What Leads To Signs Of Piriformis Syndrome Treatment
"Explore the most effective treatments for Piriformis Syndrome. Learn about the causes, signs, and symptoms, and discover exercises, stretches, and therapies that can provide lasting relief."'

Written by Dr. Shaik Abdul Kalam
Reviewed by Dr. D Bhanu Prakash MBBS, AFIH, Advanced certificate in critical care medicine, Fellowship in critical care medicine
Last updated on 13th Jan, 2026
Introduction:
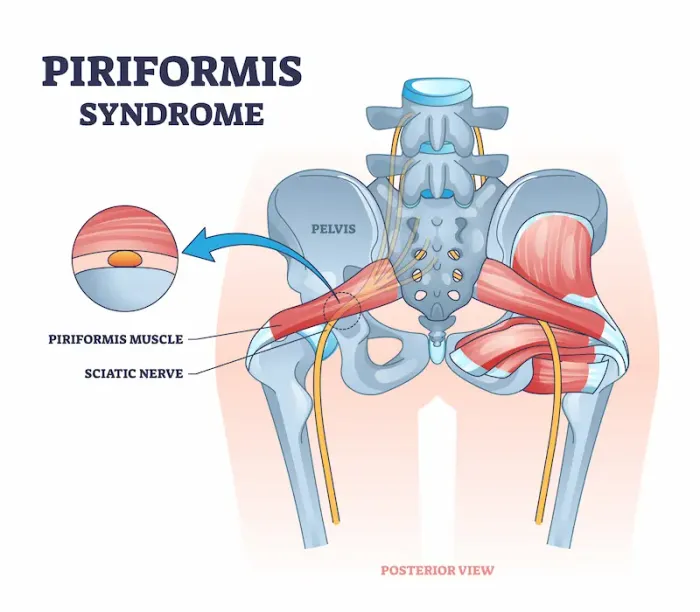
That sharp, burning pain deep in your buttock that shoots down your leg when you sit for too long—it’s a common complaint often mistaken for a herniated disc. But what if the culprit is a small, hidden muscle in your hip called the piriformis? Piriformis syndrome occurs when this muscle spasms, tightens, or swells, compressing the nearby sciatic nerve and leading to a unique set of challenges. Understanding what leads to these signs is the first and most critical step toward effective piriformis syndrome treatment. This comprehensive guide will walk you through the root causes, how to accurately identify the symptoms, and the full spectrum of treatment options—from simple at-home stretches to advanced medical interventions—to help you find lasting relief and get back to living your life without pain.
What is Piriformis Syndrome? The Hidden Cause of Sciatic Pain
Piriformis syndrome is a neuromuscular disorder where the piriformis muscle, located deep within the buttocks, compresses or irritates the sciatic nerve. This compression mimics the symptoms of true sciatica, making it a frequent source of misdiagnosis. The piriformis muscle is crucial for hip rotation and stability, connecting the lower spine to the top of the femur. For most people, the sciatic nerve runs underneath this muscle. However, in a significant portion of the population (an estimated 15-20%), the sciatic nerve pierces through the piriformis muscle, making them inherently more susceptible to this syndrome.
The Piriformis Muscle: Your Body's Unsung Hero
Think of the piriformis as a key stabilizer for your hip joint. Every time you walk, run, or shift your weight from one foot to the other, this muscle is actively working to rotate your hip and abduct your thigh. Its deep location means it doesn't get the attention that larger muscles like the glutes do, but its role is vital for fluid, pain-free movement.
Sciatica vs. Piriformis Syndrome: Untangling the Confusion
The primary difference lies in the origin of the pain. True sciatica is typically caused by compression at the nerve root in the lower spine, often from a herniated disc or spinal stenosis. Piriformis syndrome, however, is an extraspinal cause of sciatica—the compression happens far away from the spine, in the buttock. A key distinguishing factor is that piriformis syndrome rarely causes back pain, whereas true sciatica often does. This is a critical distinction that guides effective piriformis syndrome treatment.
H2: What Triggers Piriformis Syndrome? The Root Causes Explored
Identifying the trigger is paramount to successful treatment. The causes can be categorized into two main types.Consult Top Specialists
Primary vs. Secondary Piriformis Syndrome
• Primary (Anatomical): This is rare and due to an innate anatomical variation, such as the sciatic nerve splitting through the piriformis muscle or an abnormally positioned muscle belly. This predisposes individuals to symptoms from a younger age.
• Secondary (Acquired): This is the most common form. It occurs due to an event or condition that causes the piriformis muscle to compress the nerve. This is where most piriformis syndrome treatment plans begin their focus.
Common Lifestyle and Activity-Related Triggers
• Prolonged Sitting: Especially on hard surfaces or with a wallet in the back pocket ("wallet sciatica").
• Repetitive Stress: Activities like long-distance running, cycling, or climbing stairs that involve repeated hip flexion and rotation.
• Overuse or a Sudden Increase in Activity: Jumping into a new workout routine without proper conditioning.
• Poor Biomechanics: Weak glutes or core muscles force the piriformis to overwork to stabilize the hip.
Underlying Anatomical Factors
• Previous Trauma: A fall directly onto the buttocks, a car accident, or a hard impact can cause inflammation, scarring, or muscle spasms.
• Leg Length Discrepancy: Even a small difference can alter pelvic alignment and muscle function.
• Muscle Imbalances: Tight hip flexors and weak abductors create a dysfunctional movement pattern that overloads the piriformis.
Recognizing the Signs: Symptoms of Piriformis Syndrome
The symptoms can range from a mild annoyance to debilitating pain, often worsening with specific activities.
The Classic Symptom: Radiating Buttock Pain
The hallmark sign is a tender, aching pain deep within the buttock, approximately where your back pocket is. It's often described as a "knot" that's hard to massage away.
Beyond the Buttock: Pain Down the Leg and Other Sensations
The pain can travel down the back of the thigh, calf, and even into the foot—a sensation known as radiculopathy. This is often accompanied by:
Numbness and Tingling (Paresthesia) along the path of the sciatic nerve.
Burning or shooting pain that makes sitting difficult beyond 15-20 minutes.
Discomfort that is exacerbated by walking upstairs, squatting, or running.
When to See a Doctor: Red Flags and Serious Concerns
While often manageable conservatively, certain symptoms warrant immediate medical attention. If you experience sudden, severe pain, loss of bladder or bowel control, or significant leg weakness, seek emergency care. These could indicate a more serious spinal condition like cauda equina syndrome. For persistent deep gluteal pain syndrome, it's wise to consult a professional. If your symptoms persist beyond two weeks, consult a doctor online with Apollo24|7 for further evaluation and to rule out other causes.
How is Piriformis Syndrome Diagnosed?
There is no single definitive test; diagnosis is primarily clinical, based on history and physical examination.
The Physical Examination: FAIR Test and Others
A physician or physical therapist will perform specific maneuvers designed to stretch or contract the piriformis muscle to reproduce your symptoms. The most common is the FAIR test (Flexion, Adduction, and Internal Rotation), where they position your hip to passively stretch the piriformis. Pain during this test is a strong indicator. They will also palpate the muscle for tenderness.
The Role of Imaging: MRI, Ultrasound, and EMG
Imaging is used less to diagnose piriformis syndrome and more to exclude other pathologies.
MRI of the Lumbar Spine: Rules out disc herniation or spinal stenosis as the cause of sciatica.
MRI of the Pelvis: Can sometimes show an enlarged or inflamed piriformis muscle.
Diagnostic Ultrasound: Can visualize the muscle in real-time and assess for spasms.
Electromyography (EMG): Can help differentiate between nerve compression in the spine versus in the buttock.
Effective Piriformis Syndrome Treatment Strategies
Treatment is almost always progressive, starting with the least invasive options.
First-Line Conservative Treatments
This is the cornerstone of management, with a success rate of over 80%.
Activity Modification: Avoiding activities that trigger pain (e.g., prolonged sitting, running).
Physical Therapy: The gold standard. A PT will design a program focused on:
Targeted Piriformis Stretching Routine
Gentle, consistent stretching is paramount. Examples include the supine piriformis stretch (figure-four stretch) and the seated pigeon pose. Hold stretches for 30 seconds and repeat 3 times daily.
Strengthening Exercises for Hip Stability
Strengthening the gluteus medius, maximus, and core muscles offloads the piriformis. Exercises like clamshells, bridges, and side-lying leg raises are fundamental.
Pain Management and Anti-Inflammatory Approaches
• NSAIDs: Medications like ibuprofen or naproxen can reduce inflammation and pain in the short term.
• Heat and Ice Therapy: Ice can reduce acute inflammation, while heat can relax muscle spasms and improve blood flow.
• Massage Therapy: Deep tissue massage or myofascial release can help break up muscle knots.
Advanced and Interventional Treatment Options
If conservative measures fail after 3-6 months, other options exist:
• Corticosteroid Injections: An injection of anesthetic and corticosteroid directly into the piriformis muscle under ultrasound guidance can provide significant pain relief and break the cycle of pain-spasm-pain.
• Botox Injections: Botulinum toxin (Botox) can be injected to chemically relax the spasming muscle for several months, allowing for more effective physical therapy.
• Surgery: Piriformis release surgery is a last resort, considered only in severe, refractory cases. It involves cutting the piriformis tendon to relieve pressure on the sciatic nerve.
Consult Top Specialists
Conclusion: Your Path to a Pain-Free Life
Dealing with the nagging, shooting pain of piriformis syndrome can be frustrating, but it's important to remember that it is a highly treatable condition. The journey to relief begins with understanding the unique root causes—whether it's from prolonged sitting, muscle imbalances, or overuse. By committing to a consistent regimen of targeted piriformis syndrome stretches, strengthening your hip stabilizers, and making smart ergonomic adjustments to your daily life, you can effectively manage and often completely resolve your symptoms. Listen to your body, be patient with the process, and don't hesitate to seek professional guidance to create a personalized plan. If your condition does not improve after trying these conservative methods, book a physical visit to a doctor or a physiotherapist to get a tailored treatment plan and finally step into a life free from pain.
Consult Top Specialists

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr Syed Mateen Pasha
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Syed Ismail Ali
General Practitioner
7 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr. Harshendra Jaiswal
General Physician/ Internal Medicine Specialist
12 Years • MBBS , MD (General medicine)
Kolkata
108 DHANA DHANVANTARI Clinic, Kolkata
(25+ Patients)
Consult Top Specialists

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr Syed Mateen Pasha
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Syed Ismail Ali
General Practitioner
7 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr. Harshendra Jaiswal
General Physician/ Internal Medicine Specialist
12 Years • MBBS , MD (General medicine)
Kolkata
108 DHANA DHANVANTARI Clinic, Kolkata
(25+ Patients)
More articles from Piriformis Syndrome
Frequently Asked Questions
1. What is the fastest way to relieve piriformis syndrome?
While no fix is instant, a combination of avoiding aggravating activities, applying ice to the area for 15 minutes, and gently performing a supine piriformis stretch can provide the most rapid initial relief from acute pain.
2. Can piriformis syndrome be cured permanently?
Yes, for most people. Through a dedicated regimen of physical therapy to correct underlying muscle imbalances and learning to avoid specific triggers, many individuals experience a permanent resolution of symptoms without the need for surgery.
3. What is the best sleeping position for piriformis syndrome?
Sleeping on your back is often best. Place a pillow under your knees to slightly elevate them and reduce tension on the piriformis and sciatic nerve. If you prefer to sleep on your side, sleep on the non-painful side with a pillow between your knees to keep your hips aligned.
4. Are there any exercises to avoid piriformis syndrome?
Yes, you should temporarily avoid high-impact activities like running and jumping, as well as exercises that deeply stretch or load the hip in internal rotation, such as pigeon pose (if it causes pain), and prolonged sitting exercises like cycling.
5. How long does it take for piriformis syndrome to heal?
With consistent conservative treatment like stretching and physical therapy, many people see significant improvement within a few weeks. However, completely resolving the issue and strengthening the supporting muscles can take 4-6 weeks or longer, depending on the severity and chronicity of the condition.

