Piriformis Syndrome Treatment: Relieve Sciatic Nerve Pain
Discover effective treatment strategies for piriformis syndrome—a hidden cause of sciatic nerve pain. Learn symptoms, causes, stretches, and prevention tips for lasting relief.

Written by Dr. M L Ezhilarasan
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 13th Jan, 2026

Introduction
Have you ever experienced a deep, nagging pain in your buttock that radiates down your leg, making sitting or walking a challenge? You might have immediately thought of sciatica, but the real culprit could be a small, powerful muscle hidden beneath your glutes: the piriformis. Piriformis syndrome occurs when this muscle spasms and compresses the sciatic nerve, leading to pain, tingling, and numbness that mimics other spinal conditions. Understanding what leads to this syndrome is the first step toward effective treatment. This comprehensive guide will walk you through the causes, symptoms, and, most importantly, the multi-phase treatment strategies—from simple home stretches to advanced medical interventions—that can help you find lasting relief and get back to a pain-free life.
What is Piriformis Syndrome? The Hidden Cause of Sciatica
Piriformis syndrome is a neuromuscular disorder that occurs when the piriformis muscle, located in the buttock region, compresses or irritates the sciatic nerve. It's often called "wallet sciatica" because sitting on a wallet for prolonged periods is a classic trigger. While the symptoms mirror traditional sciatica from a lumbar spine issue, the origin is muscular, making its diagnosis and treatment unique.
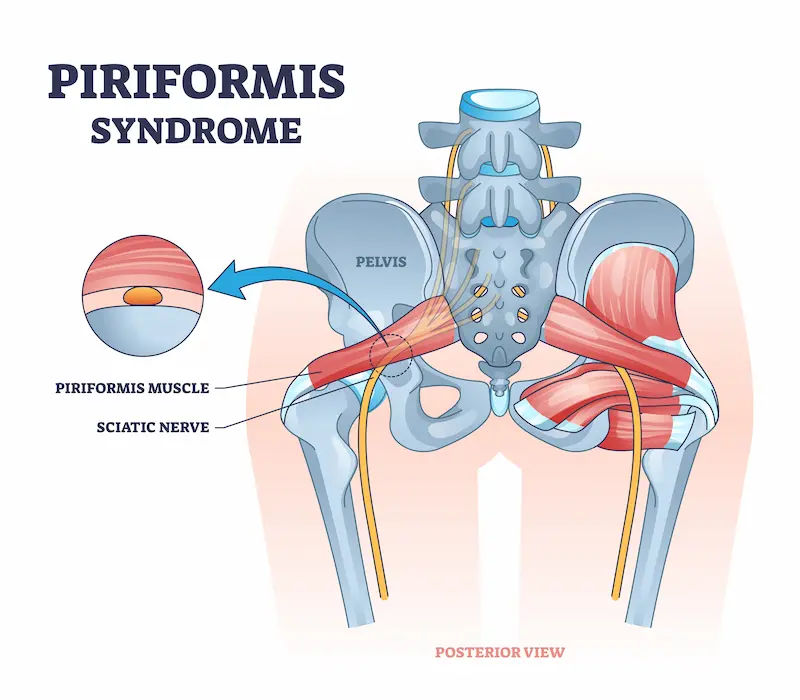
Anatomy 101: Your Piriformis Muscle and Sciatic Nerve
The piriformis is a flat, band-like muscle located deep in the buttocks, behind the gluteus maximus. It connects the lower spine to the top of the femur (thigh bone) and is crucial for hip rotation and stability. The sciatic nerve is the longest and thickest nerve in the body, running from the lower back, through the buttocks, and down each leg. In most people, the sciatic nerve runs underneath the piriformis muscle. However, in a significant portion of the population (estimated 15-20%), the sciatic nerve pierces through the piriformis muscle, making these individuals inherently more susceptible to nerve compression if the muscle becomes tight or inflamed.
Is It Piriformis Syndrome or a Herniated Disc?
Differentiating between piriformis syndrome and a herniated disc is critical for proper treatment. While both can cause sciatic nerve pain, key differences exist. Piriformis syndrome pain is often more localised in the buttock and tender to the touch. The pain may be triggered by sitting for long periods or climbing stairs. In contrast, pain from a herniated disc often originates in the lower back and is typically worsened by actions like bending forward, coughing, or sneezing. A healthcare professional can perform specific physical tests (like the FAIR test) to help distinguish between the two. If you're unsure about the source of your pain, consult a doctor online with Apollo24|7 for a preliminary evaluation.
What Leads to Piriformis Syndrome? Uncovering the Root Causes
The primary cause of piriformis syndrome is the compression of the sciatic nerve by the piriformis muscle. This compression can happen due to several reasons, which are categorised as primary or secondary.
Primary vs. Secondary Piriformis Syndrome
Primary Piriformis Syndrome: This is less common and is due to an anatomic variation, such as the sciatic nerve passing through the piriformis muscle belly or a split piriformis muscle. This predisposes individuals to nerve compression even with minor muscle changes.
Secondary Piriformis Syndrome: This is far more common. It occurs due to a precipitating event that causes the muscle to cramp, spasm, hypertrophy (enlarge), or become inflamed, thereby compressing the nerve. This is what most treatment plans address.Consult a Neurologist for Personalised Advice
Common Triggers and Risk Factors
Several factors can lead to the development of secondary piriformis syndrome:
• Overuse or Injury: A sudden fall onto the buttocks, a car accident, or a direct blow can injure the piriformis muscle, leading to inflammation and spasm.
• Prolonged Sitting: Sitting for long hours on hard surfaces or with a wallet in the back pocket is a classic cause.
• Repetitive Stress: Activities that involve repetitive, forceful movement of the legs and hips, such as long-distance running, cycling, or climbing, can overwork and irritate the muscle.
• Gait Abnormalities: Walking with an abnormal pattern can place uneven stress on the hip musculature.
• Leg Length Discrepancy: Even a small difference in leg length can alter pelvic mechanics and strain the piriformis.
• Weak Glutes or Core Muscles: When the primary movers (gluteus maximus, core) are weak, smaller stabiliser muscles like the piriformis are forced to overcompensate, leading to fatigue and spasm.
• Previous Surgery: Hip or lower back surgery can lead to scar tissue formation or altered biomechanics that affect the piriformis.
Recognising the Signs: Symptoms of Piriformis Syndrome
The symptoms of piriformis syndrome can vary from mild annoyance to debilitating pain. Common signs include:
• A dull, aching pain deep in the buttock.
• Tenderness in the buttock area (you can often pinpoint the pain).
• Pain that radiates down the back of the thigh, calf, and sometimes into the foot (sciatica).
• Tingling (pins and needles) or numbness in the buttock and down the leg.
• Pain that worsens after sitting for prolonged periods, especially on hard chairs.
• Pain when climbing stairs, walking, or running.
• Reduced range of motion in the hip joint.
• Some people may even experience pain during bowel movements or, rarely, sexual intercourse due to the muscle's proximity to other pelvic structures.
How is Piriformis Syndrome Diagnosed?
Diagnosing piriformis syndrome can be challenging as there is no single definitive test. It is often a diagnosis of exclusion, meaning other conditions like herniated discs or spinal stenosis are ruled out first. A doctor or physical therapist will:
1. Take a Medical History: Discussing your symptoms, activities, and any recent injuries.
2. Perform a Physical Exam: This involves palpating (pressing on) the piriformis muscle to reproduce the pain. They will also check your range of motion and strength.
3. Conduct Provocative Tests: Specific manoeuvres like the FAIR test (Flexion, Adduction, and Internal Rotation of the hip) can stretch the piriformis and elicit symptoms.
4. Order Imaging Tests: While X-rays, MRIs, or CT scans cannot show piriformis syndrome itself, they are used to rule out other spinal problems that could be causing the sciatic pain. In some cases, an MR Neurography can visualise nerve compression.
Effective Piriformis Syndrome Treatment Strategies
Treatment for piriformis syndrome is almost always non-surgical and follows a progressive, phased approach.
Phase 1: Immediate Relief and Home Remedies
The initial goal is to reduce pain and inflammation.
• The RICE Method (Rest, Ice, Compression, Elevation): Avoid activities that trigger pain. Apply ice packs to the tender area for 15-20 minutes several times a day to reduce inflammation. Compression with a bandage and elevating the legs can also help.
• Heat Therapy for Muscle Relaxation: After the initial 48-72 hours of acute pain, applying a heating pad can help relax the tight muscle and improve blood flow, easing spasms.
• Over-the-Counter Medications: NSAIDs like Ibuprofen or Naproxen can help manage pain and reduce inflammation in the short term.
Phase 2: Stretching and Rehabilitation Exercises
This is the cornerstone of long-term recovery. Once acute pain subsides, gentle stretching and strengthening begin.
Top 3 Piriformis Stretches for Immediate Relief:
1. Supine Piriformis Stretch: Lie on your back with both knees bent. Cross the painful leg over the other knee, forming a "figure 4." Gently pull the bottom thigh toward your chest until you feel a stretch in the buttock.
2. Seated Piriformis Stretch: Sit in a chair with your feet flat. Place the ankle of your painful leg on the knee of the other leg. Gently lean forward until you feel a deep stretch.
3. Pigeon Pose (Yoga): A deep stretch popular in yoga that directly targets the piriformis and hip rotators.
Strengthening Supporting Muscles: A physical therapist will design a programme to strengthen weak gluteal muscles, core, and hip abductors to prevent the piriformis from overworking.
Phase 3: Professional Medical Treatments
If conservative measures aren't enough, further options are available.
• Physical Therapy and Manual Techniques: A physical therapist can use deep tissue massage, myofascial release, instrument-assisted soft tissue mobilisation (IASTM), and dry needling to release the tight muscle and break up adhesions.
• Medications for Pain and Inflammation: A doctor may prescribe stronger muscle relaxants or anti-inflammatory drugs.
• Advanced Interventions: Injections and Surgery: For persistent cases, an image-guided injection of a local anaesthetic and corticosteroid directly into the piriformis muscle can provide significant relief. In rare, severe cases that don't respond to any other treatment, piriformis release surgery may be considered to cut the tendon and relieve pressure on the sciatic nerve. If your condition does not improve after trying conservative methods, book a physical visit to a doctor with Apollo24|7 to discuss these advanced options.
Prevention: How to Stop Piriformis Syndrome from Returning
Preventing a recurrence involves addressing the underlying causes:
• Ergonomics: Avoid sitting for long periods. Use a standing desk, take frequent walking breaks, and never sit on your wallet.
• Proper Form: If you're an athlete, ensure you use proper technique during running, cycling, or weight training. Consider a gait analysis.
• Consistent Stretching: Incorporate piriformis and hip stretches into your daily routine, especially after exercise.
• Strengthening Programme: Regularly perform exercises that target the glutes, hamstrings, and core to maintain balanced muscle strength around the hip and pelvis.
• Warm-Up and Cool-Down: Always properly warm up before activity and cool down with stretches afterwards.
Conclusion
Piriformis syndrome, while painful and frustrating, is a highly treatable condition. The journey to relief begins with understanding the unique relationship between a small hip muscle and a major nerve. By identifying the triggers—be it prolonged sitting, overuse, or an underlying weakness—you can take proactive steps toward healing. A phased approach, starting with rest and ice, progressing to targeted stretches, and seeking professional care when needed, offers the best path to recovery. Remember, consistency with your exercise and stretching regimen is the key to not only overcoming the current pain but also preventing it from returning. Listen to your body, be patient with the process, and don't hesitate to seek expert guidance to get back to moving freely and without pain.Consult a Neurologist for Personalised Advice
Consult a Neurologist for Personalised Advice

Dr. Uddalak Chakraborty
Neurologist
8 Years • MBBS, MD(GENL.MED.),DM(NEUROLOGY)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr. Uddalak Chakraborty
Neurologist
8 Years • MBBS,MD(GENL. MED.),DM(NEUROLOGY)
Kolkata
VDC Clinic, Kolkata
(25+ Patients)

Dr. Ganeshgouda Majigoudra
Neurologist
10 Years • MBBS, MD ( GENERAL MEDICINE) DM (NEUROLOGY)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(175+ Patients)

Dr Debnath Dwaipayan
Neurosurgeon
9 Years • MBBS, MS(Gen. Surgery), DrNB (Neurosurgery)
Delhi
Apollo Hospitals Indraprastha, Delhi
Consult a Neurologist for Personalised Advice

Dr. Uddalak Chakraborty
Neurologist
8 Years • MBBS, MD(GENL.MED.),DM(NEUROLOGY)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr. Uddalak Chakraborty
Neurologist
8 Years • MBBS,MD(GENL. MED.),DM(NEUROLOGY)
Kolkata
VDC Clinic, Kolkata
(25+ Patients)

Dr. Ganeshgouda Majigoudra
Neurologist
10 Years • MBBS, MD ( GENERAL MEDICINE) DM (NEUROLOGY)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(175+ Patients)

Dr Debnath Dwaipayan
Neurosurgeon
9 Years • MBBS, MS(Gen. Surgery), DrNB (Neurosurgery)
Delhi
Apollo Hospitals Indraprastha, Delhi
More articles from Piriformis Syndrome
Frequently Asked Questions
1. What is the fastest way to fix piriformis syndrome?
While no fix is instant, combining immediate rest and ice with gentle piriformis stretching (like the supine stretch) can provide the most rapid relief. Avoiding aggravating activities is crucial in the first 48 hours.
2. Can piriformis syndrome be cured permanently?
Yes, for most people, piriformis syndrome can be effectively managed and considered 'cured' with consistent conservative treatment like physical therapy and lifestyle modifications. However, without addressing the underlying cause (e.g., poor sitting habits, weak glutes), it can recur.
3. What should I avoid doing with piriformis syndrome?
Avoid prolonged sitting, especially on hard surfaces. Also, avoid activities that aggravate the pain, such as running, cycling, or exercises that deeply externally rotate the hip (like some yoga poses). Don't stretch into sharp, intense pain.
4. Is walking good for piriformis syndrome?
Yes, in moderation. Short, gentle walks can help reduce inflammation and prevent stiffness. However, long walks or walking with poor form that aggravates your pain should be avoided until symptoms improve.
5. How long does a typical piriformis syndrome flare-up last?
The duration varies. A mild flare-up might resolve in a few days with rest and ice. A more severe case caused by an injury could take several weeks of consistent stretching and physical therapy to fully heal.