Guide to Ovarian Cyst
A comprehensive UK-standard medical guide to ovarian cysts — including causes, symptoms, diagnosis, risks, and treatment options. Learn when to observe, when to seek urgent care, and how management varies across life stages. Includes expert-guided care pathways with Apollo 24|7.

Written by Dr. Siri Nallapu
Reviewed by Dr. J T Hema Pratima MBBS, Fellowship in Diabetes Mellitus
Last updated on 13th Jan, 2026

Introduction
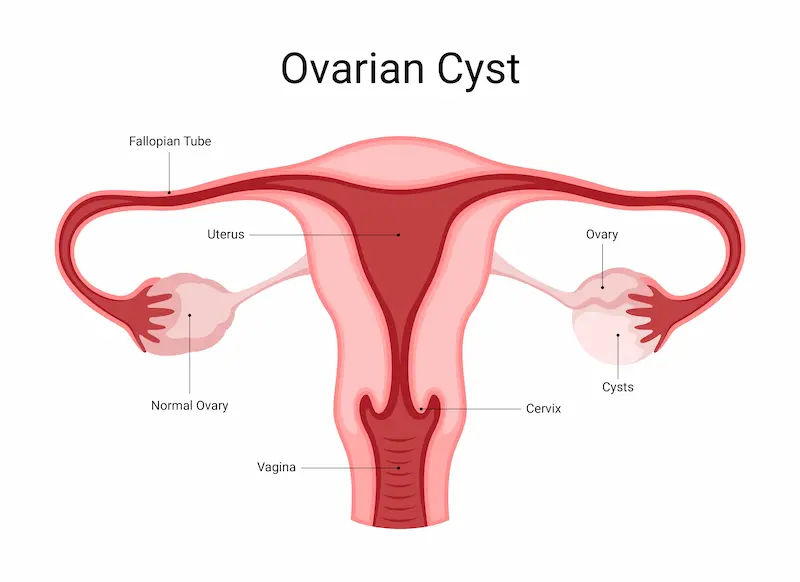
Ovarian cysts are fluid-filled sacs that develop on or within the ovaries. They are extremely common during the reproductive years and, in most cases, are benign and resolve spontaneously. Many individuals never realise they have a cyst until it appears during routine imaging. However, ovarian cysts can also lead to pain, bloating, menstrual irregularities, or complications such as torsion or rupture in some situations. Understanding the type of cyst, its behaviour, and the appropriate management pathway is key to ensuring safe outcomes.
This guide provides a detailed medical overview of ovarian cysts, including their development, categories, clinical presentation, risk indicators, diagnostic methods, and treatment approaches ranging from conservative monitoring to surgical intervention. It also addresses special circumstances, including pregnancy and postmenopause and offers medical insights on prevention limits and long-term management. For personalised recommendations or guidance when symptoms persist, individuals can seek gynaecological care through Apollo 24|7.
Consult a Top Gynaecologist for Personalised Advice
What Is an Ovarian Cyst?
Ovarian cysts commonly arise as part of the normal ovarian cycle and are often temporary.
Ovarian cysts most frequently result from normal follicular activity. Every month, a follicle matures in preparation for
ovulation. If this process continues beyond egg release or does not proceed normally, fluid accumulation may occur,
forming a functional cyst. These cysts usually disappear within one to three menstrual cycles and rarely require
intervention.
Normal Ovarian Function and Cyst Formation
During the follicular phase, ovarian follicles enlarge under hormonal stimulation. At ovulation, one follicle releases an
oocyte. The residual structure forms the corpus luteum, secreting progesterone. If the corpus luteum persists beyond its
expected duration, it may retain fluid or blood and become cystic. These physiological cysts are a result of standard
reproductive processes and are typically self-limiting.
Simple vs Complex Cysts
A simple cyst is thin-walled and contains clear fluid. These are commonly benign.
A complex cyst may contain blood, septations, or solid areas. Such findings are not synonymous with malignancy;
benign entities such as endometriomas or dermoids may show complexity. Ultrasound features, patient age, symptoms,
and menopausal status collectively determine clinical relevance.
Prevalence
Simple cysts are frequent among those who menstruate and often go unnoticed. In premenopausal individuals, cysts up to
3–5 cm are usually considered physiological. In postmenopause, cysts require more careful evaluation due to altered risk
patterns, though small simple cysts may still be monitored safely.
Clinical Insight: The clinical management approach depends not solely on cyst size, but also on imaging appearance,
symptom severity, and reproductive stage.
Types of Ovarian Cysts
Accurate classification assists in predicting progression and treatment requirements.
Functional Cysts
Functional cysts arise from normal ovulation and include:
- Follicular cysts — typically thin-walled, fluid-filled.
- Corpus luteum cysts — thicker-walled, may contain blood and cause acute pain.
These cysts usually resolve without treatment. Monitoring with follow-up ultrasound is common.
Benign Non-Functional Cysts
- Dermoid cysts (mature cystic teratomas): Derived from germ cells; may contain fat or hair. Although benign, their
potential for torsion increases with growth, often warranting removal if large or symptomatic. - Cystadenomas: Can be serous or mucinous and may grow substantially. Surgical management is frequently indicated to prevent complications.
Endometriomas
Endometriosis-related cysts, containing old blood, are known as endometriomas. They are associated with chronic pelvic
pain and may impair fertility. Management includes symptom control, surgical removal if necessary, and long-term
monitoring due to recurrence risk.
PCOS vs a Single Cyst
Polycystic ovary syndrome is a hormonal disorder characterised by multiple small follicles, menstrual irregularities, and
hyperandrogenic symptoms. It is distinct from a singular ovarian cyst and requires a different management pathway.
Clinical Insight: “Complex” is a descriptive imaging term — not a diagnosis. Many complex cysts remain benign.
Symptoms and When to Worry
Symptoms vary widely and may overlap with other pelvic conditions.
Common Symptoms
Some individuals remain asymptomatic. When symptoms occur, they may include:
- Unilateral pelvic pain (dull or sharp)
- Abdominal bloating or pressure sensation
- Menstrual irregularities
- Dyspareunia or pain during bowel movements
- Urinary frequency due to mass effect
These symptoms warrant assessment, especially if persistent. If discomfort continues for more than two weeks, online consultation with an Apollo 24|7 gynaecologist may support early diagnostic decisions.
Emergency Symptoms: Torsion or Rupture
Urgent evaluation is required in cases of:
- Suddenly, severe unilateral pelvic pain
- Nausea or vomiting accompanying pain
- Fever or fainting
- Rapid breathing or dizziness
- Pain onset following vigorous physical activity
These signs may indicate torsion, compromising ovarian blood supply, or cyst rupture with internal bleeding.
When to Contact a Clinician
Persistent or worsening pelvic symptoms, significant bloating, or abnormal menstrual patterns indicate the need for
review. Apollo 24|7 offers a timely medical assessment to determine whether imaging or an in-person examination is
required.
Clinical Insight: Symptom tracking aligned with the menstrual cycle aids differential diagnosis.
Causes and Risk Factors
Risk varies depending on hormonal activity, medical history, and reproductive stage.
Hormonal and Ovulatory Drivers
Regular ovulation increases the likelihood of functional cyst formation. Combined hormonal contraception may reduce
recurrence risk by preventing ovulation but does not shrink pre-existing cysts.
Pregnancy, Fertility Treatment, Past Cysts
Early pregnancy may involve corpus luteum cysts that resolve naturally. Ovulation-inducing medications may increase
functional cyst formation. A history of cysts slightly increases recurrence probability.
Endometriosis and Pelvic Infection
Endometriosis commonly forms ovarian cysts. Severe pelvic infections may produce tubo-ovarian abscesses — clinically
distinct and requiring urgent antibiotic therapy.
Age and Menopause
Cyst incidence decreases following menopause. However, any new postmenopausal ovarian mass warrants structured
evaluation due to variation in malignant potential. Appropriate surveillance is required.
Clinical Insight: Timing of imaging matters — a repeat scan after 6–12 weeks may clarify transient post-ovulatory
changes.
Diagnosis: Tests and Imaging
Accurate assessment combines clinical history, examination, and imaging.
Initial Assessment
Investigations typically include:
- Pelvic examination
- Pregnancy testing when applicable
- Pelvic ultrasound as the primary diagnostic tool
Apollo 24|7 enables scheduling for imaging and laboratory tests where service availability supports efficient workflow.
Doppler and MRI
Doppler ultrasound assesses ovarian blood flow when torsion is suspected. MRI provides additional anatomical detail
where ultrasound is indeterminate.
CA-125 Testing
CA-125 may be used selectively, especially in postmenopausal individuals or when imaging indicates suspicious features.
Elevated values can arise from benign conditions, so interpretation must be contextual.
Follow-Up and Monitoring
Most small, simple, asymptomatic cysts are monitored with interval ultrasounds. Persistence, growth, or atypical features may prompt referral for surgical evaluation.
Clinical Insight: Reviewing previous imaging can reduce unnecessary interventions by demonstrating cyst stability.
Treatment Options: From Monitoring to Surgery
Management is tailored to symptoms, imaging characteristics, and reproductive considerations.
Conservative Measures
Pain control may include:
- Non-steroidal anti-inflammatory medicines where clinically suitable
- Local heat therapy
- Guided physical activity adjustments
- Constipation management
If pain limits daily mobility, consultation with an Apollo 24|7 clinician may support pain planning and follow-up recommendations.
Hormonal Therapy
Combined hormonal contraception may reduce the recurrence of functional cysts by suppressing ovulation, helping
individuals who develop cysts frequently.
Surgical Management
Indications for surgery include:
- Large cysts (>5–7 cm)
- Persistent symptomatic cysts
- Suspicious or complex imaging features
- Concern for torsion or rupture
Laparoscopy is preferred for benign cysts to preserve ovarian tissue, particularly where future fertility is a priority. Laparotomy may be necessary for large or suspicious masses.
Informed Decision-Making
Patients are encouraged to clarify:
- Cyst type
- Risk profile
- Treatment timeline
- Fertility impact
- Appropriate follow-up schedule
Apollo 24|7 specialists can guide decisions based on clinical need and patient goals.
Clinical Insight: Management thresholds differ between reproductive stages — similar imaging features may lead to
different approaches depending on age and menopause status.
Special Situations
Certain life stages alter risk patterns and management.
Pregnancy
Most pregnancy-associated cysts resolve spontaneously. Conservative care is typical unless complications arise. Surgical
intervention, if needed, is generally safest during the second trimester.
Adolescents and Young Adults
Functional cysts dominate in this group. Avoiding unnecessary ovarian surgery protects future fertility. Monitoring and
education are key components of care.
Perimenopause and Postmenopause
New ovarian masses in this group require more rigorous assessment. Surveillance approaches balance early detection
with avoidance of unwarranted surgery.
Clinical Insight: Establishing a clear escalation plan supports prompt action if symptoms evolve.
Complications, Outlook, and Prevention
Most cysts resolve completely, but potential complications require vigilance.
Possible Complications
- Ovarian torsion — more common in larger cysts
- Rupture — may result in acute pain and internal bleeding
- Rare malignancy risk — increases with age and suspicious features
Recurrence and Long-Term Prognosis
Functional cyst recurrence is common in ovulating individuals. Contraceptive strategies may reduce recurrence in
suitable candidates. After removal of benign cysts, recurrence may occur in either ovary. Symptom awareness aids early
detection.
Prevention Limits
While ovulation-suppressing contraception can reduce functional cyst formation, benign cysts from other causes cannot
be fully prevented. Monitoring and timely assessment remain crucial.
If ongoing pelvic pain or cycle changes persist, Apollo 24|7 provides access to medical consultations to determine next
steps.
Clinical Insight: Self-monitoring of symptoms enhances continuity of care.
Conclusion
The majority of ovarian cysts are benign and transient. Understanding cyst type, clinical implications, and appropriate
diagnostic pathways allows individuals to navigate management confidently. Many cysts resolve without intervention, and simple observation with structured follow-up is a safe and common approach. Where treatment is necessary — whether hormonal therapies or minimally invasive surgery — modern options support both safety and fertility.
Clear communication with a clinician helps ensure that decisions reflect personal health priorities and risk profiles. Symptom diaries, knowledge of warning signs, and regular follow-up imaging support safer outcomes. If persistent pain, bloating, or menstrual irregularities continue beyond several weeks — or if severe, sudden symptoms occur — timely medical advice is essential.
For further evaluation, ongoing monitoring, or expert gynaecological care, support is accessible through Apollo 24|7, including virtual consultations, diagnostic bookings, and care coordination where available. With credible medical guidance, most individuals recover fully and return to daily life without long-term consequences.
Consult a Top Gynaecologist for Personalised Advice
Consult a Top Gynaecologist for Personalised Advice

Dr. Sreeparna Roy
Obstetrician and Gynaecologist
8 Years • MBBS , MS (OBSTETRICS & GYNAECOLOGY), Fellowship in Infertility, Endoscopy & Ultrasonography), Fellowship in Laparoscopy & Hysteroscopy,DRM
Kolkata
Dr Utsa Basu Clinic, Kolkata

Dr. Revathi S Rajan
Obstetrician and Gynaecologist
24 Years • MBBS, DGO, DNB.FFMM
Bengaluru
Apollo Clinic, JP nagar, Bengaluru
Dr. Navin Srinivasan
Gynaecological Oncologist
9 Years • MBBS, MS DNB(OBS-GYNAE), MCH (GYNAE ONCOLOGY)
Bengaluru
Apollo Clinic Mahadevapura, Bengaluru

Dr. Prashant Chandra Das
Surgical Oncologist
15 Years • MBBS (MKCG Medical college) MCh (Surgical Oncology, Kidwai memorial institute of Oncology, Bangalore) MS (General Surgery, BHU Varanasi) Fellowship in Minimal Access Surgery ( FMAS). ESSO Course On Minimally Invasive Esophagectomy & Gastrectomy (UMC, Utrecht, Netherlands). Trained in Robotic and Laparoscopic Cancer Surgery.
Bhubaneswar
Apollo Hospitals Old Sainik School Road, Bhubaneswar
(25+ Patients)

Dr. Swati Shah
Surgical Oncologist
15 Years • DNB Surgical Oncology, certified Robotic Cancer Surgeon
Ahmedabad
Apollo Hospitals Gandhinagar, Ahmedabad
(25+ Patients)
Consult a Top Gynaecologist for Personalised Advice

Dr. Sreeparna Roy
Obstetrician and Gynaecologist
8 Years • MBBS , MS (OBSTETRICS & GYNAECOLOGY), Fellowship in Infertility, Endoscopy & Ultrasonography), Fellowship in Laparoscopy & Hysteroscopy,DRM
Kolkata
Dr Utsa Basu Clinic, Kolkata

Dr. Revathi S Rajan
Obstetrician and Gynaecologist
24 Years • MBBS, DGO, DNB.FFMM
Bengaluru
Apollo Clinic, JP nagar, Bengaluru
Dr. Navin Srinivasan
Gynaecological Oncologist
9 Years • MBBS, MS DNB(OBS-GYNAE), MCH (GYNAE ONCOLOGY)
Bengaluru
Apollo Clinic Mahadevapura, Bengaluru

Dr. Prashant Chandra Das
Surgical Oncologist
15 Years • MBBS (MKCG Medical college) MCh (Surgical Oncology, Kidwai memorial institute of Oncology, Bangalore) MS (General Surgery, BHU Varanasi) Fellowship in Minimal Access Surgery ( FMAS). ESSO Course On Minimally Invasive Esophagectomy & Gastrectomy (UMC, Utrecht, Netherlands). Trained in Robotic and Laparoscopic Cancer Surgery.
Bhubaneswar
Apollo Hospitals Old Sainik School Road, Bhubaneswar
(25+ Patients)

Dr. Swati Shah
Surgical Oncologist
15 Years • DNB Surgical Oncology, certified Robotic Cancer Surgeon
Ahmedabad
Apollo Hospitals Gandhinagar, Ahmedabad
(25+ Patients)
More articles from Ovarian cysts
Frequently Asked Questions
1) How long do functional ovarian cysts take to resolve?
Most resolve within one to three cycles. A follow-up ultrasound is commonly advised to ensure resolution.
2) Can contraception prevent ovarian cysts?
Combined hormonal contraception may reduce the formation of new functional cysts; it does not shrink existing ones.
3) What does a complex cyst indicate?
Complex features reflect internal structure on imaging but do not necessarily imply cancer. Combined assessment determines risk.
4) When should I worry about pelvic pain?
sudden severe unilateral pain, fainting, fever, or vomiting requires urgent attention. Persistent symptoms also require medical review.
5) Is CA-125 testing always needed?
CA-125 is used selectively based on menopause status and imaging findings. It must be interpreted in context.