Guide to Link Between Diabetes And Liver Disease
Explore the link between diabetes and liver disease. Learn how diabetes increases the risk of fatty liver, symptoms to watch for, and strategies for prevention and management.

Written by Dr. Rohinipriyanka Pondugula
Reviewed by Dr. D Bhanu Prakash MBBS, AFIH, Advanced certificate in critical care medicine, Fellowship in critical care medicine
Last updated on 13th Jan, 2026

Introduction
Diabetes is widely known for its impact on blood sugar levels, but its effects extend far beyond, with one of the most significant and often overlooked organs being the liver. This vital organ plays a crucial role in metabolising sugars and fats, making it highly susceptible to the metabolic chaos caused by diabetes. If you have type 2 diabetes, you are at a substantially higher risk of developing a serious liver condition known as non-alcoholic fatty liver disease (NAFLD). This comprehensive guide will explore the intricate, two-way relationship between diabetes and liver health. We will break down how one condition fuels the other, identify the often-silent symptoms, and provide actionable strategies for prevention, management, and protecting your long-term health. Understanding this link is your first step toward taking proactive control of your well-being.
Understanding the Liver's Role in Your Body
The Liver's Multitasking Marvel: More Than Just Detox
While most people associate the liver with detoxification, its responsibilities are vast and vital. Think of it as the body's central processing unit. It regulates fuel supply by storing excess glucose as glycogen and releasing it when needed. It manufactures essential proteins, produces bile to digest fats, and filters toxins from the blood. When this complex organ is compromised by conditions like diabetes, its ability to perform these life-sustaining functions dwindles, creating a cascade of metabolic problems.
Consult a Hepatologist for the best advice
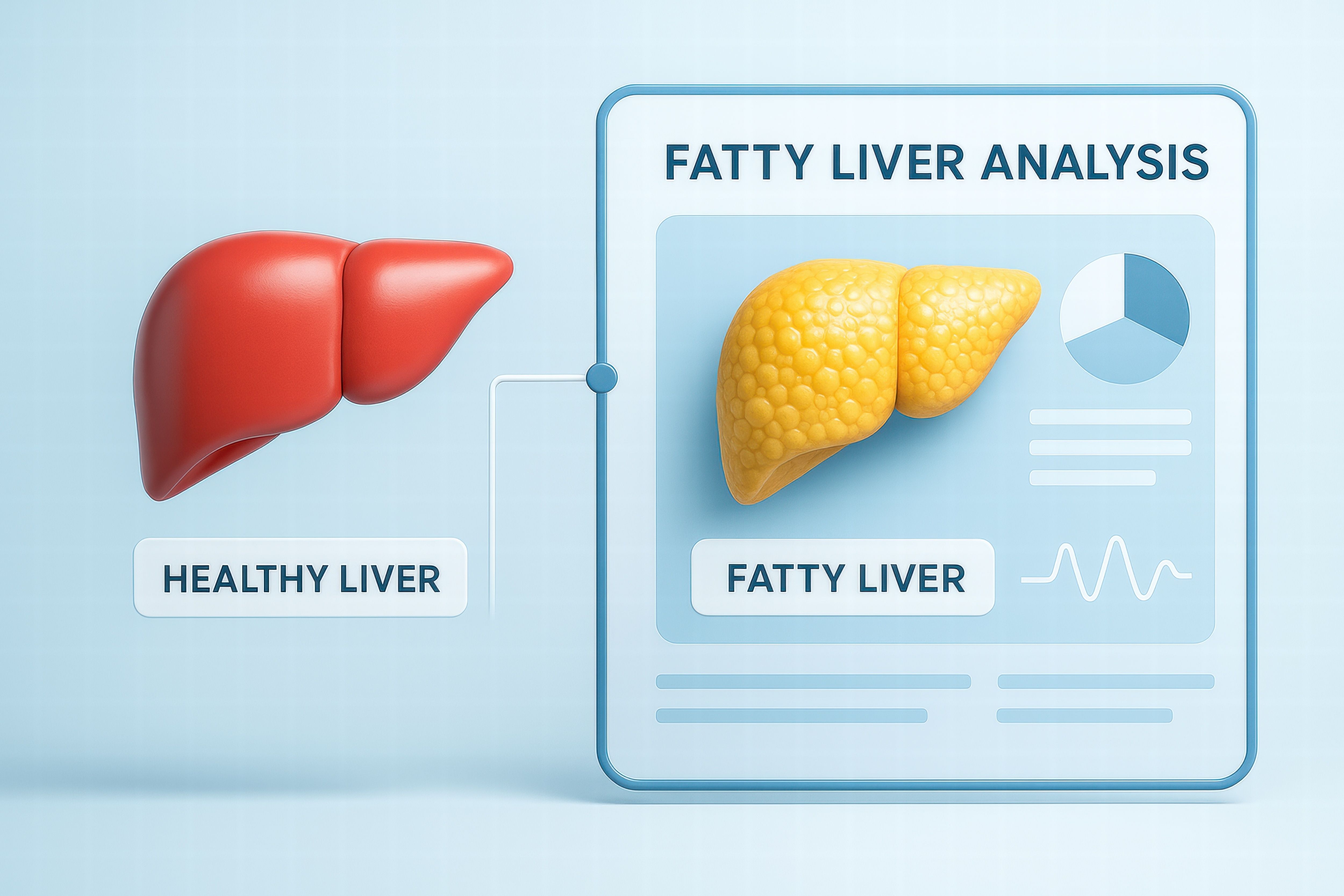
What is Non-Alcoholic Fatty Liver Disease (NAFLD)?
Non-alcoholic fatty liver disease (NAFLD) is an umbrella term for a range of liver conditions affecting people who drink little to no alcohol. As the name implies, it's characterised by an excessive buildup of fat in liver cells. It is intimately linked with insulin resistance and is considered the hepatic manifestation of metabolic syndrome.
From Simple Fatty Liver to NASH: The Spectrum of Disease
NAFLD encompasses two main stages:
Simple Fatty Liver (Steatosis): This is the initial, more benign stage where fat is present in the liver but with little to no inflammation or cell damage. Many people live with this without it progressing.
Non-Alcoholic Steatohepatitis (NASH): This is a more aggressive form where the fat accumulation is accompanied by liver inflammation and cell damage. This inflammation can lead to scarring (fibrosis) and is a major risk factor for advanced liver disease.
Why NAFLD is a Major Concern for Public Health
NAFLD has become the most common chronic liver disease globally, paralleling the rise in obesity and type 2 diabetes. Its significance lies in its potential to progress silently to severe complications, making early detection and management in at-risk populations, like diabetics, absolutely critical.
The Diabetes-Liver Disease Connection: A Two-Way Street
The relationship between diabetes and liver disease is cyclical and self-perpetuating. One doesn't just cause the other; they actively make each other worse.
How Insulin Resistance Fuels Fat Buildup in the Liver
In type 2 diabetes, the body's cells become resistant to insulin. To compensate, the pancreas produces even more insulin (hyperinsulinaemia). This high level of insulin tells the liver to increase fat production (lipogenesis) while also impairing the liver's ability to export that fat. This double whammy causes triglycerides to accumulate within the liver cells, leading to steatosis—the first step toward liver disease.
How a Diseased Liver Worsens Diabetes Control
A healthy liver helps regulate blood sugar by storing and releasing glucose as needed. A fatty, inflamed liver loses this precision. It becomes less responsive to insulin's signals to stop producing glucose, leading to the liver dumping unnecessary sugar into the bloodstream. This contributes to fasting hyperglycaemia (high blood sugar after fasting), making diabetes significantly harder to control and often requiring higher doses of medication.
Recognising the Signs and Symptoms
The Silent Nature of Early Liver Disease
One of the most challenging aspects of NAFLD and early NASH is its silence. In the initial stages, it often presents no symptoms at all. This is why routine screening is so important for individuals with diabetes, as the disease can progress significantly before any signs appear.
When to Seek Medical Advice: Red Flags
As the disease advances, some symptoms may emerge. If you experience any of the following, it's crucial to consult a doctor:
Persistent fatigue and weakness
Pain or discomfort in the upper right abdomen
Unexplained weight loss
Jaundice (yellowing of the skin and eyes)
Swelling in the legs (edema) or abdomen (ascites)
If you have diabetes and are experiencing persistent abdominal discomfort or unusual fatigue, consult a doctor online with Apollo24|7 for further evaluation. Early consultation can make a significant difference in outcomes.
How is Liver Disease Diagnosed in Diabetics?
Diagnosis typically involves a multi-step process, especially since symptoms of fatty liver in diabetics are often absent.
Blood Tests and Liver Function Tests (LFTs)
Routine blood work can reveal elevated liver enzymes (ALT and AST), which are markers of liver inflammation. However, enzyme levels can be normal even with advanced disease, so they are not a perfect screening tool.
Imaging Techniques: Ultrasound, FibroScan, and MRI
Ultrasound: Often the first imaging test, it can detect the presence of fat in the liver.
FibroScan® (Transient Elastography): This is a specialised, non-invasive ultrasound that measures liver stiffness, which correlates with scarring (fibrosis). It's a crucial tool for staging the disease without a biopsy.
MRI: More advanced MRI techniques can precisely quantify liver fat and fibrosis.
The Role of Liver Biopsy in Staging Fibrosis
A liver biopsy, where a small sample of tissue is extracted for analysis, remains the gold standard for diagnosing NASH and determining the exact stage of fibrosis. It is typically recommended if other tests are inconclusive or if advanced disease is suspected.
Get Your Health Assessed
Effective Management and Treatment Strategies
The primary goal of managing NAFLD with diabetes is to reduce liver fat, inflammation, and fibrosis by addressing the underlying metabolic drivers.
The Cornerstone of Treatment: Lifestyle Modification
There is no medication specifically approved for NAFLD/NASH yet. Lifestyle changes are the most effective treatment.
Dietary Changes for Liver and Diabetic Health
Adopting a best diet for diabetic fatty liver is essential. Focus on:
Reducing Sugars and Refined Carbs: Eliminate sugary drinks and highly processed foods.
Choosing Healthy Fats: Incorporate sources of monounsaturated (olive oil, avocados, nuts) and omega-3 (fatty fish) fats.
Increasing Fiber: Eat plenty of vegetables, whole grains, and legumes.
Avoiding Fructose: High-fructose corn syrup, found in many processed foods, is particularly harmful to the liver.
The Power of Regular Physical Activity
Exercise improves insulin sensitivity and directly helps reduce liver fat, independent of weight loss. Aim for a mix of:
Aerobic Exercise: At least 150 minutes of moderate-intensity exercise (brisk walking, cycling) per week.
Resistance Training: At least 2 sessions per week to build muscle, which is a major site for glucose disposal.
Medications: Managing Diabetes to Protect the Liver
Some diabetes medications have beneficial effects on the liver:
Pioglitazone: An insulin-sensitiser shown to improve NASH in many patients.
GLP-1 Receptor Agonists (e.g., liraglutide, semaglutide): These drugs aid significant weight loss and have been shown to resolve NASH in a considerable number of patients.
Vitamin E: An antioxidant that has shown benefit in non-diabetic adults with NASH, though its use must be discussed with a doctor due to potential risks.
Managing the right medication regimen is complex. If your condition does not improve after trying these methods, book a physical visit to a doctor with Apollo24|7 to discuss the best pharmacological approach for your specific situation.
Emerging Treatments and Therapies for NASH
A robust pipeline of new drugs is in development, targeting various pathways of NASH progression, including inflammation, fibrosis, and metabolism. These represent a hopeful future for NASH diabetes treatment options.
Potential Complications if Left Unmanaged
Ignoring the link between type 2 diabetes and liver health can lead to severe, irreversible consequences.
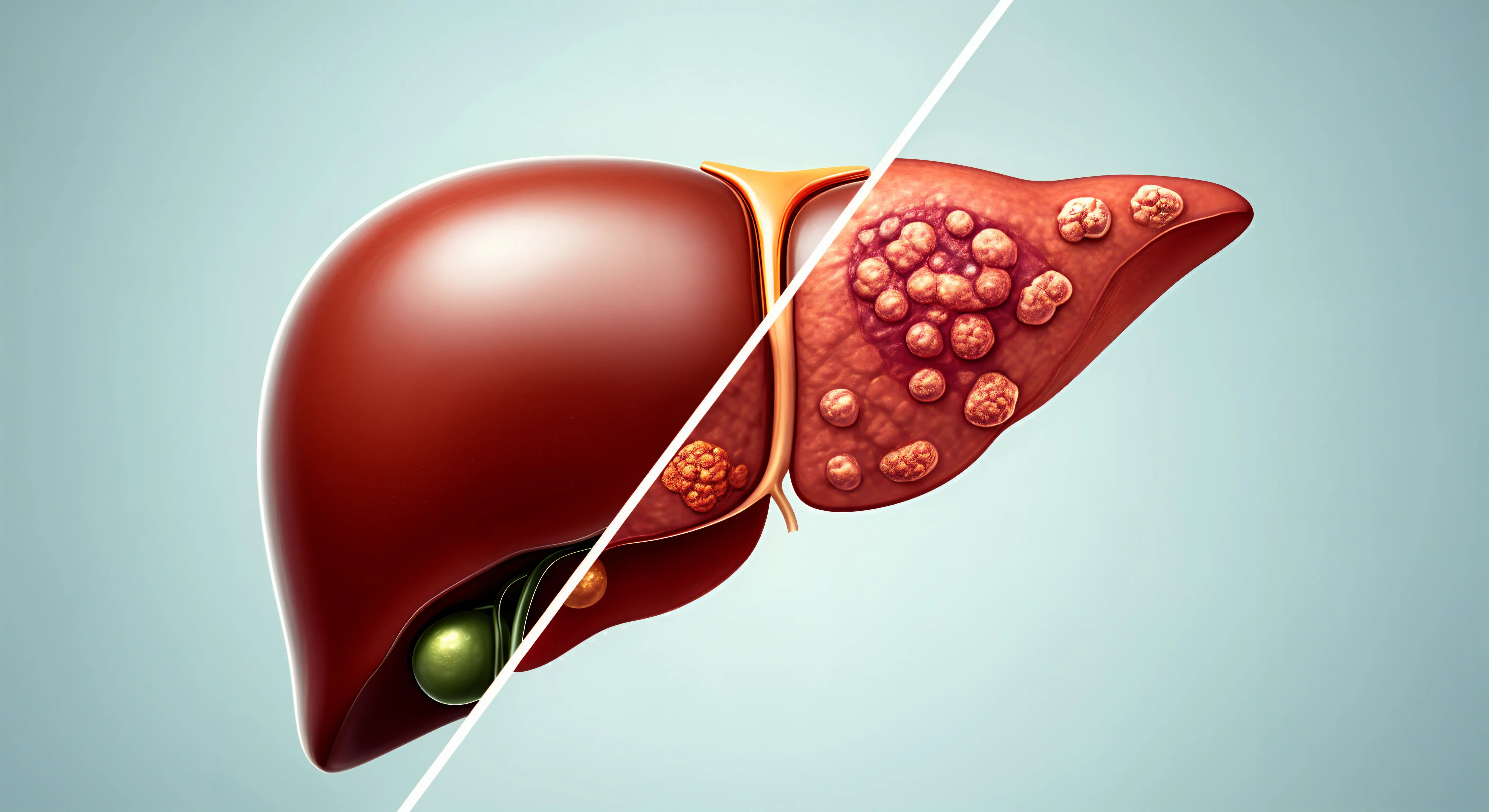
Liver Cirrhosis and Liver Failure
Persistent inflammation leads to fibrosis, which can progress to cirrhosis—the scarring and hardening of the liver. Cirrhosis impairs liver function and can eventually lead to liver failure, a life-threatening condition.
Increased Risk of Hepatocellular Carcinoma (Liver Cancer)
Individuals with cirrhosis from NASH have a significantly increased risk of developing liver cancer. Regular surveillance with ultrasound is recommended for those with advanced cirrhosis.
Prevention: Safeguarding Your Liver Health
Regular Monitoring and Screening for Diabetics
Given the silent progression, all individuals with type 2 diabetes should be screened for NAFLD. This typically involves an annual LFT test. Apollo24|7 offers convenient home collection for tests like liver function panels or HbA1c, making regular monitoring effortless.
Building Sustainable Healthy Habits
Prevention is fundamentally about the same lifestyle measures used for treatment: maintaining a healthy weight, eating a balanced diet, and staying physically active. It's about managing your diabetes as effectively as possible to protect your liver.
Conclusion
The connection between diabetes and liver disease is a critical aspect of metabolic health that demands attention. While the statistics may seem daunting, the power to change the trajectory of this disease lies largely in your hands. By understanding this link, you are already ahead. Proactive management of your blood sugar, commitment to a healthy lifestyle, and regular check-ups with your healthcare provider are the pillars of protecting your liver. Remember, is fatty liver disease reversible? In its early stages, yes, it often is. The liver possesses a remarkable ability to heal itself when the underlying insults are removed. Don't wait for symptoms to appear. Take charge of your health today by discussing liver screening with your doctor and making sustainable choices that benefit your entire metabolic system.
Consult a Hepatologist for the best advice
Consult a Hepatologist for the best advice

Dr. Srinivasa Reddy
Hepatologist
12 Years • MBBS, MD (General Medicine), DM (Hepatology),ASGE
Hyderabad
Myra Liver & Gastro Care, Hyderabad

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(150+ Patients)

Dr. Aswin S. Krishna
Hepatologist
10 Years • MBBS, MD (Internal Medicine,MMC), DM (Hepatology, MMC), PDF(Fellowship in Liver Transplanatation)
Chennai
Apollo Hospitals Greams Road, Chennai
(125+ Patients)

Dr. Pukhraj Singh Jeji
Gastroenterology/gi Medicine Specialist
13 Years • MBBS, MD ( Internal Medicine ), DM ( Gastroenterology ), Consultant - Gastroenterology
Bhubaneswar
Apollo Hospitals Old Sainik School Road, Bhubaneswar

Dr U V U Vamsidhar Reddy
Hepatologist
10 Years • MBBS, MD (JIPMER), DM (Hepatology, PGIMER)
Chennai
Apollo Hospitals Greams Road, Chennai
(75+ Patients)
More articles from Liver disease
Frequently Asked Questions
1. Can you have fatty liver disease without having diabetes?
2. What are the best foods to eat for a fatty liver if you are diabetic?
Focus on whole, unprocessed foods: leafy greens, fatty fish (salmon, mackerel), nuts (walnuts, almonds), olive oil, avocados, and whole grains like oats and quinoa. These foods fight inflammation and improve insulin sensitivity.
3. Are there any specific drinks I should avoid?
Yes. Sugary sodas, fruit juices, and any beverages with high-fructose corn syrup are extremely harmful to the liver. Alcohol should also be avoided or strictly limited, as it adds additional strain on the liver.
4. How much weight loss is needed to improve NAFLD?
Significant improvement in liver fat and inflammation can be seen with a weight loss of 7-10% of your total body weight. For a 200-pound person, that's 14 to 20 pounds.
5. What is the difference between NAFLD and alcoholic liver disease?
The liver damage looks very similar under a microscope, but the cause is different. NAFLD is not caused by alcohol consumption but by metabolic problems. Alcoholic liver disease is directly caused by excessive alcohol intake.