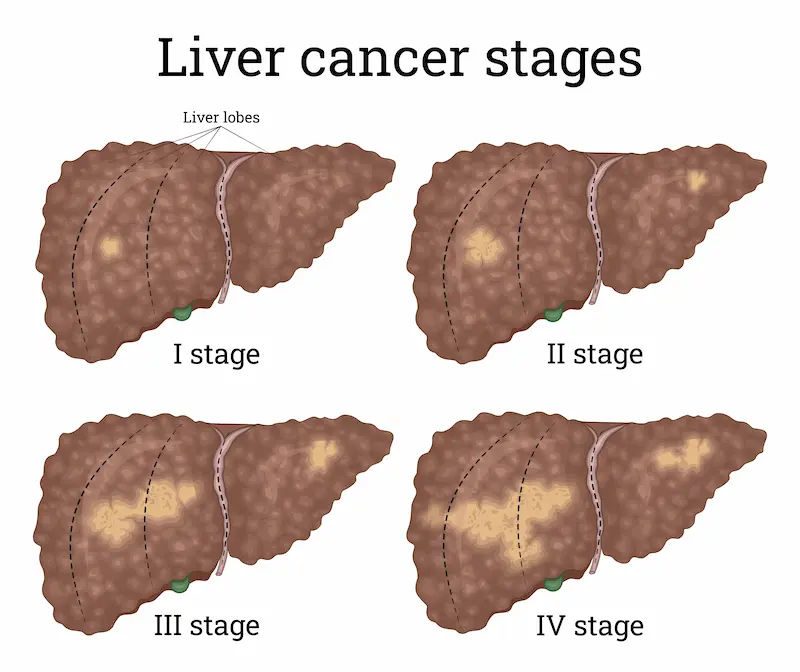
This dual-action approach makes TARE Y90 uniquely effective. It’s often described as a "smart bomb" for liver cancer because of its precision. The procedure is typically recommended for patients with primary liver cancer (Hepatocellular Carcinoma or HCC) or cancers that have spread to the liver from other parts of the body, such as colorectal cancer. For many, it can be a palliative Y90 treatment option that effectively controls tumour growth, alleviates symptoms, and improves quality of life, even if a cure isn't the immediate goal.
The "Inside-Out" Radiation Approach
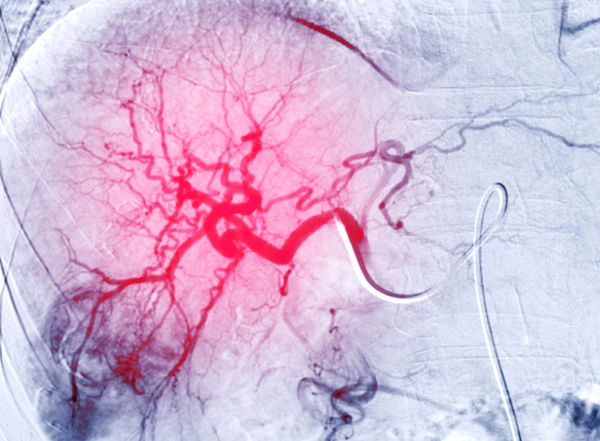
The genius of the TARE Y90 approach lies in biology. Liver tumours get their blood supply almost exclusively from the hepatic artery, while healthy liver tissue primarily relies on the portal vein. During the procedure, an interventional radiologist uses this to their advantage. They navigate a tiny catheter through the femoral artery in the groin up into the hepatic artery supplying the tumour. Then, millions of microscopic radioactive spheres (smaller than a human hair) are injected. These spheres flow directly to the tumour site, where they become lodged in the small vessels, cutting off the tumour's nutrient supply (embolisation) and bathing it in radiation from within.
TARE Y90 vs. Traditional Treatment Options
When comparing TARE Y90 vs. chemoembolisation (TACE), a key difference is the primary agent. TACE delivers chemotherapy drugs directly to the tumour, while TARE Y90 delivers radiation. TARE Y90 is often better tolerated because it typically lacks the severe systemic side effects of chemotherapy, such as significant hair loss or nausea. Compared to systemic chemotherapy or immunotherapy, which circulates throughout the entire body, TARE Y90 is a localised treatment, leading to fewer whole-body side effects. For patients with unresectable liver cancer (tumours that cannot be surgically removed), TARE Y90 can be a powerful option to control the disease locally within the liver.
Understanding How TARE Y90 Works
Here we explain how the therapy functions at a cellular and procedural level.
The Tiny Spheres That Pack a Powerful Punch
The active agents in this treatment are the Y90 microspheres. These are not simple liquid radiation; they are tiny, biocompatible glass or resin spheres impregnated with Yttrium-90. Yttrium-90 is a high-energy beta-ray emitter with a short half-life of about 64 hours. This means it delivers over 90% of its radiation dose within the first 11 days, effectively destroying cancer cells' DNA and causing tumour shrinkage, while the radioactivity dissipates to a safe level within two weeks. The spheres are permanently lodged in the tumour vasculature, posing no risk of travelling to other parts of the body after the procedure.
The Two-Step TARE Y90 Procedure: Mapping and Treatment
The TARE Y90 procedure is meticulously planned and executed in two separate sessions, usually a week or two apart.
The Mapping Angiogram (Simulation): This first step is crucial for safety and success. The interventional radiologist performs an angiogram to create a detailed "roadmap" of the liver's arteries. They inject a contrast dye to visualise blood flow using X-ray imaging. During this step, they often inject tiny non-radioactive particles (called Technetium-99m macroaggregated albumin or Tc-99m MAA) into the hepatic artery. A subsequent nuclear medicine scan (SPECT scan) shows where these particles travelled. This scan is vital to check if any particles might shunt to the lungs or gastrointestinal tract, which would require adjustments to prevent unintended radiation damage. If your doctor orders specific blood tests like liver function tests during this planning phase, Apollo24|7 offers convenient home collection services to simplify your preparation.
The Treatment Delivery: Based on the mapping results, a personalised dose of radioactive Y90 microspheres is calculated. During the treatment session, which is similar to the mapping procedure, the calculated dose is injected through the catheter directly into the arteries feeding the tumour. The procedure itself typically takes 1–2 hours, and patients are usually under conscious sedation rather than general anaesthesia.
Are You a Candidate for TARE Y90?
Eligibility depends on cancer type, liver function, and overall health.
Common Cancers Treated with Y90
TARE Y90 is primarily used for liver-dominant cancers. The most common indications include:
Hepatocellular Carcinoma (HCC): The most common form of primary liver cancer, especially when surgery isn't an option.
Metastatic Colorectal Cancer: When colorectal cancer spreads to the liver, TARE Y90 can effectively control these metastases.
Neuroendocrine Tumour (NET) Metastases: For liver metastases from NETs that are not amenable to surgery.
Cholangiocarcinoma: A cancer of the bile ducts within the liver.
Consult Top Specialists for Personalised Tips
Key Eligibility Factors Your Doctor Will Assess
Not everyone with liver tumours is a candidate. A multidisciplinary team of specialists will determine your eligibility based on several factors:
Liver Function: Your liver must be healthy enough to withstand the procedure. This is assessed through blood tests (bilirubin, albumin, INR) and clinical scoring systems.
Tumour Burden: The size, number, and location of tumours within the liver.
Overall Health: Your performance status and ability to recover from the procedure.
Blood Flow: The mapping angiogram must confirm that the tumours have a suitable blood supply from the hepatic artery and that the risk of shunting to the lungs is low.
Portal Vein Patency: While TARE Y90 can often be used in patients with portal vein thrombosis (a blockage in the main liver vein), it requires careful evaluation, which is a significant advantage over other embolisation techniques.
If you are unsure about your eligibility for this procedure, consulting a specialist oncologist or interventional radiologist is the best next step. You can consult a doctor online with Apollo24|7 to discuss your reports and get an initial opinion on whether TARE Y90 might be suitable for your specific case.
What to Expect: The TARE Y90 Treatment Journey
Knowing the step-by-step process can help you prepare mentally and physically.
Step 1: Pre-Procedure Consultation and Preparation
Once you are deemed a candidate, you will have a detailed consultation. You'll undergo pre-procedure tests, which may include blood work, imaging (like an MRI or CT scan), and an EKG. You will receive specific instructions, which may include fasting for several hours before the procedure and adjusting certain medications.
Step 2: The Day of the TARE Y90 Procedure
You will be admitted to the hospital or outpatient centre. An IV line will be placed for fluids and sedation. In the angiography suite, you will lie on an X-ray table. The area near your groin will be cleansed and numbed with local anaesthesia. You will be awake but sedated and comfortable. The radiologist will insert the catheter, and you may feel slight pressure but no pain. After the microspheres are delivered, the catheter is removed, and pressure is applied to the insertion site to prevent bleeding.
Step 3: Recovery and Post-Treatment Care
You will need to lie flat for a few hours after the procedure to ensure the puncture site heals. Most patients stay in the hospital overnight for observation. It's common to experience side effects of Y90 microspheres after the procedure, most notably "post-embolisation syndrome," which can include fatigue, mild fever, nausea, and abdominal pain for a few days to a week. These symptoms are manageable with medications. You will receive detailed instructions on post-procedure care, including any temporary radiation safety precautions (e.g., close contact with pregnant women or young children may be limited for a short period).
Benefits and Potential Risks of TARE Y90
Every treatment has pros and cons; understanding them helps in making an informed decision.
Key Advantages of Choosing Radioembolisation
Targeted Precision: Maximises tumour damage while sparing healthy liver tissue.
Minimally Invasive: No large incisions; faster recovery time after Y90 treatment compared to surgery.
Outpatient or Short Stay: Often performed as a same-day or 23-hour observation procedure.
Tolerable Side Effects: Generally fewer and less severe systemic side effects than chemotherapy.
Bridges to Other Treatments: Can shrink tumours to a size where they become operable or eligible for ablation (this is called "downstaging").
Improved Quality of Life: Effective for tumour control and symptom relief.
Understanding the Side Effects and Risks
While generally safe, potential risks exist. Common side effects include fatigue, nausea, abdominal pain, and fever (post-embolisation syndrome). Rare but serious risks include:
Radiation-induced liver disease (damage to healthy liver tissue).
Ulcers in the stomach or duodenum if microspheres travel incorrectly.
Injury to the lungs or gallbladder.
Damage to the injection site in the groin.
Your medical team will take every precaution during the mapping phase to minimise these risks.
Life After TARE Y90: Results and Follow-Up
After treatment, ongoing care and monitoring are vital for long-term success.
How Success is Measured
Success of Y90 radioembolisation is not always measured by immediate tumour disappearance. The primary goal is often to control growth. You will typically have a follow-up CT or MRI scan 4–6 weeks after treatment to assess initial response. Success is seen as tumour shrinkage or a lack of growth (stable disease). Tumour markers in the blood (like AFP for HCC or CEA for colorectal cancer) are also monitored for decreases.
Long-Term Monitoring and Healthy Living
Follow-up is a long-term commitment. You will have regular scans and blood tests to monitor the liver and check for any new tumour activity. Maintaining a healthy lifestyle is crucial. This includes a balanced diet, avoiding alcohol (which is toxic to the liver), and not smoking. If you experience persistent symptoms like worsening fatigue, jaundice (yellowing of the skin), or abdominal swelling after your recovery period, it is essential to consult your doctor promptly. You can book a follow-up physical visit to a doctor with Apollo24|7 to discuss your ongoing recovery and any concerns.
Conclusion
Navigating a liver cancer diagnosis is a challenging journey, but advanced treatments like TARE Y90 radioembolisation offer a powerful and targeted weapon against the disease. This guide has illuminated how this innovative procedure delivers radiation with pinpoint accuracy, providing a viable option for many patients for whom traditional surgery or chemotherapy may not be suitable. The key takeaway is that TARE Y90 represents a significant advancement in personalised cancer care, focusing on controlling tumour growth, preserving quality of life, and, in some cases, creating new pathways to curative treatments. While the decision to pursue any cancer treatment is deeply personal and should be made in close consultation with a dedicated medical team, understanding the mechanics, benefits, and journey of TARE Y90 empowers you to ask the right questions and advocate for your health.
Consult Top Specialists for Personalised Tips

Dr Syed Mateen Pasha
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Madhuri Sai Sreepada
General Practitioner
9 Years • MBBS
Hyderabad
BRIGHT SMILES MEDICARE & DENTAL CARE, Hyderabad

Dr. Johnson. S
General Practitioner
7 Years • MBBS MD(Preventive and social Medicine)
Pune
Apollo Clinic, Nigdi, Pune

Dr. Syed Ismail Ali
General Practitioner
7 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad