Guide to Tace Transarterial Chemoembolization
Learn about TACE (Transarterial Chemoembolization), a targeted treatment for liver cancer. Understand its procedure, benefits, risks, and recovery process.

Written by Dr. Rohinipriyanka Pondugula
Reviewed by Dr. Md Yusuf Shareef MBBS
Last updated on 13th Jan, 2026

Facing a liver cancer diagnosis can be overwhelming, and the array of treatment options can feel confusing. Among these options, you may have heard of a procedure called TACE, or Transarterial Chemoembolization. This minimally invasive treatment has become a cornerstone of care for many patients with liver tumors, offering a targeted approach that differs significantly from traditional chemotherapy. But what exactly is it, how does it work, and what can you expect? This guide will walk you through everything you need to know about TACE, breaking down the complex medical jargon into clear, understandable information. We'll cover the procedure step-by-step, its benefits and risks, the recovery process, and how it fits into a comprehensive cancer care plan, empowering you to have informed discussions with your healthcare team.
What is TACE? Understanding the Basics
Transarterial Chemoembolization (TACE) is a minimally invasive procedure performed by interventional radiologists to treat liver cancers. It's uniquely designed to deliver a high dose of chemotherapy directly to a liver tumor while simultaneously cutting off its blood supply. Think of it as a targeted siege on a castle: the chemotherapy attacks the walls (cancer cells), while the embolization blocks the supply routes (blood vessels), starving the defenders.
The Meaning Behind the Name: Chemo + Embolization
The name perfectly describes the two-part action:
Chemo: Chemotherapy drugs are injected directly into the blood vessels feeding the tumor.
Embolization: Tiny particles (microspheres or gel foam) are injected to block, or "embolize," these same blood vessels.
This combination is what makes TACE therapy for liver tumors so effective. By trapping the chemotherapy drugs right where they are needed most, the procedure maximizes the dose to the cancer while minimizing exposure to the rest of the body.
TACE vs. Traditional Chemotherapy: What's the Difference?
This is a crucial distinction. Traditional chemotherapy is systemic—it travels through your entire bloodstream, affecting both cancerous and healthy cells, which leads to widespread side effects like hair loss, severe nausea, and weakened immunity. TACE, however, is a localized or regional therapy. Its effects are concentrated primarily in the liver, which typically results in fewer and less severe systemic side effects. This makes it a viable option for patients who may not be able to tolerate full-body chemotherapy.
Consult a Top Oncologist
How Does the TACE Procedure Actually Work?
The mechanism of TACE is a clever application of human anatomy. Liver tumors derive almost all their blood supply from the hepatic artery, while healthy liver tissue gets most of its blood from the portal vein. TACE exploits this difference by targeting the hepatic artery.
The Dual-Action Attack on Cancer Cells
1. High-Dose Chemo Delivery: The chemotherapy drugs are delivered directly into the branches of the hepatic artery that lead to the tumor. This creates a massively high concentration of cancer-killing agents right at the source.
2. Starvation via Embolization: The embolic agents then follow, clogging up the small arteries. This blocks the oxygen and nutrients the tumor needs to survive, effectively starving it. It also traps the chemotherapy drugs inside the tumor, allowing them to work for a longer period.
A Step-by-Step Walkthrough of the TACE Process
Understanding the TACE procedure steps can greatly reduce anxiety. Here’s what typically happens:
1. You will receive mild sedation or general anesthesia to ensure you are comfortable and pain-free.
2. The interventional radiologist makes a tiny incision, usually in the groin area.
3. A thin, flexible tube called a catheter is threaded through the femoral artery and guided all the way up to the hepatic artery in the liver using live X-ray imaging (fluoroscopy).
4. A contrast dye is injected to create a map of the blood vessels and pinpoint the exact vessels feeding the tumor.
5. The chemotherapy and embolic agent mixture is carefully injected through the catheter directly into those target vessels.
6. The catheter is removed, and pressure is applied to the small incision site to prevent bleeding. No stitches are needed.
The entire TACE procedure usually takes between 1 to 2 hours.
Who is a Candidate for TACE Therapy?
TACE is not for everyone, but it is a leading option for a specific group of patients. The decision is made by a multidisciplinary team of oncologists, surgeons, and interventional radiologists.
Primary Liver Cancer: The Most Common Candidate
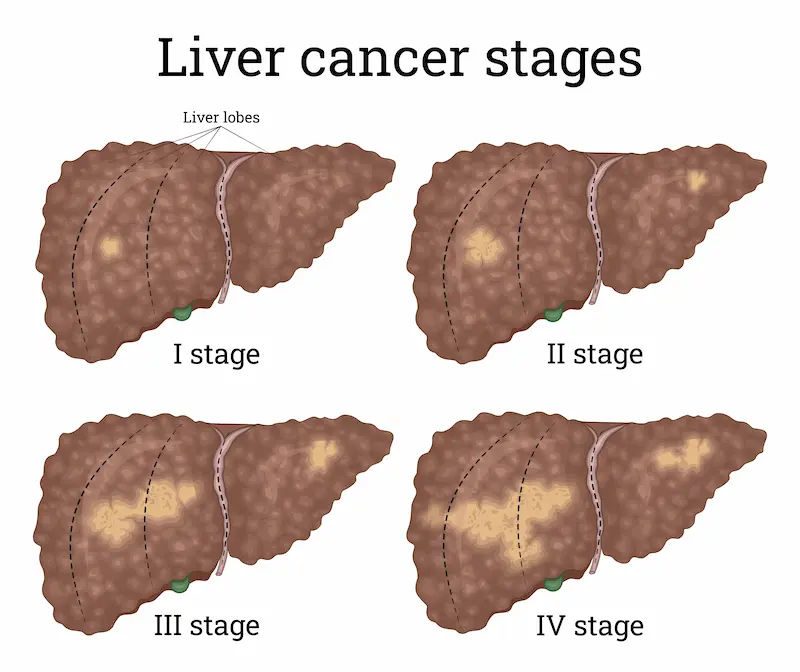
The most frequent use of TACE is for hepatocellular carcinoma (HCC), the most common type of primary liver cancer. It is often recommended for patients with intermediate-stage (Barcelona Clinic Liver Cancer Stage B) tumors that are too large or too numerous for surgical removal (unresectable) or ablation but have not yet spread extensively outside the liver.
Secondary Liver Cancers: When Cancer Spreads
TACE can also be highly effective for metastatic liver cancer, particularly cancers that originated in the colon or rectum (colorectal metastases). It can be used to control growth in the liver when surgery isn't an option.
Key Factors Your Doctor Will Consider
Candidacy depends on several factors:
Tumor characteristics: Number, size, and location of tumors within the liver.
Liver function: How well the non-cancerous part of your liver is working (often assessed by the Child-Pugh score).
Overall health: Your performance status and ability to withstand the procedure.
Blood flow: Confirmation that the tumor gets its blood supply from the hepatic artery.
Unique Insight: While often used for intermediate-stage cancer, emerging research is exploring "downstaging" using TACE to shrink large tumors enough to make a patient eligible for a curative treatment like liver transplant or resection, fundamentally changing their prognosis.
Conclusion
Transarterial Chemoembolization (TACE) represents a significant advancement in the fight against liver cancer, offering a powerful, targeted strategy that can control tumor growth, shrink lesions, and prolong survival for many patients. While it is not a cure, it is a crucial tool that provides hope and an improved quality of life by focusing its effects precisely where they are needed. Understanding the procedure, its benefits, and the recovery process empowers you to be an active participant in your care journey. If you or a loved one has been diagnosed with liver cancer, discuss with your oncologist whether TACE could be a suitable part of your treatment plan. For a personalized evaluation and to discuss your specific case with a specialist, you can consult an expert oncologist online with Apollo24|7.
Consult a Top Oncologist
Consult a Top Oncologist

Dr.sanchayan Mandal
Medical Oncologist
17 Years • MBBS, DrNB( MEDICAL ONCOLOGY), DNB (RADIOTHERAPY),ECMO. PDCR. ASCO
Kolkata
Dr. Sanchayan Mandal Oncology Clinic, Kolkata

Dr. Sanchayan Mandal
Medical Oncologist
17 Years • MBBS, DrNB( MEDICAL ONCOLOGY), DNB (RADIOTHERAPY),ECMO. PDCR. ASCO
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr. Sanchayan Mandal
Medical Oncologist
17 Years • MBBS, DNB Raditherapy, DrNB Medical Oncology
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr Gowshikk Rajkumar
Oncologist
10 Years • MBBS, DMRT, DNB in Radiation oncology
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Gopal Kumar
Head, Neck and Thyroid Cancer Surgeon
15 Years • MBBS, MS , FARHNS ( Seoul, South Korea ), FGOLF ( MSKCC, New York )
Delhi
Apollo Hospitals Indraprastha, Delhi
(25+ Patients)
More articles from Liver Cancer
Frequently Asked Questions
1. Is TACE treatment painful?
During the procedure, you will be under sedation or anesthesia and won't feel pain. Afterwards, it is common to experience discomfort, cramping, or pain in the upper abdomen or right shoulder due to the embolization. This is effectively managed with pain medication provided by your hospital team.
2. What is the life expectancy after TACE?
Survival rates vary widely based on the individual's cancer stage, liver function, overall health, and response to treatment. Studies show median survival rates ranging from 16 to 28 months for patients with hepatocellular carcinoma treated with TACE. Your doctor can provide a more personalized prognosis based on your specific situation.
3. How successful is TACE at shrinking tumors?
TACE has a high technical success rate in delivering treatment. In terms of tumor response, studies show that over 50% of patients experience significant tumor shrinkage (objective response) when assessed a few months after the procedure using standardized criteria (mRECIST).
4. Can TACE cure liver cancer?
TACE is rarely considered a curative treatment on its own. It is a locoregional therapy aimed at controlling the cancer within the liver, slowing its progression, and extending life. In some cases, if it successfully downstages the cancer, it may make a patient eligible for a potentially curative treatment like surgery or transplant.
5. How many TACE sessions will I need?
The number of sessions needed varies. It often requires a series of treatments, typically repeated every 2-3 months, depending on how the tumor responds. Your medical team will use follow-up imaging scans after each session to determine if and when another TACE procedure is necessary.