Guide to Can Hepatitis C Be Cured Liver Transplant
Exploring the role of liver transplantation in treating Hepatitis C. Understand the cure rates, risks, and treatment options available after a transplant.

Written by Dr. Dhankecha Mayank Dineshbhai
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 13th Jan, 2026
.webp?tr=q-80,f-webp,w-350,dpr-2,c-at_max 700w)
Introduction
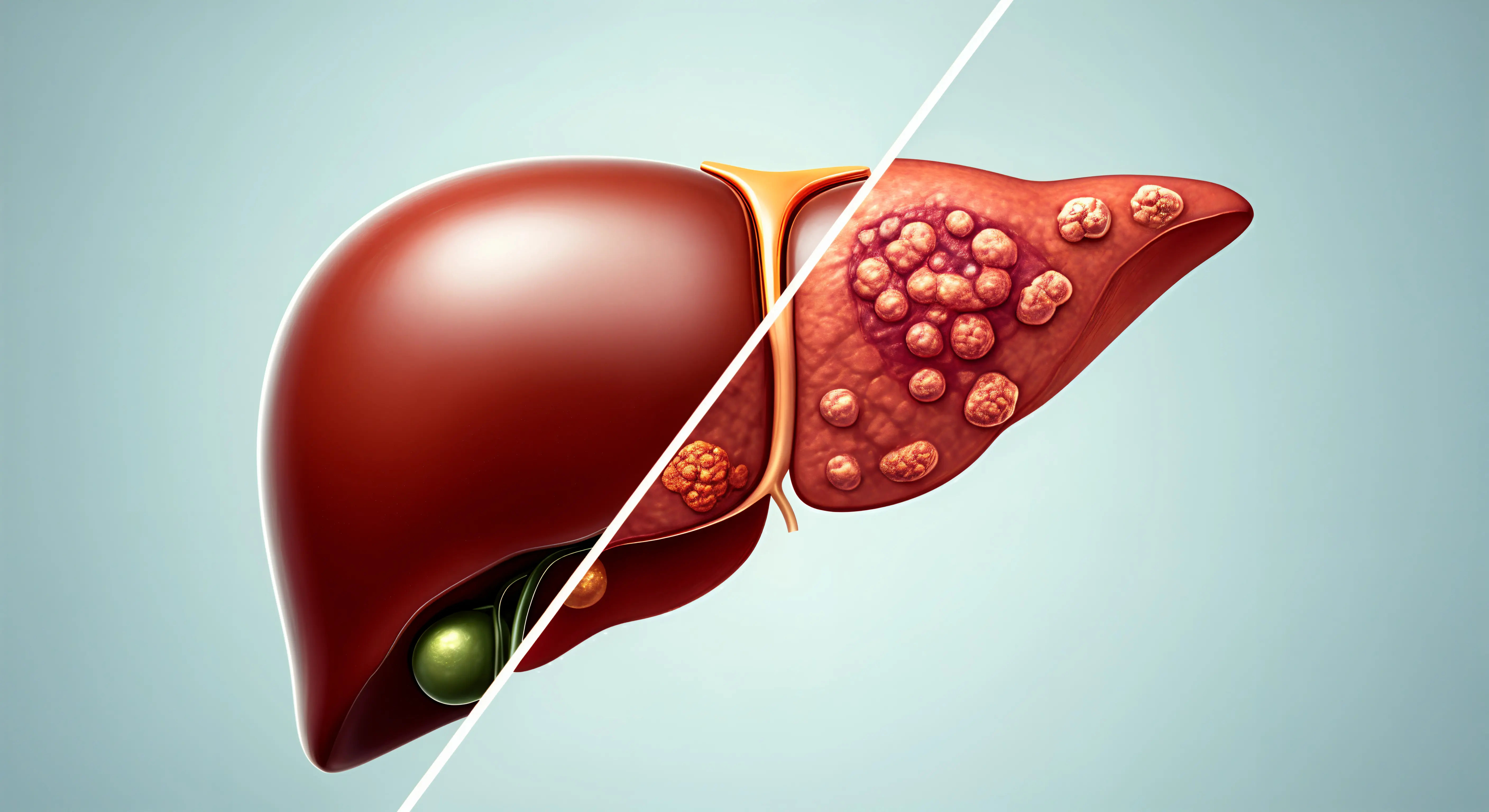
Hepatitis C once meant an almost certain return of the virus after a liver transplant. Today, highly effective direct-acting antivirals (DAAs) have transformed that story. Most people can be cured of hepatitis C before or after a transplant, often with cure rates above 95%. That shift also opened a surprising door: accepting an HCV-positive donor liver to shorten wait time—then using DAAs to prevent or eliminate infection.
In this guide, we explain how a cure is defined, who needs a liver transplant, and when to treat hepatitis C before versus after surgery. We’ll cover the transplant process, risks, recovery, and life after transplant—including medications, diet, and preventing reinfection. You’ll learn about using HCV-positive donor organs safely, what tests you’ll need, and the latest guidance from expert societies. Whether you’re a patient, caregiver, or simply exploring options, this step-by-step resource will help you talk with your team and make informed decisions about hepatitis C and transplant.
Why This Matters Now: Hepatitis C in the DAA Era?
Over the past decade, DAAs have changed hepatitis C from a chronic, often progressive infection into a highly curable condition for most people. Unlike older interferon-based regimens, DAAs are short (usually 8–12 weeks), well-tolerated, and highly effective across genotypes, including in people with cirrhosis. Cure is defined as sustained virologic response (SVR)—an undetectable hepatitis C viral load 12 or 24 weeks after finishing treatment (SVR12/SVR24). Achieving SVR is associated with lower risks of liver failure, liver cancer, and death, and in compensated cirrhosis it may halt or even reverse some scarring.
For transplant candidates, this is crucial. In the interferon era, hepatitis C recurrence after transplant was almost universal and could be aggressive. Now, most candidates can be cured before transplant or soon after, dramatically improving graft survival and quality of life . DAAs also enable safe use of HCV-positive donor livers, reducing wait times and mortality on the list when paired with early antiviral therapy. Unique insight: Cure changes not only outcomes but options—people can choose between pre- or post-transplant treatment based on urgency, liver function, and donor availability, tailoring care rather than following a one-size-fits-all pathway.
Consult a Top General Physician
What Is a Liver Transplant and Who Needs One?
A liver transplant replaces a failing liver with a healthy liver from a deceased or living donor. It’s considered when medical therapy can no longer control complications of end-stage liver disease or in certain liver cancers. Common indications include decompensated cirrhosis (ascites, variceal bleeding, hepatic encephalopathy), acute liver failure, and hepatocellular carcinoma (HCC) that meets transplant criteria.
In most countries, priority on the waitlist is guided by the MELD (Model for End-Stage Liver Disease) score, which estimates the risk of death without transplant using lab values (bilirubin, INR, creatinine, sodium). Higher MELD means higher urgency—and generally faster access to an organ . People with hepatitis C may develop cirrhosis and complications over years. Even after curing the virus, advanced scarring can leave the liver too damaged to recover, making transplant the best option for survival and quality of life. Example: Someone with recurrent fluid buildup despite maximal therapy and a MELD of 20 is usually evaluated urgently. LSI terms to note: liver transplant eligibility MELD score; hepatitis C and liver cancer transplant criteria.
Unique insight: Curing hepatitis C doesn’t always remove the need for transplant if cirrhosis is severe—but it often simplifies post-transplant care and lowers risks.
Can Hepatitis C Be Cured Before Transplant?
Treating hepatitis C before transplant is often preferred if time and liver function permit. DAA therapy can reduce inflammation, decrease complications (like ascites or encephalopathy), and sometimes improve MELD scores . Cure rates typically exceed 95% even in people with compensated cirrhosis. In decompensated cirrhosis, cure rates remain high, though regimen choice and duration may differ, and close monitoring is essential.
Benefits of pre-transplant cure:
- Eliminates risk of post-transplant HCV recurrence.
- Simplifies post-transplant medication management (fewer drug–drug interactions).
- May improve symptoms and quality of life while on the waitlist.
- Can modestly reduce the risk of HCC over time, though surveillance may still be needed in advanced fibrosis
Limitations and the “MELD purgatory” phenomenon:
Some people improve biochemically after DAAs (lower MELD) but still feel unwell, potentially delaying transplant without fully restoring function. Teams balance symptom burden, objective measures, and timing to avoid prolonged suffering.
If someone is very close to receiving an organ (e.g., high MELD), pre-transplant therapy might not fit the timeline.
- Unique insight: The choice isn’t just medical; it’s strategic. If your center offers HCV-positive donor livers with early post-transplant DAA therapy, declining pre-transplant treatment may offer faster access to surgery. This should be a shared decision with full counseling.
Can Hepatitis C Be Cured After Transplant?
Yes. Post-transplant hepatitis C is highly curable with DAAs. Modern regimens achieve cure rates above 95% in liver transplant recipients, including those with prior treatment experience . Many centers begin therapy early after transplant if HCV is present or if an HCV-positive organ was used. The main consideration is managing drug–drug interactions with immunosuppressive medications such as tacrolimus or cyclosporine. Your team will adjust doses and monitor levels during DAA therapy.
Timing:
- Early treatment (within weeks) can prevent the virus from causing damage to the new liver if acquired from the donor.
- If you were already HCV-positive and not treated pre-transplant, therapy is often started once you’re stable post-surgery.
- Unique insight: Early post-transplant DAA therapy isn’t just about cure; it helps protect the new graft from HCV-related injury, potentially reducing biliary complications and fibrosis over time .
- LSI terms: direct-acting antivirals post transplant; hepatitis c recurrence after transplant.
HCV-Positive Donor Livers: A New Opportunity
With DAAs, many centers now offer HCV-positive donor livers to HCV-negative recipients under careful protocols. Why consider this? It can significantly shorten wait time and reduce mortality while waiting, especially in regions with organ scarcity. Strategy: If you accept an HCV-positive organ, your team will typically begin DAA treatment right away or shortly after surgery to prevent or rapidly clear infection. Outcomes with this approach have been excellent in published cohorts and are endorsed by expert guidance in appropriately consented cases
Informed consent should cover:
- The near certainty of transient HCV exposure from the donor.
- The plan for immediate or early DAA therapy and expected high cure rates.
- Rare risks, including resistance or treatment intolerance, and how they would be managed.
- Insurance coverage and access to DAAs.
- Unique insight: Choosing an HCV-positive organ is not “settling.” In many cases, it’s a proactive, data-supported way to get transplanted sooner with excellent long-term outcomes. Long-tail keyword: HCV positive donor to negative recipient.
The Transplant Journey: Step-by-Step
Evaluation
Comprehensive labs (including HCV RNA), imaging (ultrasound, CT/MRI), cardiopulmonary assessment, nutrition and frailty testing, psychosocial evaluation, and cancer screening. You may meet surgeons, hepatologists, infectious disease specialists, social workers, and financial coordinators.
On the list
You’ll have a MELD score and be re-evaluated regularly. Optimize health: vaccinations, smoking cessation, alcohol abstinence, nutrition, and physical therapy to maintain strength. Discuss DAA timing with your team if you have hepatitis C.
The surgery and hospital course
The operation often lasts 6–12 hours. ICU stay is common initially. Most people spend 1–2 weeks in the hospital depending on recovery.
Recovery milestones
Discharge with immunosuppressants; frequent labs to monitor graft function; gradual return to activity. Many resume routine activities within 8–12 weeks, though this varies.
Unique insight: Bring a “transplant binder” with up-to-date medication lists, lab schedules, provider contacts, and symptom logs. It streamlines communication and reduces errors—a small step with big dividends.
Risks, Complications, and How They’re Managed
Common risks include rejection (acute and chronic), infections (especially in the first months due to immunosuppression), and biliary problems (leaks, strictures). Most are manageable with prompt detection and treatment If hepatitis C is present, untreated infection can accelerate graft fibrosis—but DAAs have largely neutralized this risk by enabling early cure .
Reinfection after cure
You can be reinfected if exposed again (e.g., through unsterile injections). Harm-reduction practices and safe healthcare settings are essential. After SVR, your team may periodically recheck HCV RNA if risks are present.
HCC surveillance
If you had HCC or advanced fibrosis before transplant, your team will determine appropriate surveillance post-transplant.
- Unique insight: Immunosuppression changes how infections present—fevers may be muted. Report subtle signs like new fatigue, confusion, abdominal pain, or decreased urine promptly. If your condition does not improve after initial advice, book a physical visit to a doctor with Apollo 24|7. LSI terms: organ transplant risks rejection infection.
Life After Transplant: Medications, Monitoring, and Lifestyle
Medications
Most people take tacrolimus or cyclosporine, plus mycophenolate and/or steroids initially. Blood levels are monitored and doses adjusted. Tell your team about all medications and supplements to avoid interactions.
Lifestyle
- Diet: heart-healthy, high-quality protein, limit salt to control fluid, and food safety to reduce infection risk.
- Exercise: gradual, guided by your team; strength and aerobic activity improve recovery.
- Alcohol: avoid completely to protect the new liver.
Vaccines and screening
Stay current with inactivated vaccines (e.g., influenza, pneumococcal). Live vaccines are generally avoided on immunosuppression. Cancer screening continues as per guidelines.
- Unique insight: Sun protection is more than cosmetic—immunosuppression increases skin cancer risk. Use broad-spectrum sunscreen, protective clothing, and regular skin checks.
Special Situations: Liver Cancer, Pregnancy, and Living Donation
Hepatocellular carcinoma (HCC)
Many with HCV-related HCC qualify for transplant under defined criteria. DAAs do not replace HCC surveillance; your team will coordinate imaging and bridge therapies.
Pregnancy
After successful transplant and stabilized medications, pregnancy is possible with careful planning. Certain DAAs and immunosuppressants are not suitable in pregnancy; discuss timing for HCV cure and conception with your team.
Living donor liver transplant (LDLT)
LDLT can shorten wait time and improve outcomes in experienced centers. Donors undergo rigorous evaluation. For hepatitis C, recipients can be treated pre- or post-LDLT based on urgency. Long-tail keyword: living donor liver transplant for hepatitis c.
Unique insight: For couples planning pregnancy, aim for SVR before conception when feasible and coordinate with hepatology and obstetrics early.
Costs, Insurance, and Access to Care
Drivers of cost
Hospitalization, surgery, ICU care, lifelong immunosuppression, and follow-up. DAA therapy adds cost but is time-limited and often covered due to strong evidence of benefit .
Coverage and assistance
Many insurers approve DAAs for transplant candidates and recipients; patient assistance programs may help with copays. In India and other regions, generic DAAs improve affordability.
Regional perspective
Cost of liver transplant in India varies by center and complexity; discuss detailed estimates and financial counseling early. Apollo 24|7 can help coordinate consultations and follow-up scheduling, and offers home collection for common labs like liver function tests.
- Unique insight: Ask your center to preauthorize DAA therapy before listing or before accepting an HCV-positive organ so there’s no delay when you need it most.
Tests You’ll Need and When to See a Doctor?
Key tests
HCV RNA (to diagnose active infection and confirm SVR), liver function tests (ALT, AST, bilirubin), INR, creatinine, complete blood count, and imaging (ultrasound, CT/MRI) for cancer surveillance or complications. Fibrosis assessment (elastography) may be used pre-transplant .
When to seek care
Call urgently for fever, confusion, severe abdominal pain, jaundice that worsens, uncontrolled vomiting, bleeding, or decreased urine output.
Convenient care
If symptoms persist beyond two weeks, consult a doctor online with Apollo 24|7 for further evaluation. Apollo 24|7 offers a convenient home collection for tests like liver function profiles and HbA1c to monitor metabolic health after transplant.
Unique insight: Keep a copy of your latest lab results on your phone; in emergencies, this speeds decisions and can prevent duplicate testing.
Myths vs Facts About Hepatitis C and Transplant
- Myth: “Hep C always comes back after transplant.”
- Fact: With DAAs, cure rates exceed 95% post-transplant, and recurrence is no longer expected when treated .
- Myth: “You can’t get a transplant if you have Hep C.”
- Fact: People with hepatitis C routinely receive transplants. Many are cured before or after surgery, and some safely accept HCV-positive donor organs with planned antiviral therapy .
- Myth: “DAAs are too risky with immunosuppression.”
- Fact: DAAs are generally safe post-transplant; teams manage drug interactions with routine monitoring.
What the Latest Research and Guidelines Say?
Expert guidelines from hepatology and transplant societies support:
- Treating hepatitis C before transplant when feasible to prevent post-transplant recurrence.
- Treating hepatitis C soon after transplant if not cured pre-surgery.
- Using HCV-positive donor organs with informed consent and prompt DAA therapy, given
- excellent outcomes and the potential to reduce waitlist mortality.
- Emerging data continue to refine optimal timing, regimen selection, and monitoring. Ask your team which protocol your center follows and how they handle drug–drug interactions. LSI terms: hepatitis C cure rate SVR12; antiviral treatment before transplant.
How to Choose a Transplant Center and Prepare?
Questions to ask
- Do you offer HCV-positive donor organs to HCV-negative recipients with immediate DAA therapy?
- What are your outcomes for hepatitis C pre- and post-transplant?
- How do you manage DAA–immunosuppression interactions?
Preparation tips
- Designate a caregiver team; arrange transportation and nearby lodging if needed.
- Build a medication checklist and calendar reminders for labs and clinic visits.
- Discuss nutrition, vaccination status, and exercise plans pre-surgery.
Unique insight: Consider joining a peer support group—patients often share practical strategies for day-to-day recovery that complement medical advice.
Conclusion
In the DAA era, the answer to “Can hepatitis C be cured after a liver transplant?” is a confident yes for most people. Even better, many can be cured before surgery, reducing post-transplant complexity and risk. These therapies also enable innovative pathways—like accepting an HCV-positive donor liver to shorten the wait and then treating right away—without compromising long-term outcomes.
Your best plan depends on timing, liver function, and center protocols. Work with your transplant team to decide whether to treat hepatitis C before or after surgery, how to manage medication interactions, and how to protect your new liver through lifestyle, vaccines, and regular monitoring. Remember: cure is only part of the journey; preparation, support, and follow-up make the difference in day-to-day recovery and quality of life.
If symptoms such as worsening jaundice, abdominal swelling, confusion, or severe fatigue persist beyond two weeks—or if you need help coordinating tests—consult a doctor online with Apollo 24|7. Apollo 24|7 offers a convenient home collection for liver function tests to support your care. With the right strategy and a trusted team, you can navigate transplant and hepatitis C confidently and focus on getting back to life.
Consult a Top General Physician
Consult a Top General Physician

Dr. Imtiyaz Khan
General Physician/ Internal Medicine Specialist
6 Years • MBBS
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru

Dr. Abhishek Gowda
General Physician/ Internal Medicine Specialist
3 Years • MBBS MD General Medicine
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Sajid Samiullah Siraj
General Physician/ Internal Medicine Specialist
2 Years • MBBS
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru

Dr. Karan Goel
General Physician/ Internal Medicine Specialist
11 Years • MBBS, MD (Paediatrics)
Kolkata
Little Steps Clinic, Kolkata
Dr. Sujay P R
General Physician/ Internal Medicine Specialist
3 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru
Consult a Top General Physician

Dr. Imtiyaz Khan
General Physician/ Internal Medicine Specialist
6 Years • MBBS
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru

Dr. Abhishek Gowda
General Physician/ Internal Medicine Specialist
3 Years • MBBS MD General Medicine
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Sajid Samiullah Siraj
General Physician/ Internal Medicine Specialist
2 Years • MBBS
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru

Dr. Karan Goel
General Physician/ Internal Medicine Specialist
11 Years • MBBS, MD (Paediatrics)
Kolkata
Little Steps Clinic, Kolkata
Dr. Sujay P R
General Physician/ Internal Medicine Specialist
3 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru
More articles from Liver disease
Frequently Asked Questions
Can hepatitis C be cured after liver transplant?
Yes. With direct-acting antivirals post transplant, cure rates (SVR12) commonly exceed 95%. Your team will choose a regimen and timing that fit your immunosuppression and recovery.
Should I treat hepatitis C before or after transplant?
It depends on urgency, MELD score, and donor options. Pre-transplant treatment prevents recurrence; post-transplant treatment also achieves high cure rates, especially if you accept an HCV-positive donor liver to shorten wait time.
Will hepatitis C come back after I’m cured?
Cure (SVR) means the virus is cleared. It does not typically “reactivate,” but reinfection can happen with new exposure. Practice harm reduction and safe healthcare to prevent reinfection.
Are there interactions between DAAs and transplant medications?
Some DAAs interact with tacrolimus or cyclosporine. Your team will monitor drug levels and adjust doses. This is routine in post-transplant care.
Can I accept an HCV-positive donor liver if I’m hepatitis C negative?
Yes, in many centers. With informed consent and immediate or early DAA therapy, outcomes are excellent. This approach can reduce time on the waiting list.