What Leads To Liver Cancer Risk Factors And Prevention
Know about liver cancer, what it is, types, cirrhosis, fatty liver disease types, symptoms, contributing factors for liver cancer and prevention


Introduction
Your liver is a silent workhorse, performing over 500 vital functions, from filtering toxins to processing nutrients. But when liver cancer develops, it often does so quietly, with symptoms appearing only at advanced stages. This makes understanding the risk factors for liver cancer not just important, but potentially life-saving. This article will demystify what leads to liver cancer, separating myth from fact and outlining the most significant risks, from widespread viral infections to modern lifestyle diseases. More importantly, we will provide a clear, actionable guide on prevention strategies you can start implementing today.
What is Liver Cancer? A Brief Overview
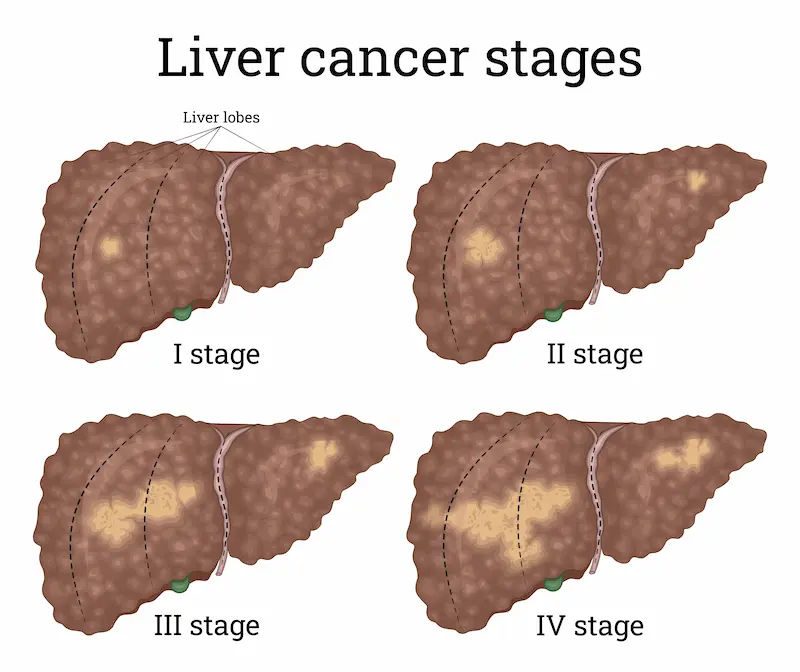
Liver cancer begins when healthy cells in the liver change and grow out of control, forming a malignant tumour. The most common type worldwide is hepatocellular carcinoma (HCC), which starts in the main liver cell type (hepatocyte). Understanding the basic types is crucial for context.
Primary vs. Secondary Liver Cancer
- Primary Liver Cancer: This is cancer that originates in the liver itself, like HCC. Our discussion of risk factors primarily pertains to this type.
- Secondary (Metastatic) Liver Cancer: This is more common and occurs when cancer from another organ (like the colon, breast, or lung) spreads (metastasises) to the liver. Its risk factors are tied to the original cancer.
The Major Risk Factors for Liver Cancer
The development of liver cancer is rarely due to a single cause. It's typically a result of several factors working together over time, often involving long-term damage and inflammation that leads to scarring (cirrhosis).
Consult an Oncologist for Personalised Advice
Chronic Viral Hepatitis: The Leading Cause
Globally, chronic infection with the hepatitis B virus (HBV) or hepatitis C virus (HCV) is the most significant liver cancer risk factor, contributing to the majority of cases.
Hepatitis B Virus (HBV) and Liver Cancer
The HBV virus can integrate its DNA into the host's liver cells, which can directly promote cancer development even before cirrhosis sets in. This is a key reason why HBV is a potent carcinogen. Vaccination against Hepatitis B is a powerful preventive measure.
Hepatitis C Virus (HCV) and Liver Cancer
Unlike HBV, HCV does not integrate its genetic material into the host DNA. Instead, it causes cancer almost exclusively through chronic inflammation, leading to cirrhosis over 20-30 years. The great news is that modern antiviral treatments can now cure over 95% of HCV infections, drastically reducing the future risk of hepatocellular carcinoma.
Cirrhosis: The Scarred Pathway to Cancer
Cirrhosis is a condition where healthy liver tissue is replaced by scar tissue, preventing the liver from functioning
properly. It is the end stage of many chronic liver diseases and is the strongest predictor of liver cancer development. Think of cirrhosis as the fertile ground in which cancer seeds can grow. The majority of HCC cases occur in livers already damaged by cirrhosis. The ongoing cycle of cell damage and regeneration in a cirrhotic liver increases the chance of genetic mutations that can lead to cancer.
Fatty Liver Disease: A Modern Epidemic
With rising rates of obesity and diabetes, fatty liver disease has emerged as a rapidly growing cause of liver cancer.
Alcoholic Fatty Liver Disease (AFLD)
Excessive alcohol consumption is a well-known toxin to liver cells. It can cause fat buildup (steatosis), inflammation (alcoholic hepatitis), and eventually, cirrhosis. This entire spectrum significantly elevates liver cancer risk.
Non-Alcoholic Fatty Liver Disease (NAFLD) and NASH
This is a concerning modern epidemic. NAFLD is the buildup of fat in the liver in people who drink little to no alcohol. Its more severe form, called non-alcoholic steatohepatitis (NASH), involves inflammation and liver cell damage. NASH can progress to cirrhosis and is now one of the fastest-rising reasons for liver cancer in many countries.
Dietary and Environmental Dangers
Aflatoxins in Contaminated Food
Aflatoxins are poisons produced by molds that grow on crops like corn, peanuts, and tree nuts that are stored in hot and humid conditions. Consuming food contaminated with aflatoxins poses a significant risk, particularly in certain parts of Asia and Africa. These toxins are potent carcinogens that can cause genetic mutations in the liver.
Excessive Alcohol Consumption
As highlighted under AFLD, heavy, long-term drinking is a direct pathway to liver damage. It's a dose-dependent risk: the more you drink regularly over time, the higher your chance of developing liver cirrhosis and cancer.
Other Contributing Factors and Conditions
Type 2 Diabetes and Metabolic Syndrome
People with type 2 diabetes, especially those who also have other features of metabolic syndrome (like high blood
pressure and high cholesterol), have a 2 to 3 times higher risk of liver cancer. This is often linked to the high prevalence of NAFLD in this population.
Obesity and Its Impact on Liver Health
Obesity is a primary driver of NAFLD and NASH. By promoting chronic inflammation and insulin resistance
throughout the body, excess body weight directly contributes to liver damage and increases cancer risk.
Genetic and Inherited Liver Diseases
Certain less common inherited conditions can damage the liver and increase risk. These include hemochromatosis (iron overload), Wilson's disease (copper overload), and autoimmune hepatitis. If you have a family history of liver disease, discussing screening for liver cancer with a doctor is prudent.
Proactive Prevention: How to Shield Your Liver
The good news is that many liver cancer risks are modifiable. Prevention is your most powerful tool.
Get Vaccinated and Practice Safe Habits
The hepatitis B vaccine is over 90% effective at preventing chronic HBV infection and is a cornerstone of liver cancer prevention. For Hepatitis C, there is no vaccine, but you can reduce your risk by avoiding unprotected sex and not sharing needles, razors, or toothbrushes.
Embrace a Liver-Healthy Diet and Lifestyle
- Diet: Focus on a plant-based diet rich in fruits, vegetables, and whole grains. Limit saturated fats, sugars, and processed foods. Be cautious of grains and nuts that appear moldy or are stored improperly to avoid aflatoxins.
- Alcohol: Drink in moderation, or not at all. The best approach for liver health is to avoid excessive alcohol
consumption entirely. - Exercise: Regular physical activity helps maintain a healthy weight and prevents fatty liver disease.
Manage Your Weight and Underlying Conditions
If you are overweight, even a 5-10% reduction in body weight can significantly improve liver health. Effectively
managing diabetes, high cholesterol, and triglycerides with the help of a doctor is also crucial.
The Critical Role of Regular Screening
For individuals at high risk (e.g., those with cirrhosis, chronic HBV, or a history of HCV), regular screening is vital.
This typically involves an abdominal ultrasound every six months. Early detection of liver cancer when tumours are
small and treatable dramatically improves survival outcomes. If you fall into a high-risk category, consult a doctor
online with Apollo24|7 to create a personalised screening plan.
Conclusion
Understanding what leads to liver cancer empowers you to take control of your health. While some factors like genetics are beyond our control, the most significant risks—chronic viral hepatitis, cirrhosis, fatty liver disease, and lifestyle choices—can be mitigated through awareness and action. Prevention hinges on a multi-pronged approach: get vaccinated, drink responsibly, maintain a healthy weight through a balanced diet and regular exercise, and be vigilant about storing food safely. Most importantly, if you have any known liver condition or fall into a high-risk category, partnering with a healthcare professional for regular monitoring is non-negotiable. If you have concerns about your liver health or need to discuss a personalised prevention strategy, booking a consultation with a specialist through Apollo24|7 is a proactive first step.
Consult an Oncologist for Personalised Advice
Consult an Oncologist for Personalised Advice

Dr.sanchayan Mandal
Medical Oncologist
17 Years • MBBS, DrNB( MEDICAL ONCOLOGY), DNB (RADIOTHERAPY),ECMO. PDCR. ASCO
Kolkata
Dr. Sanchayan Mandal Oncology Clinic, Kolkata

Dr. Sanchayan Mandal
Medical Oncologist
17 Years • MBBS, DNB Raditherapy, DrNB Medical Oncology
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr Gowshikk Rajkumar
Oncologist
10 Years • MBBS, DMRT, DNB in Radiation oncology
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Gopal Kumar
Head, Neck and Thyroid Cancer Surgeon
15 Years • MBBS, MS , FARHNS ( Seoul, South Korea ), FGOLF ( MSKCC, New York )
Delhi
Apollo Hospitals Indraprastha, Delhi
(25+ Patients)

Dr. Raja T
Oncologist
20 Years • MBBS; MD; DM
Chennai
Apollo Hospitals Greams Road, Chennai
(200+ Patients)
Consult an Oncologist for Personalised Advice

Dr.sanchayan Mandal
Medical Oncologist
17 Years • MBBS, DrNB( MEDICAL ONCOLOGY), DNB (RADIOTHERAPY),ECMO. PDCR. ASCO
Kolkata
Dr. Sanchayan Mandal Oncology Clinic, Kolkata

Dr. Sanchayan Mandal
Medical Oncologist
17 Years • MBBS, DNB Raditherapy, DrNB Medical Oncology
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr Gowshikk Rajkumar
Oncologist
10 Years • MBBS, DMRT, DNB in Radiation oncology
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Gopal Kumar
Head, Neck and Thyroid Cancer Surgeon
15 Years • MBBS, MS , FARHNS ( Seoul, South Korea ), FGOLF ( MSKCC, New York )
Delhi
Apollo Hospitals Indraprastha, Delhi
(25+ Patients)

Dr. Raja T
Oncologist
20 Years • MBBS; MD; DM
Chennai
Apollo Hospitals Greams Road, Chennai
(200+ Patients)
More articles from Liver Cancer
Frequently Asked Questions
1. Can you get liver cancer if you don't drink alcohol?
Yes, absolutely. While heavy alcohol use is a major risk factor, many non-alcohol-related conditions like chronic viral hepatitis (B and C), non-alcoholic fatty liver disease (NAFLD), and autoimmune diseases can also lead to cirrhosis and liver cancer.
2. What are the early warning signs of liver cancer?
Early liver cancer often has no symptoms. When present, signs can be vague and include unexplained weight loss, loss of appetite, feeling very full after a small meal, nausea, pain in the upper right abdomen, and general fatigue. Jaundice (yellowing of the skin and eyes) is a sign of more advanced disease.
3. Is liver cancer hereditary?
Most cases are not directly inherited. However, you can inherit a higher susceptibility or genetic conditions that increase your risk, such as hemochromatosis or Wilson's disease. A family history of liver cancer or chronic liver disease should prompt a discussion with your doctor.
4. How can I check my liver health at home?
You cannot thoroughly check your liver health at home. While being aware of symptoms is important, many liver diseases are silent. The best way to assess liver health is through medical tests. Apollo24|7 offers convenient home collection for liver function tests (LFTs) and other panels that your doctor may recommend.
5. Does fatty liver always lead to cancer?
No, not always. Simple fatty liver (NAFLD without inflammation) often doesn't progress. However, if it advances to its inflammatory form (NASH), the risk of developing cirrhosis and subsequently liver cancer increases significantly. Lifestyle changes can often reverse simple fatty liver.