What Leads To Signs Of Liver Cancer And
Learn what leads to the signs and symptoms of liver cancer, including its causes, risk factors, early indicators, and diagnosis methods for timely detection.

Written by Dr. Dhankecha Mayank Dineshbhai
Reviewed by Dr. Vasanthasree Nair MBBS
Last updated on 13th Jan, 2026

Introduction
Liver cancer can be difficult to spot early because the liver is a resilient organ with an extraordinary ability to compensate when injured. By the time clear signs show up, the cancer may already be advanced. Understanding what leads to the signs and symptoms of liver cancer gives you a powerful head start: you’ll know which changes in your body matter, what to do next, and how to lower your risk.
In this comprehensive guide, written for the general public, we explain how liver cancer develops, why symptoms appear, which risk factors matter most, and when to see a doctor. We’ll also break down how liver cancer is diagnosed and treated, what prevention and screening look like, and how daily life can be managed if you or a loved one faces this disease.
If any symptoms persist beyond two weeks, or you’re worried about your risk, consider consulting a doctor online with Apollo 24|7 for further evaluation. Early attention—especially for people with cirrhosis, hepatitis B or C, or fatty liver disease—can make a real difference.
Liver Cancer: Types, How It Starts, and Who It Affects
Know all about liver cancer here:
1. The Main Types
- Hepatocellular carcinoma (HCC): The most common primary liver cancer, starting in hepatocytes (liver cells). Often
develops on a background of cirrhosis from hepatitis B or C, alcohol-related liver disease, or nonalcoholic fatty liver
disease (NAFLD/NASH). - Intrahepatic cholangiocarcinoma (ICC): Cancer starting in the bile ducts inside the liver; symptoms can skew toward jaundice and itching due to blocked bile flow.
- Metastatic liver cancer: Many cancers (colon, breast, lung, pancreas) spread to the liver. Symptoms can be similar but
causes and treatments differ.
2. How Liver Cancer Begins
- Chronic injury → inflammation → scarring (fibrosis/cirrhosis) → genetic changes → cancer.
- Key culprits include hepatitis B and C, heavy alcohol use, and NAFLD/NASH linked to diabetes and obesity.
- Aflatoxin exposure (a mould toxin in poorly stored grains/nuts) remains a major cause in some regions.
3. Who Is Most at Risk
- People with cirrhosis from any cause.
- Chronic HBV carriers (even without cirrhosis), especially Asian men over 40, Asian women over 50, people from sub-
Saharan Africa over 20, and anyone with a family history of liver cancer. - People with long-standing diabetes, obesity, or metabolic syndrome tied to fatty liver (NAFLD/NASH).
Why Do Liver Cancer Symptoms Happen?
Here are the reasons why the symptoms occur:
1. Pressure and Stretching Cause Pain
As a tumour grows, it can stretch the liver capsule, causing a dull ache in the upper right abdomen or even pain felt in
the right shoulder due to shared nerve pathways.
2. Bile Backup Leads to Jaundice and Itching
Tumours that block bile ducts can cause bilirubin to build up, yellowing the skin and eyes (jaundice). The same backup
triggers intense itching.
3. Portal Hypertension Drives Fluid Buildup
When tumours and scarring disrupt blood flow through the liver, pressure builds in the portal vein, leading to
abdominal fluid (ascites), leg swelling, and enlarged veins that can bleed.
4. Tumour “Signals” Cause Whole-Body Symptoms
Cancer cells can release substances that lead to fever, fatigue, weight loss, poor appetite, and rare effects such as low
blood sugar or increased red blood cell counts.
In people with cirrhosis, early liver cancer symptoms often hide behind cirrhosis symptoms. The earliest clues are
sometimes subtle changes like a new ache, a slight worsening in energy, or a sudden increase in bilirubin.
Consult Liver Specialists Here
Early Signs vs. Later Symptoms: What to Watch For
Here are the early symptoms to watch out for:
1. Early Signs (Often Subtle)
- Unexplained fatigue and low energy
- Mild, persistent right upper abdominal discomfort
- Decreased appetite or feeling full quickly
- Unintended weight loss
- Slightly abnormal liver tests (found on routine bloodwork)
2. Later Symptoms (More Obvious)
- Jaundice (yellowing of eyes/skin), dark urine, pale stools
- Worsening abdominal swelling (ascites) and leg swelling
- Increasing right-sided pain, sometimes radiating to the shoulder
- Nausea, vomiting, severe fatigue, and significant weight loss
- Easy bruising or bleeding; occasionally vomiting blood
- Itching, fever, or confusion from toxin buildup
3. Symptoms Specific to Tumour Location
- Tumours near major bile ducts: more jaundice and itching
- Multifocal tumours in cirrhotic livers: earlier fluid buildup and bleeding risk
- Large solitary tumours: a palpable mass or pressure sensation
When to act: If you notice jaundice, vomiting blood, increasing abdominal swelling, severe persistent pain, or major
weight loss, seek medical care immediately. If symptoms last beyond two weeks, consult a doctor online with Apollo 24
|7.
What Leads to Liver Cancer?
Major risk factors you can and can’t change include:
1. Viral Hepatitis
- Hepatitis B (HBV): A major global driver; vaccine-preventable. Chronic HBV can lead to cancer with or without
cirrhosis. - Hepatitis C (HCV): Curable with modern antivirals, but prior damage can persist.
2. Cirrhosis from Any Cause
Cirrhosis due to alcohol-related liver disease, NAFLD/NASH, autoimmune hepatitis, primary biliary cholangitis,
primary sclerosing cholangitis, and certain genetic conditions can all increase risk.
3. Metabolic and Lifestyle Factors
Type 2 diabetes, obesity, metabolic syndrome, and smoking increase risk. NAFLD-linked HCC is the fastest-rising
subtype in many countries.
4. Environmental Exposures and Others
Aflatoxins in contaminated food and chronic arsenic exposure in water in some regions are known risks. Long-term
anabolic steroid use may also contribute.
When Should You See a Doctor?
See when to consult a doctor here:
1. Red Flags Requiring Urgent Attention
- Jaundice, vomiting blood, black stools, confusion, severe abdominal pain, or rapid belly swelling may signal advanced
disease or bleeding and need emergency care.
2. Persistent or Unexplained Symptoms
Fatigue, appetite loss, right-sided ache, or weight loss lasting more than two weeks should prompt medical review.
Apollo 24|7 offers online consultations for evaluation.
3. Higher-Risk Groups
If you have cirrhosis, chronic HBV or HCV, or NAFLD with diabetes/obesity, ask about surveillance every six months
with liver ultrasound (with or without AFP).
How Doctors Diagnose Liver Cancer: Tests, Imaging, and Staging
Here’s how doctors diagnose liver cancer:
1. Blood Tests
Liver enzymes, bilirubin, alkaline phosphatase, albumin, clotting tests, and AFP are assessed. AFP helps alongside
imaging but isn’t diagnostic on its own.
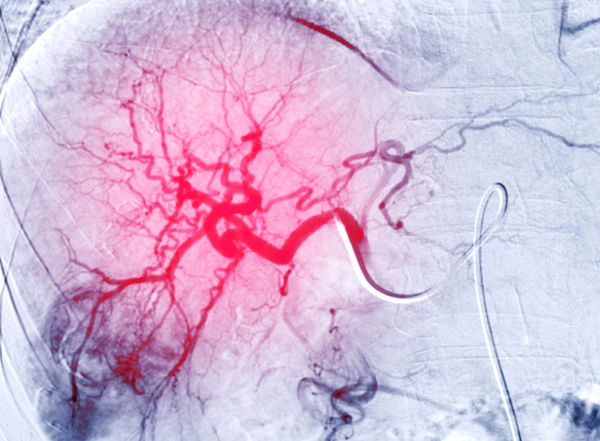
2. Imaging
- Ultrasound: First-line for surveillance and initial evaluation.
- Contrast-enhanced CT or MRI: Diagnostic for HCC when showing arterial-phase enhancement with venous
“washout.” - MRI with liver-specific contrast or MRCP: Used for bile duct evaluation.
3. Biopsy
Not always required if imaging is typical. It’s needed for atypical cases, non-cirrhotic livers, or when ICC/metastasis is
suspected.
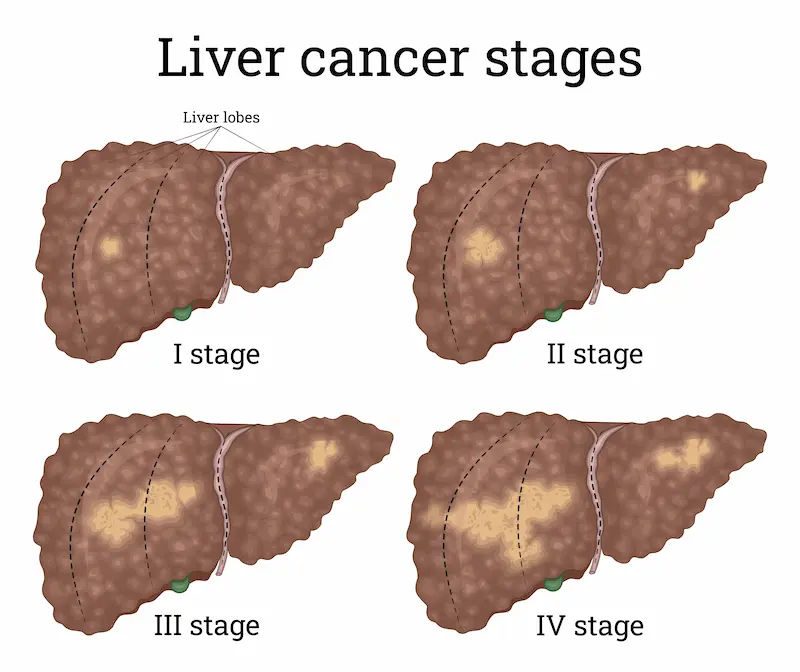
4. Staging and Liver Function Assessment
The BCLC system integrates tumour size, liver function, and patient fitness to guide treatment.
Treatment Options by Stage: From Cure to Control
1. Curative-Intent Options
- Surgical resection: Best for single tumours in patients with preserved liver function.
- Liver transplantation: Ideal for early-stage cases meeting transplant criteria.
- Ablation (RFA/MWA): Destroys small tumours using heat, with outcomes comparable to surgery for small lesions.
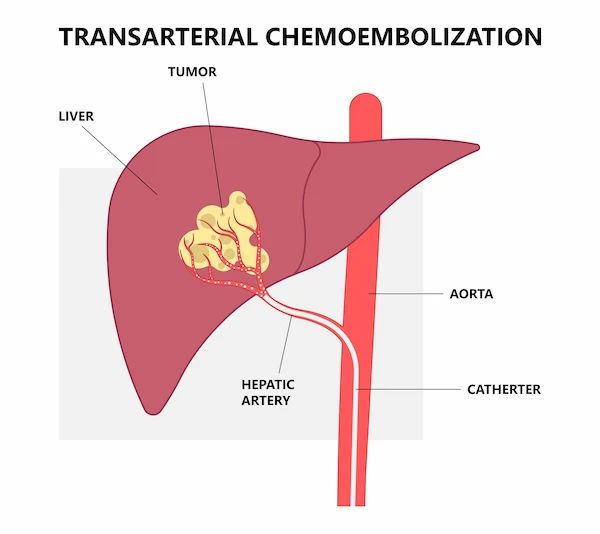
2. Liver-Directed Therapies
- TACE: Blocks blood supply and delivers chemotherapy locally.
- Radioembolisation (TARE/Y-90): Delivers radiation via arteries.
- SBRT: Focused radiation for those unfit for other therapies.
3. Systemic Therapies
- Immunotherapy combinations: Atezolizumab + bevacizumab or durvalumab + tremelimumab.
- Targeted therapies and TKIs: Lenvatinib, sorafenib, regorafenib, cabozantinib, ramucirumab.
- Single-agent immunotherapy: Nivolumab or pembrolizumab in selected cases.
4. Palliative and Supportive Care
Symptom control, nutrition support, and emotional care are essential at all stages.
Prevention and Screening: What You Can Do Now
Here’s how you can prevent liver cancer:
1. Prevent What You Can
- Vaccinate against hepatitis B.
- Get tested and treated for hepatitis C.
- Moderate alcohol, quit smoking, and maintain a healthy weight.
- Reduce aflatoxin exposure by storing food properly.
2. Who Needs Screening
- All adults with cirrhosis, regardless of cause.
- HBV carriers at higher risk (by age, ethnicity, or family history).
- Some patients with advanced fibrosis due to NASH.
3. How Screening Works
Ultrasound every six months, with or without AFP blood test. If an abnormality is found, proceed to CT or MRI.
Living With and After Liver Cancer: Daily Life, Diet, and Support
Here’s how you can make lifestyle adjustments to live with liver cancer:
1. Nutrition and Activity
Small, frequent meals can help with fullness; prioritise protein to prevent muscle loss. A dietitian familiar with liver
disease can assist.
2. Managing Common Symptoms
- Ascites: Low-salt diet and diuretics.
- Itching: Bile acid sequestrants and gentle skincare.
- Pain: Specialist-guided pain management without excessive sedation.
3. Emotional Health
Anxiety and low mood are common. Support groups, counselling, and palliative care can improve wellbeing at any
stage.
Myths vs. Facts You Should Know
1. Myth: “All Liver Pain Means Cancer.”
Fact: Most liver pain isn’t cancer. Gallbladder issues or gastritis are often the cause, but persistent pain should be
checked.
2. Myth: “Detox Teas Cleanse the Liver.”
Fact: The liver naturally detoxifies. Some supplements can harm it. Prevention via vaccination, treatment, and healthy
habits is safer.
3. Myth: “If AFP Is Normal, I Can’t Have Liver Cancer.”
Fact: Many HCCs don’t raise AFP. Imaging remains essential for diagnosis.
Special Considerations: Women, Older Adults, and People With Diabetes
Here are some special considerations to keep in mind:
1. Women
Symptoms may be subtle. Women with HBV, HCV, or cirrhosis should ask about screening.
2. Older Adults
Treatment decisions should balance other health issues; minimally invasive or immunotherapy options may be suitable.
3. Diabetes and Metabolic Risk
Diabetes raises HCC risk even without alcohol use. People with fatty liver and diabetes should discuss surveillance.
Consult Liver Specialists Here
Conclusion
Liver cancer develops quietly, and its signs can be easy to miss because the liver compensates so well—until it can’t. Understanding what leads to the symptoms—pressure on the liver capsule, blocked bile flow, increased portal pressure, and whole-body effects—helps you recognise them early.
If you have cirrhosis, hepatitis B or C, heavy alcohol use, or fatty liver linked to metabolic syndrome, you’re at higher risk and should ask about regular screening every six months. If you notice persistent right-sided abdominal discomfort, appetite loss, fatigue, unexplained weight loss, jaundice, or increasing belly swelling, don’t wait.
Diagnosis typically involves imaging (contrast CT or MRI), lab tests, and sometimes biopsy; treatments are increasingly effective and tailored to your stage and liver function. Prevention remains powerful: vaccination, viral hepatitis treatment, and lifestyle steps can reduce risk.
If your symptoms persist beyond two weeks or you’re concerned about your risk, consult a doctor online with Apollo 24|7 for guidance and consider Apollo 24|7’s home collection for relevant tests. Awareness and timely action are your best tools to change the trajectory of liver cancer.
Consult Liver Specialists Here
Consult Liver Specialists Here

Dr. Srinivasa Reddy
Hepatologist
12 Years • MBBS, MD (General Medicine), DM (Hepatology),ASGE
Hyderabad
Myra Liver & Gastro Care, Hyderabad

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(150+ Patients)

Dr. Aswin S. Krishna
Hepatologist
10 Years • MBBS, MD (Internal Medicine,MMC), DM (Hepatology, MMC), PDF(Fellowship in Liver Transplanatation)
Chennai
Apollo Hospitals Greams Road, Chennai
(125+ Patients)

Dr. Pukhraj Singh Jeji
Gastroenterology/gi Medicine Specialist
13 Years • MBBS, MD ( Internal Medicine ), DM ( Gastroenterology ), Consultant - Gastroenterology
Bhubaneswar
Apollo Hospitals Old Sainik School Road, Bhubaneswar

Dr. Murugan N
Hepatologist
18 Years • MBBS, MRCPI, FRCPG
Chennai
Apollo Hospitals Greams Road, Chennai
(425+ Patients)
Consult Liver Specialists Here

Dr. Srinivasa Reddy
Hepatologist
12 Years • MBBS, MD (General Medicine), DM (Hepatology),ASGE
Hyderabad
Myra Liver & Gastro Care, Hyderabad

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(150+ Patients)

Dr. Aswin S. Krishna
Hepatologist
10 Years • MBBS, MD (Internal Medicine,MMC), DM (Hepatology, MMC), PDF(Fellowship in Liver Transplanatation)
Chennai
Apollo Hospitals Greams Road, Chennai
(125+ Patients)

Dr. Pukhraj Singh Jeji
Gastroenterology/gi Medicine Specialist
13 Years • MBBS, MD ( Internal Medicine ), DM ( Gastroenterology ), Consultant - Gastroenterology
Bhubaneswar
Apollo Hospitals Old Sainik School Road, Bhubaneswar

Dr. Murugan N
Hepatologist
18 Years • MBBS, MRCPI, FRCPG
Chennai
Apollo Hospitals Greams Road, Chennai
(425+ Patients)
Consult Liver Specialists Here

Dr. Srinivasa Reddy
Hepatologist
12 Years • MBBS, MD (General Medicine), DM (Hepatology),ASGE
Hyderabad
Myra Liver & Gastro Care, Hyderabad

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(150+ Patients)

Dr. Aswin S. Krishna
Hepatologist
10 Years • MBBS, MD (Internal Medicine,MMC), DM (Hepatology, MMC), PDF(Fellowship in Liver Transplanatation)
Chennai
Apollo Hospitals Greams Road, Chennai
(125+ Patients)

Dr. Pukhraj Singh Jeji
Gastroenterology/gi Medicine Specialist
13 Years • MBBS, MD ( Internal Medicine ), DM ( Gastroenterology ), Consultant - Gastroenterology
Bhubaneswar
Apollo Hospitals Old Sainik School Road, Bhubaneswar

Dr. Murugan N
Hepatologist
18 Years • MBBS, MRCPI, FRCPG
Chennai
Apollo Hospitals Greams Road, Chennai
(425+ Patients)
More articles from Liver Cancer
Frequently Asked Questions
1) What are the earliest warning signs of liver cancer?
Early signs can include fatigue, mild right-upper-abdominal discomfort, feeling full quickly, and unintended weight loss.
2) Can fatty liver lead to cancer even if I don’t drink?
Yes. Nonalcoholic fatty liver disease can progress to scarring and cancer. Ask your doctor about fibrosis assessment and screening.
3) How is liver cancer diagnosed without a biopsy?
Contrast CT or MRI showing arterial enhancement with venous washout can diagnose HCC in many cases.
4) What treatment options exist for advanced liver cancer?
Options include immunotherapy combinations, targeted therapies, and liver-directed treatments in select cases.
5) Who needs regular screening for liver cancer?
All patients with cirrhosis, chronic HBV at high risk, and some with advanced NASH-related fibrosis should undergo ultrasound screening every six months.