What Leads To Signs Of Piriformis Syndrome Treatment
Know about the piriformis syndrome, what it is, signs, symptoms, causes, diagnosis, treatment options and misconceptions of the piriformis syndrome.

Written by Dr. Siri Nallapu
Reviewed by Dr. Shaik Abdul Kalam MD (Physician)
Last updated on 13th Jan, 2026

Introduction
If you’ve ever felt a deep, nagging ache in your buttock that gets worse when you sit, climb stairs, or drive—sometimes with tingling or pain down the back of your leg—you might wonder if it’s sciatica or something else. Piriformis syndrome is a common, under-recognised cause of “sciatica-like” pain, where a small hip muscle (the piriformis) irritates the nearby sciatic nerve. In this guide, we’ll unpack what leads to the signs of piriformis syndrome, how to recognise it, and what truly works for treatment. You’ll learn the difference between piriformis syndrome and other causes of sciatica, get a step-by-step plan for relief, and see how to prevent flare-ups long term. Whether you’re a desk worker, runner, parent, or weekend warrior, you’ll find practical, evidence-informed strategies you can start today and clear advice on when to seek medical help, including convenient telehealth options if symptoms persist.
Piriformis Syndrome: What It Is and Why It Hurts
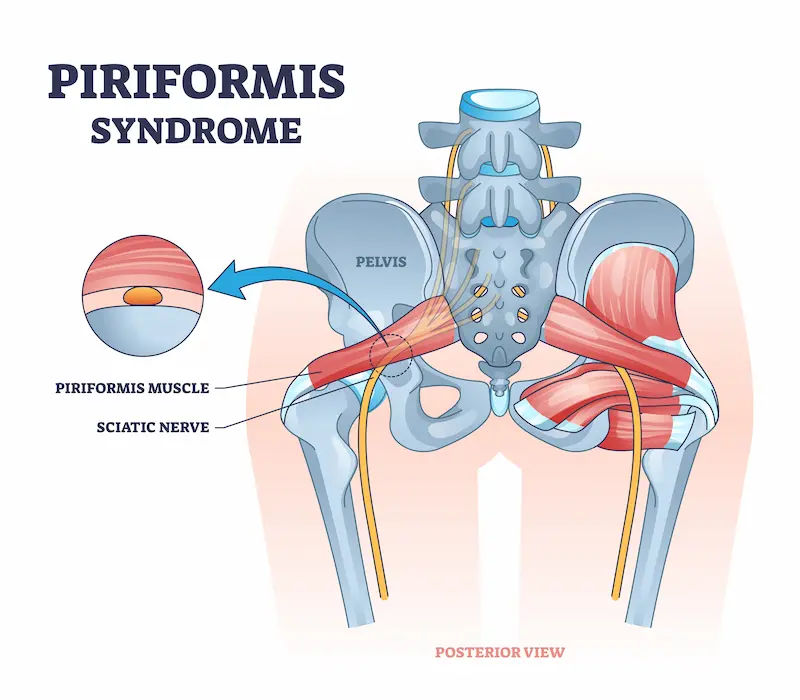
Piriformis syndrome is a neuromuscular condition where the piriformis muscle in the buttock compresses or irritates the sciatic nerve, producing buttock pain that can radiate down the back of the thigh, sometimes to the calf or foot. Unlike “true sciatica” caused by a lumbar disc herniation or spinal stenosis, the problem here sits outside the spine within the deep gluteal space. Hence, positions that stretch or compress the piriformis (like long sitting or crossing legs) often aggravate symptoms.
A quick tour of the piriformis muscle: The piriformis is a small, pear-shaped muscle that runs from your sacrum to the top of your thigh bone (greater trochanter). It helps rotate the hip and stabilise the pelvis during walking and running.
Consult Top General Practitioner for Personalised Advice
How can the piriformis irritate the sciatic nerve?
The sciatic nerve typically passes beneath the piriformis. Tightness, spasm, hypertrophy, or inflammation of the piriformis can reduce space or increase friction on the nerve, leading to pain and neurologic-like symptoms such as tingling or numbness down the leg.
Piriformis syndrome vs. “true” sciatica
Both can feel similar, but spinal sciatica often worsens with coughing/sneezing and prolonged forward flexion, and may show changes on lumbar MRI. Piriformis syndrome typically provokes pain with sitting, external rotation, or direct pressure over the deep gluteal area. Many clinicians also use the umbrella term “deep gluteal syndrome” when non-piriformis structures contribute.
What Leads to the Signs and Symptoms? Root Causes and Triggers
Piriformis syndrome signs arise from a mix of mechanical irritation and nerve sensitivity. Key contributors include:
Overuse, prolonged sitting, and muscle imbalances: Long sitting (especially on a soft couch or with a thick wallet in the back pocket), hill running, and sudden increases in training volume can overwork the piriformis or surrounding hip rotators. Weak gluteus medius and deep hip stabilisers force the piriformis to “pick up the slack,” increasing strain. Over time, this leads to tightness, spasm, and pressure on the sciatic nerve.
Biomechanics: hip stability, foot posture, and gait: Poor single-leg stability, excessive hip internal rotation when running, and overpronation can make the piriformis work overtime to control the femur. Addressing mechanics with targeted strengthening and gait cues often reduces recurrence.
Anatomical variants: In a minority of people, the sciatic nerve passes through or above parts of the piriformis, increasing the chance of nerve irritation when the muscle tightens. These variants help explain why some individuals develop piriformis syndrome with minimal load, while others tolerate high volumes of activity.
Secondary causes: Direct buttock trauma (falls), hip surgery, pregnancy (hormonal laxity plus altered posture), or local oedema can narrow the deep gluteal space and sensitise the nerve.
Unique insight: The same “dose” of sitting or running doesn’t affect everyone equally. Your unique anatomy and movement patterns determine your threshold—so the fix must be personalised.
Recognising the Signs of Piriformis Syndrome
Typical symptoms:
- Deep buttock pain (often one-sided), sometimes sharp or burning
- Worse with sitting (especially >20–30 minutes), climbing stairs, getting out of a car, or crossing legs
- Tenderness over the deep gluteal area
- Pain or tingling down the back of the thigh (sometimes to the calf/foot)
- Relief with standing or lying on the opposite side
How Clinicians Diagnose Piriformis Syndrome
There’s no single test that “proves” piriformis syndrome. Diagnosis combines history, exam, and ruling out other causes.
History and physical: Clinicians look for buttock-predominant pain aggravated by sitting, tenderness over the piriformis, and reproduction of symptoms with specific manoeuvres:
- FAIR test (Flexion, Adduction, Internal Rotation): compresses the piriformis against the nerve
- Freiberg sign (forced internal rotation)
- Pace test (resisted abduction and external rotation)
- Positive tests support the diagnosis but are not definitive.
Imaging and EMG: MRI of the lumbar spine may be ordered to exclude disc herniation or stenosis if symptoms or signs suggest a spinal source. Pelvic MRI or ultrasound can sometimes visualise piriformis hypertrophy or inflammation; diagnostic ultrasound can also guide injections. EMG may help differentiate peripheral nerve compression from radiculopathy in complex cases.
Differential diagnosis:
- Lumbar radiculopathy (L4-S1)
- Hamstring tendinopathy
- Greater trochanteric pain syndrome
- Sacroiliac joint dysfunction
- Ischiofemoral impingement, Deep gluteal syndrome from other structures (e.g., obturator internus)
A careful exam helps target the true driver.
Evidence-Based Treatment Options (From Simple to Specialised)
Most cases of piriformis syndrome improve without injections or surgery. A stepped approach reduces pain while addressing root causes.
Self-care first: activity modification, heat/ice, pacing
- Reduce prolonged sitting; stand and move every 20–30 minutes
- Avoid long strides, steep hills, and deep hip stretches initially
- Use heat to relax muscles before gentle movement; ice after activity if inflamed
- Gentle walking can reduce nerve sensitivity and improve circulation
These strategies are first-line in many clinical guides.
Physical therapy essentials: stretching, strengthening, nerve glides
- Stretching: gentle figure-4 stretch, supine knee-to-opposite-shoulder stretch, and pigeon pose modifications for 20–30 seconds, 2–3 times/day
- Strengthening: gluteus medius/minimus, deep rotators, and core (side planks, clamshells, hip abduction, bridging progressions)
- Nerve gliding exercises (“nerve flossing”) for the sciatic nerve to reduce irritability without aggressive tension
ChoosePT emphasizes a progressive plan balancing mobility with stability to avoid re-irritation (APTA/ChoosePT). - Medications: Short courses of NSAIDs or acetaminophen can reduce pain and inflammation. Some patients benefit from short-term muscle relaxants for nighttime spasm. Discuss risks (e.g., GI, kidney) with your clinician (StatPearls, 2024).
Image-guided injections: When pain persists despite therapy, ultrasound- or CT-guided injections (local anaesthetic with corticosteroid) can reduce inflammation around the nerve and provide a window of relief to progress rehab. Small studies and reviews suggest botulinum toxin (“botox for piriformis syndrome”) can relax the muscle and decrease pain for several weeks to months, though availability and indications vary; evidence is promising but not definitive.
Surgery: Rarely required. Reserved for refractory cases where imaging and diagnostic injections strongly implicate deep gluteal compression and conservative care has failed. Procedures may involve releasing the piriformis or decompressing the sciatic nerve (HSS, 2024).
At-Home Relief: A Practical, Daily Plan
You can start a simple plan now to calm symptoms and restore function. Always move within “mild discomfort”
(3–4/10), not sharp pain.
A starter routine: three stretches (piriformis muscle stretches)
1) Supine figure-4 stretch: Cross the ankle over the opposite knee, gently pull the thigh toward your chest, hold 20–30
seconds, 2–3 reps.
2) Knee-to-opposite-shoulder stretch: Lying on your back, bring the knee toward the opposite shoulder, hold 20–30 seconds, 2–3 reps.
3) Seated figure-4 hinge: Sit tall, cross ankle over knee, hinge forward slightly, hold 20–30 seconds, 2–3 reps.
Do 1–2 sets daily. Progress ranges slowly.
- Self-myofascial release: ball and foam rolling techniques
- Use a tennis or lacrosse ball on the buttock (avoid direct pressure on the sciatic nerve if it produces sharp, radiating
pain). Roll for 60–90 seconds, 1–2 times/day. - Foam roll glutes and lateral hip. Follow with gentle stretching.
Sitting and driving ergonomics
- Keep feet flat, knees slightly below hips, sit on both sit bones (avoid crossing legs)
- Use a firm cushion or wedge; avoid soft couches
- For driving: slide seat forward to reduce hip flexion; take a 2–3 minute walk break every 45–60 minutes on long trips
These at-home measures align with common guidance from clinical sources and physical therapy practice.
Recovery Timeline and What to Expect
Acute vs. chronic: Many acute cases improve within 2–6 weeks with consistent self-care and physical therapy. Chronic
cases (months of symptoms) may take 8–12+ weeks, with periodic flare-ups that become milder and less frequent.
- When to seek medical care:
- If pain is severe, radiates below the knee, or you have numbness/weakness, get a clinical assessment.
If symptoms persist beyond two weeks or interfere with daily activities despite self-management, consult a doctor online
with Apollo24|7 for further evaluation and personalised treatment. If red flags are present (e.g., bowel/bladder
changes), seek urgent in-person care.
Prevention: Keeping Your Piriformis Happy
Hip and core strength balance:
- Twice weekly: side planks, hip abduction/hinge work, single-leg Romanian deadlifts, clamshells, step-downs
- Aim for control, not fatigue; quality reps prevent compensations
Footwear and stride tips for runners:
- Consider cadence around 165–180 steps/minute to reduce overstriding
- Gradually adapt to new footwear; rotating pairs can reduce repetitive load
- Incorporate strides on flat terrain before resuming hills
Microbreaks and mobility snacks:
- Every 20–30 minutes of sitting: 60–90 seconds of movement (hip circles, mini-squats, short walk)
- Set reminders; pair movement with routine tasks (calls, coffee)
Myths and Misconceptions
- Is it always the piriformis? No. “Deep gluteal syndrome” recognises that other structures (e.g., obturator internus, fibrous bands) can compress the sciatic nerve. Don’t assume; assess.
- “Sitting on the wallet” causes piriformis syndrome: Prolonged asymmetric pressure can aggravate symptoms, but it’s one of many contributors. The fix is broader: posture, breaks, strength, and movement variety.
- More stretching is always better: Overstretching an irritated nerve-muscle interface can worsen symptoms. Prioritise
gentle mobility, then strengthen and control range.
Measuring Progress (and When to Pivot)
- Pain and function scores: Use a simple 0–10 pain scale, the Lower Extremity Functional Scale (LEFS), and a daily
“sitting tolerance” log to quantify improvements. - Movement metrics: Track single-leg balance time, step count, and minutes to symptom onset in sitting/driving.
- When to add testing: If progress stalls despite 4–6 weeks of consistent therapy, consider clinician review. In select cases, checking vitamin D (linked to musculoskeletal pain) or HbA1c (if neuropathy is suspected) may be relevant; Apollo24|7 offers convenient home collection for tests like vitamin D or HbA1c.
Working With Your Care Team
Which specialist to see: Start with a primary care physician, sports medicine doctor, or physical therapist. Pain medicine specialists and physiatrists often guide injections. Surgeons enter the picture only after exhaustive conservative care.
Telehealth and Apollo24|7: If you need quick guidance on exercises, medications, or whether to pursue imaging, consult a doctor online with Apollo24|7. If your condition does not improve after trying these methods, book a physical visit to a doctor with Apollo24|7 for hands-on assessment and potential referral.
Cost and expectations: Most patients improve with a low-cost mix of self-care and PT; injections add cost but can accelerate progress when appropriately used. Set realistic goals: better sitting tolerance, fewer flare-ups, and a sustainable activity plan.
Conclusion
Piriformis syndrome is frustrating but fixable. The signs—deep buttock pain, sitting intolerance, and sometimes leg symptoms—reflect a sensitive interface between a small hip muscle and the sciatic nerve. What leads to those signs is almost always a mix of load (prolonged sitting, tough workouts), local muscle balance (hip stability), and sometimes unique anatomy. Injections can help break stubborn pain cycles, while surgery remains a last resort. If pain lingers or you’re unsure whether it’s piriformis syndrome or spine-related sciatica, consult a doctor online with Apollo24|7 to personalise your next steps. With steady effort and the right guidance, you can get back to comfortable sitting, confident movement, and the activities you enjoy—without the constant tug of deep gluteal pain.
Consult Top General Practitioner for Personalised Advice
Consult Top General Practitioner for Personalised Advice

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr Syed Mateen Pasha
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Syed Ismail Ali
General Practitioner
7 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr. Debajyoti Goswami
Obstetrician and Gynaecologist
10 Years • MBBS,D.G.O(DNB),Adv. Infertility Tech.(AIIMS),Fellowship in Diabetes(U.K),Comprehensive Abortion Care(Govt. Of W.B), Certificate in Clinical Embryology(AIIMS, BHUBANESWAR)
Bankura
D.G Clinic, Bankura
(25+ Patients)
Consult Top General Practitioner for Personalised Advice

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr Syed Mateen Pasha
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Syed Ismail Ali
General Practitioner
7 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr. Debajyoti Goswami
Obstetrician and Gynaecologist
10 Years • MBBS,D.G.O(DNB),Adv. Infertility Tech.(AIIMS),Fellowship in Diabetes(U.K),Comprehensive Abortion Care(Govt. Of W.B), Certificate in Clinical Embryology(AIIMS, BHUBANESWAR)
Bankura
D.G Clinic, Bankura
(25+ Patients)
More articles from Piriformis Syndrome
Frequently Asked Questions
1) How do I know if it’s piriformis syndrome or a herniated disc?
Piriformis syndrome usually causes buttock-predominant pain worse with sitting and hip positions; a disc herniation often adds back pain and worsens with coughing/sneezing. A clinician can differentiate with an exam and, if needed, imaging. If symptoms persist, consult a doctor online with Apollo24|7.
2) What are the best piriformis syndrome exercises?
A balanced routine includes gentle piriformis muscle stretches, glute medius strengthening (clamshells, side planks), and nerve gliding exercises. Start low, go slow, and avoid aggressive stretching that increases radiating pain.
3) Do injections work for piriformis syndrome?
Ultrasound-guided injections (local anaesthetic ± corticosteroid) can reduce pain and enable better rehab. “Botox for piriformis syndrome” is an option in select cases; evidence suggests benefit for some patients, but it’s not first-line.
4) How long does piriformis syndrome take to heal?
Many improve in 2–6 weeks with consistent self-care and physical therapy. Chronic cases may need 8–12+ weeks. Track sitting tolerance and function to judge progress.
5) Can I keep running with piriformis syndrome?
Often yes, if symptoms are mild. Reduce hills/speed work, increase cadence slightly, and add hip stability work. If pain worsens or radiates below the knee, scale back and consult a clinician.