PCOS Understanding the Most Common Hormonal Disorder
Learn about PCOS, its causes, symptoms, and effective management strategies, including lifestyle changes, medical treatments, and emotional support for better reproductive and metabolic health.

Introduction
Have you been struggling with unpredictable periods, unexplained weight gain, or skin issues that just won’t clear up? You are not alone. These could be signs of polycystic ovarian syndrome (PCOS), the commonest hormonal disorder affecting people with ovaries during their reproductive years. Affecting an estimated 1 in 10 women globally, PCOS is far more than just a reproductive issue; it's a complex metabolic disorder that impacts the entire body. Despite its prevalence, it often goes undiagnosed or misunderstood, leaving many to navigate its challenging symptoms without support. This guide is designed to demystify PCOS, offering a clear, comprehensive look at its causes, symptoms, and most importantly, the effective management strategies that can help you reclaim your health. Whether you're newly diagnosed or seeking to understand it better, we will walk you through everything you need to know about living well with this condition.
What Exactly is PCOS?
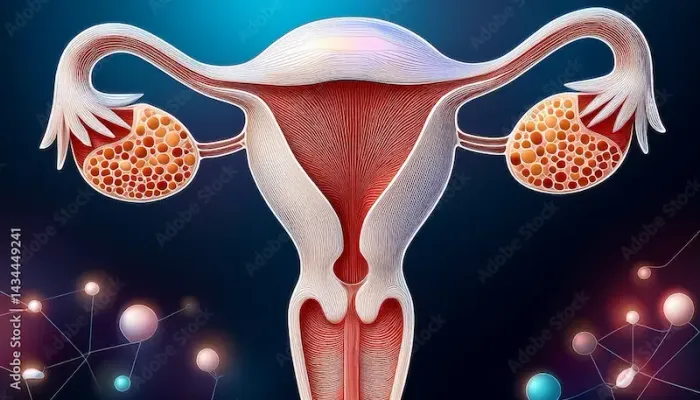
Polycystic ovarian syndrome (PCOS) is a condition characterised by a hormonal imbalance that interferes with the normal function of the ovaries. The name itself can be misleading. "Polycystic" means "many cysts," but the cysts are actually immature follicles (sacs that contain eggs) that have not been released due to the hormonal disruption. Instead of maturing and being released during ovulation, these follicles accumulate on the ovary's surface.
Beyond Ovarian Cysts: A Systemic Metabolic Condition
It's crucial to understand that PCOS is not solely an ovarian disorder. It is a systemic condition, meaning it affects the entire body. The root of the problem lies in the endocrine system, which produces hormones. In PCOS, the body often produces higher-than-normal levels of androgens (often called "male hormones," though everyone has them), which disrupts the menstrual cycle. Furthermore, many individuals with PCOS have insulin resistance, a key metabolic issue where the body's cells don't respond effectively to insulin, leading to high insulin levels in the blood. This hyperinsulinemia is a major driver of both the symptoms and long-term health risks of PCOS.
The Hormonal Imbalance at the Core of PCOS
The primary hormonal players in PCOS are:
1. Androgens (like Testosterone): Elevated levels prevent ovulation and cause symptoms like hirsutism (excessive hair growth) and acne.
2. Insulin: High insulin levels stimulate the ovaries to produce more androgens, creating a vicious cycle.
3. Luteinising Hormone (LH): Often disproportionately high compared to follicle-stimulating hormone (FSH), further impairing follicle development.
Consult a Gynaecologist for the best advice
Recognising the Signs: Common PCOS Symptoms
The symptoms of PCOS can vary widely from person to person, both in type and severity. This variability is one reason why diagnosis can be delayed.
Physical Symptoms You Can See
Here are some of the physical symptoms of PCOS that you may notice:
• Irregular Periods: This is a hallmark sign. Periods may be infrequent (fewer than nine per year), very heavy, or absent altogether.
• Hirsutism: Excess facial and body hair, particularly on the chin, upper lip, chest, and abdomen.
• Acne and Oily Skin: Persistent acne, often along the jawline, that doesn't respond well to typical treatments.
• Hair Thinning (Alopecia): Thinning hair on the scalp, similar to male-pattern baldness.
• Weight Gain and Difficulty Losing Weight: A common struggle, especially around the abdomen, largely driven by insulin resistance.
• Acanthosis Nigricans: Dark, velvety patches of skin in body folds like the neck, groin, and underarms.
Internal Symptoms You Might Feel
PCOS can also affect your body internally, leading to symptoms you might feel rather than see:
• Fertility Challenges: Due to irregular or absent ovulation, PCOS is a leading cause of infertility.
• Mental Health Impact: The physical symptoms and hormonal fluctuations can contribute to anxiety, depression, and poor self-esteem.
• Sleep Problems: Conditions like sleep apnoea are more common in people with PCOS.
What Causes PCOS? Unraveling the Mystery
While the exact cause remains unknown, research points to a combination of genetic and lifestyle factors.
The Role of Insulin Resistance
This is a central player. When cells become resistant to insulin, the pancreas produces even more insulin to compensate. High insulin levels, in turn, increase androgen production from the ovaries and adrenal glands, worsening the core symptoms of PCOS. This link is why managing insulin levels is a cornerstone of PCOS treatment.
Genetic and Environmental Factors
PCOS often runs in families, suggesting a strong genetic component. If your mother or sister has PCOS, your risk is higher. Environmental factors, such as a sedentary lifestyle and a diet high in processed foods and sugars, can exacerbate insulin resistance, triggering or worsening the condition in genetically predisposed individuals.
How is PCOS Diagnosed?
There is no single test for PCOS. Diagnosis is based on a combination of your medical history, a physical exam, blood tests, and sometimes an ultrasound. If you suspect you have PCOS, it's important to consult a gynaecologist or endocrinologist. Platforms like Apollo24|7 can connect you with specialists for an initial online consultation to discuss your symptoms.
The Rotterdam Criteria: The Gold Standard
Most experts use the Rotterdam Criteria. A diagnosis of PCOS is made if you have at least two of the following three features:
1. Irregular or absent ovulation: Manifesting as irregular or absent periods.
2. Hyperandrogenism: Clinical signs (like hirsutism or acne) or biochemical signs (high androgen levels on a blood test).
3. Polycystic ovaries on ultrasound: The presence of 12 or more follicles in one or both ovaries.
#### H3: Essential Tests and Assessments
Your doctor will likely recommend:
• Blood Tests: To check hormone levels (androgens, LH, FSH, thyroid), cholesterol, and glucose tolerance. For convenient testing, Apollo24|7 offers home collection for essential tests like HbA1c and thyroid panels, saving you a trip to the lab.
• Pelvic Ultrasound: To examine the appearance of your ovaries and the thickness of the uterine lining.
Get Your Health Assessed
Long-Term Health Risks Associated with PCOS
Managing PCOS is not just about addressing current symptoms; it's about preventing future complications. Unmanaged PCOS increases the risk of:
1. Type 2 Diabetes: Due to insulin resistance.
2. Cardiovascular Disease: High cholesterol and blood pressure are more common.
3. Endometrial Hyperplasia: The uterine lining can build up due to infrequent periods, increasing the risk of endometrial cancer.
4. Sleep Apnoea and Fatty Liver Disease.
Managing PCOS: A Multi-Faceted Approach
While there is no cure for PCOS, its symptoms can be effectively managed. Treatment is highly personalised based on your symptoms and whether you're trying to conceive.
Foundation of Management: Diet and Exercise
Lifestyle modification is the first-line treatment.
• Diet: A balanced diet focused on whole foods, high fibre, lean protein, and healthy fats helps manage insulin resistance. Reducing sugar and refined carbohydrates is critical.
• Exercise: A combination of aerobic exercise (like brisk walking) and strength training improves insulin sensitivity and aids weight management.
Medications to Manage Symptoms and Underlying Issues
Regulating Menstrual Cycles and Reducing Androgens
Several treatments can help regulate menstrual cycles and manage androgen-related symptoms in PCOS:
• Combined Oral Contraceptives (Birth Control Pills): Often prescribed to regulate periods and reduce androgen levels, improving acne and hirsutism.
• Metformin: A diabetes medication that improves insulin sensitivity, which can help with ovulation, weight loss, and regulating cycles.
• Anti-androgen medications: Can be used to treat hirsutism and hair loss.
Addressing Fertility Goals
If pregnancy is a goal, treatments may include:
• Ovulation Induction: Medications like clomiphene or letrozole are used to stimulate ovulation.
• In Vitro Fertilisation (IVF): May be considered if other treatments are not successful.
Living Well with PCOS: Beyond Medication
The Importance of Mental and Emotional Health
The emotional toll of PCOS is significant. Seeking support from a therapist, joining a support group, or practicing stress-reduction techniques like yoga and mindfulness can be incredibly beneficial. Remember, your mental well-being is just as important as your physical health.
Conclusion
Living with polycystic ovarian syndrome can feel overwhelming, but it's important to remember that it is a manageable condition. By understanding the root causes—particularly the role of insulin resistance—you can take empowered steps toward better health. A combination of a healthy lifestyle, appropriate medical interventions, and strong emotional support can help you effectively control your symptoms and significantly reduce your risk of long-term complications. You are the most important advocate for your own health. If this article resonates with your experiences, don't hesitate to seek professional help. A clear diagnosis and a tailored management plan can make a world of difference, allowing you to live a full and healthy life with PCOS. If your symptoms persist or cause you concern, booking a physical visit to a gynaecologist with Apollo24|7 can provide you with a comprehensive evaluation and a clear path forward.
Consult a Gynaecologist for the best advice
Consult a Gynaecologist for the best advice

Dr. Parul Sharma
Obstetrician and Gynaecologist
8 Years • MBBS, MS (Obstetrics & Gynaecology)
New Delhi
THE DOCTORS NESST, New Delhi

Dr. Debajyoti Goswami
Obstetrician and Gynaecologist
10 Years • MBBS,D.G.O(DNB),Adv. Infertility Tech.(AIIMS),Fellowship in Diabetes(U.K),Comprehensive Abortion Care(Govt. Of W.B), Certificate in Clinical Embryology(AIIMS, BHUBANESWAR)
Bankura
D.G Clinic, Bankura
(25+ Patients)
Dr. K Anusha
Obstetrician and Gynaecologist
4 Years • MBBS, DGO
Yemmiganur
SRINIVASAA HOSPITAL, Yemmiganur

Dr. Asha Rani Singh
Obstetrician and Gynaecologist
24 Years • MBBS DGO
Delhi
Dr Asha Rani Singh Clinic, Delhi

Dr. Sheetal Aggarwal
Obstetrician and Gynaecologist
17 Years • MBBS, MS (Obstetrics & Gynaecology)
Gurugram
Dr Sheetal's clinic, Gurugram
Consult a Gynaecologist for the best advice

Dr. Parul Sharma
Obstetrician and Gynaecologist
8 Years • MBBS, MS (Obstetrics & Gynaecology)
New Delhi
THE DOCTORS NESST, New Delhi

Dr. Debajyoti Goswami
Obstetrician and Gynaecologist
10 Years • MBBS,D.G.O(DNB),Adv. Infertility Tech.(AIIMS),Fellowship in Diabetes(U.K),Comprehensive Abortion Care(Govt. Of W.B), Certificate in Clinical Embryology(AIIMS, BHUBANESWAR)
Bankura
D.G Clinic, Bankura
(25+ Patients)
Dr. K Anusha
Obstetrician and Gynaecologist
4 Years • MBBS, DGO
Yemmiganur
SRINIVASAA HOSPITAL, Yemmiganur

Dr. Asha Rani Singh
Obstetrician and Gynaecologist
24 Years • MBBS DGO
Delhi
Dr Asha Rani Singh Clinic, Delhi

Dr. Sheetal Aggarwal
Obstetrician and Gynaecologist
17 Years • MBBS, MS (Obstetrics & Gynaecology)
Gurugram
Dr Sheetal's clinic, Gurugram
More articles from Pcod Pcos Treatment
Frequently Asked Questions
1. What is the difference between PCOD and PCOS?
While often used interchangeably, some experts distinguish them. PCOD (polycystic ovarian disease) is often considered a milder condition where ovaries produce immature eggs, while PCOS is a more severe metabolic endocrine disorder. However, in most current medical practice, PCOS is the standard term used for diagnosis.
2. Can you get pregnant if you have PCOS?
Yes, absolutely. While PCOS is a common cause of infertility due to irregular ovulation, many women with PCOS can and do get pregnant. With appropriate treatment, such as lifestyle changes and ovulation induction medications, pregnancy is very achievable.
3. What is the best diet for managing PCOS symptoms?
There's no one-size-fits-all diet, but a low-glycemic index (GI) diet is generally recommended. This focuses on whole foods like vegetables, whole grains, lean proteins, and healthy fats to help manage insulin resistance and support weight loss.
4. Does PCOS mean I have cysts on my ovaries?
Not necessarily. The 'cysts' are actually immature follicles, and you can be diagnosed with PCOS without having them on an ultrasound if you meet the other two criteria (irregular periods and high androgens).
5. Can PCOS be cured?
There is currently no cure for PCOS. However, its symptoms can be effectively managed through lifestyle interventions and medication. The goal of treatment is to manage symptoms and prevent long-term health complications.






