Understanding Vaginal Cancer: Causes, Symptoms, Risk Factors & Prevention
Learn about vaginal cancer, including its causes, symptoms, risk factors, and prevention. Understand early warning signs, diagnosis, and steps to protect your health.

Written by Dr. Mohammed Kamran
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 13th Jan, 2026

Introduction
Vaginal cancer is a rare gynaecologic cancer that begins in the vagina, the muscular tube connecting the outer genitals to the uterus. While its rarity means it's not at the forefront of most women's health concerns, understanding what leads to the signs of vaginal cancer is crucial for early detection and successful treatment. Often, the early symptoms are subtle and mistaken for less serious conditions, which is why awareness is your first line of defense. This article will demystify this condition, exploring the primary causes, from HPV infection to age-related changes, and detailing the key risk factors that can increase susceptibility. We will guide you through the symptoms you should never ignore, the diagnostic process, and the most effective strategies for prevention. Knowledge empowers you to take charge of your gynaecological health and seek timely medical advice.
Understanding Vaginal Cancer: A Rare But Serious Condition
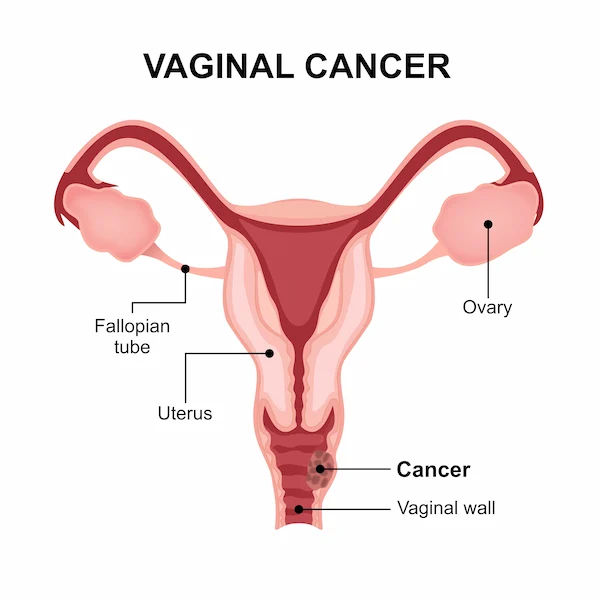
Vaginal cancer accounts for only about 1% of all cancers in the female reproductive system. It typically occurs in the cells that line the surface of your vagina, often called the birth canal. It's important to distinguish it from more common cancers like cervical cancer, though they can share similar causes and symptoms. One key aspect of understanding this disease is knowing that cancer found in the vagina may have actually started somewhere else, such as the cervix or uterus, and spread there.
Primary Vaginal Cancer vs. Secondary Cancer
Primary vaginal cancer originates in the vagina itself. This is the less common scenario.
Secondary vaginal cancer means the cancer has spread (metastasized) to the vagina from another part of the body, such as the cervix, vulva, endometrium, or even distant organs like the bladder or rectum. Treatment for secondary cancer focuses on the primary source.
The Main Types of Vaginal Cancer
The type is determined by the cell where the cancer began, which influences treatment options:
Squamous cell carcinoma: This type begins in the thin, flat squamous cells that line the surface of the vagina. It is the most common type, making up about 85% of cases, and usually grows slowly. It's most frequently found in the upper third of the vagina, often in women over 60.
Adenocarcinoma: This type begins in the glandular cells on the surface of the vagina that secrete mucus. It is more common than squamous cell carcinoma in women under 50.
Other rare types: These include melanoma (in pigment-producing cells), sarcoma (in muscle or connective tissue cells), and clear cell adenocarcinoma (which has been linked to prenatal exposure to the drug DES, or diethylstilbestrol).
Consult a Gynaecologist or Oncologist for the best advice
What Leads to Vaginal Cancer? The Primary Causes and Triggers
In most cases, vaginal cancer doesn't have a single clear cause. Instead, it is understood to develop due to a combination of factors that lead to genetic mutations in healthy vaginal cells. These mutations cause cells to grow and multiply uncontrollably, forming a mass of cancerous cells (a tumour). The key triggers for these mutations are:
The Human Papillomavirus (HPV) Connection
HPV is the most significant risk factor and is implicated in up to 75% of squamous cell vaginal cancers. HPV is a common sexually transmitted infection with many strains. While most infections clear on their own, persistent infection with high-risk HPV strains (like HPV 16 and 18) can cause cellular changes that may eventually lead to cancer over many years. The virus interferes with the normal cell cycle, leading to uncontrolled growth.
The Role of Age and Cellular Changes
Age is a major factor, with most cases diagnosed in women over 60. As women age, cellular changes in the vaginal lining can occur. For some, these changes can become pre-cancerous, a condition known as vaginal intraepithelial neoplasia (VAIN). If left undetected and untreated, VAIN can progress to invasive vaginal cancer.
Pre-existing Conditions: VAIN and Cervical Cancer
A history of certain pre-cancerous or cancerous conditions dramatically increases risk.
VAIN: As mentioned, this is a direct precursor.
Cervical Cancer: Women with a history of cervical cancer or pre-cancer (CIN) have a higher risk of developing vaginal cancer*. This is likely due to the shared risk factor of HPV and the concept of "field cancerisation," where the entire genital tract has been exposed to the same carcinogens.
Recognising the Signs: Symptoms of Vaginal Cancer
Early-stage vaginal cancer may not cause any noticeable signs. When symptoms do appear, they are often mistaken for less serious issues like infections or menstrual changes. This is why any persistent change should be evaluated by a doctor.
Early-Stage Symptoms That Are Easy to Overlook
Unusual vaginal bleeding: This is the most common symptom. It includes bleeding after menopause, bleeding after sexual intercourse, or bleeding between periods.
Watery vaginal discharge: A discharge that may be persistent and have a foul odor.
A palpable lump or mass in the vagina: Something you or your doctor might feel during a self-exam or pelvic exam.
Advanced Symptoms That Demand Immediate Attention
As the cancer grows, symptoms become more pronounced and may include:
Painful urination (dysuria) or frequent urination.
Pelvic pain, especially during sexual intercourse.
Constipation.
Pain in the back or legs.
Swelling in the legs.
If you experience any unusual vaginal bleeding, especially after menopause, or any other symptoms that persist for more than two weeks, it is essential to consult a doctor. You can book an online consultation with a gynaecologist on Apollo24|7 for a preliminary evaluation and to determine if a physical visit is needed.
Key Risk Factors That Increase Susceptibility
Beyond the direct causes, several factors can increase a woman's chance of developing this condition.
Behavioral and Lifestyle Factors
Smoking: Tobacco use is linked to many cancers, including vaginal cancer. The chemicals in tobacco can damage cellular DNA.
Multiple Sexual Partners & Early Sexual Activity: These behaviors increase the likelihood of exposure to HPV.
Weakened Immune System: Individuals with HIV/AIDS or those taking immunosuppressant drugs after an organ transplant have a reduced ability to fight off HPV infections, increasing cancer risk.
Medical History and Health Conditions
History of Cervical Pre-cancer or Cancer: This is one of the strongest risk factors.
Hysterectomy: Some studies suggest a potential link, though the reason is not entirely clear.
Prenatal DES Exposure: Women whose mothers took the drug DES (diethylstilbestrol) during pregnancy in the mid-1900s have a higher risk of a specific type called clear cell adenocarcinoma.
How is Vaginal Cancer Diagnosed?
Early diagnosis significantly improves outcomes. The process typically involves:
The Importance of Pelvic Exams and Pap Tests
Routine gynaecological care is your best defense. During a pelvic exam, a doctor visually and manually checks the vagina, cervix, uterus, and ovaries for any abnormalities. A Pap test (smear) collects cells from the cervix and, sometimes, the vagina to screen for pre-cancerous or cancerous changes. While primarily for cervical cancer, a Pap test can sometimes detect vaginal cancer or VAIN.
Advanced Diagnostic Procedures: Colposcopy and Biopsy
If an abnormality is found, the next step is usually a colposcopy. This procedure uses a special magnifying instrument (colposcope) to examine the vagina and cervix in detail. If any suspicious areas are seen, a biopsy is performed. This involves removing a small sample of tissue for laboratory analysis. A biopsy is the only definitive way to diagnose vaginal cancer. Apollo24|7 offers convenient home collection services for various tests, and while a biopsy requires a clinical procedure, your doctor can guide you through the entire diagnostic process.
Prevention and Early Detection Strategies
While not all cases can be prevented, you can take proactive steps to drastically reduce your risk.
HPV Vaccination: A Powerful Preventive Tool
Vaccines like Gardasil 9 protect against the high-risk HPV strains that cause most cervical and vaginal cancers. The vaccine is recommended for both girls and boys, ideally before they become sexually active (ages 11-12), but can be given up to age 45. This is the single most effective way to prevent HPV-related cancers.
The Critical Role of Regular Gynaecological Screenings
Do not skip your annual well-woman exam. Regular pelvic exams and Pap tests as recommended by your doctor are essential for catching pre-cancerous changes (VAIN) early, when they are most treatable and before they develop into invasive cancer.
Lifestyle Choices to Mitigate Risk
Quit Smoking: Eliminating tobacco use reduces your risk for numerous cancers.
Practice Safe Sex: Using condoms can reduce, though not eliminate, the risk of HPV transmission.
Know Your Body: Be aware of any changes in your vaginal health and report them to your doctor promptly.
Conclusion
Understanding what leads to the signs of vaginal cancer empowers you to be an active participant in your health journey. While the thought of any cancer can be frightening, knowledge is your greatest ally. The key takeaways are clear: the strong link to HPV underscores the importance of vaccination and safe sexual practices, and the subtlety of early symptoms highlights the irreplaceable value of regular gynaecological check-ups. Listening to your body and reporting persistent changes like unusual bleeding or discharge to your doctor can make a life-saving difference. Remember, vaginal cancer is highly treatable when caught in its early stages. Prioritise your well-being by scheduling your annual exam, discussing your risk factors with your healthcare provider, and taking proactive steps toward prevention. Your health is worth it.
Consult a Gynaecologist or Oncologist for the best advice
Consult a Gynaecologist or Oncologist for the best advice

Dr. Swati Shah
Surgical Oncologist
15 Years • DNB Surgical Oncology, certified Robotic Cancer Surgeon
Ahmedabad
Apollo Hospitals Gandhinagar, Ahmedabad
(25+ Patients)

Dr. V R N Vijay Kumar
Surgical Oncologist
9 Years • MBBS, MS (Gen. Surg.), DNB (Surg. Onco.)
Ahmedabad
Apollo Hospitals Gandhinagar, Ahmedabad

Dr. Sai Lakshmi Daayana
Gynaecological Oncologist
18 Years • MBBS, MRCOG
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
(225+ Patients)

Dr. Amit Choraria
Surgical Oncologist
18 Years • MBBS, MS (Surgery) Fellow, Surgical Oncology, Tata Medical Center (FSO) Fellow, European Board of Surgery (Surgical Oncology) (FEBS) Fellow, Minimal Access Surgery (FMAS) Fellow, Indian Association of Gastrointestinal Endosurgeons (FIAGES) UICC Fellow, Royal Marsden NHS, London, UK Visiting Scholar, Plastic Reconstructive Surgery, CGMH, Taiwan Fellow, Robotic Surgical Oncology, Vattikuti Foundation, USA
Kolkata
Apollo Multispeciality Hospitals , Kolkata, Kolkata

Dr. Navin Srinivasan
Obstetrician and Gynaecologist
9 Years • MBBS, MS, DNB (OBS-GYNAE), MCH (GYNE ONCOLOGY) MRCOG - 2 (Gold Medalist )
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru
More articles from Vaginal Cancer
Frequently Asked Questions
1. What is the most common first sign of vaginal cancer?
The most common and often first sign is unusual vaginal bleeding, particularly postmenopausal bleeding or bleeding after intercourse. However, early stages may have no symptoms at all.
2. Can a Pap smear detect vaginal cancer?
While the primary purpose of a Pap smear is to screen for cervical cancer, it can sometimes detect abnormal cells originating from the vagina, leading to a diagnosis of vaginal intraepithelial neoplasia (VAIN) or even vaginal cancer. However, it is not a guaranteed test for vaginal cancer.
3. Is vaginal cancer curable?
Yes, especially when diagnosed at an early stage. The five-year survival rate for early-stage vaginal cancer is very high. Treatment success depends on the type of cancer, its stage, and the patient's overall health.
4. What is the difference between vaginal and cervical cancer?
The key difference is the location where the cancer originates. Cervical cancer starts in the cells of the cervix (the lower part of the uterus that opens into the vagina), while vaginal cancer starts in the cells of the vagina itself. They share many risk factors, like HPV.
5. Who is most at risk for developing vaginal cancer?
The highest risk groups include women over 60, those with a persistent HPV infection, women with a history of cervical cancer or pre-cancer, and smokers.