Guide to Know About Risk Factors Vaginal Cancer
Learn about the main risk factors for vaginal cancer, helping you stay informed and take proactive steps for early detection and prevention.

Introduction
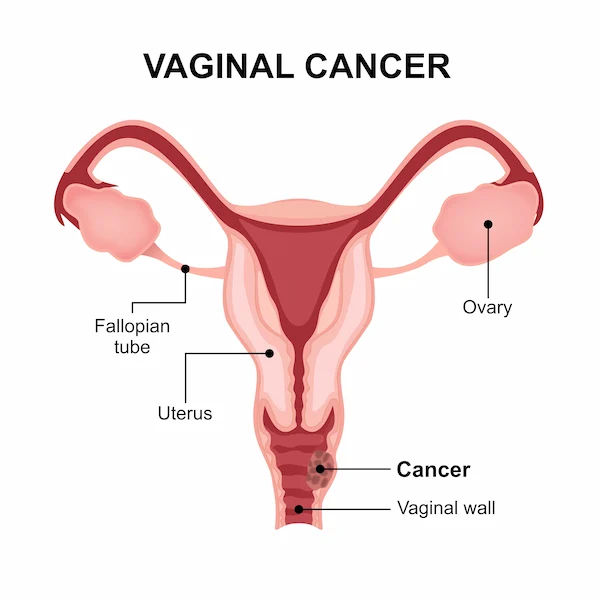
Vaginal cancer is a rare gynaecologic malignancy, but understanding its risk factors is a powerful step toward prevention and early detection. When abnormal cells develop in the tissues of your vagina, it can lead to this serious condition. Many women are more familiar with cervical or ovarian cancer, which makes awareness about vaginal cancer all the more critical. This guide will demystify the key elements that can increase a person's likelihood of developing this disease. We'll move beyond just listing factors and explore the why behind them, empowering you with knowledge about everything from the significant role of HPV to historical exposures and lifestyle choices. Whether you're looking to assess your own risk or simply become more informed about women's health, this comprehensive overview will provide the clarity and actionable insights you need to take control of your well-being.
The Primary Risk Factor: Age and Cellular Changes
While vaginal cancer can occur at any age, it is most frequently diagnosed in women over 60. The average age at diagnosis is around 67. This strong correlation with age is primarily due to the cumulative effect of cellular changes over time. Our cells are constantly regenerating, and with each division, there's a tiny chance for errors (mutations) to occur in the DNA. Over decades, these mutations can build up, potentially leading to uncontrolled cell growth, the hallmark of cancer. It's important to note that aging itself is not a cause, but it provides a longer window for other risk factors, like HPV infection, to cause significant damage. This is why regular gynaecological check-ups remain crucial throughout a woman's life, even after menopause.
The HPV Connection: A Major Preventable Cause
The human papillomavirus (HPV) is identified as the most significant and preventable risk factor for vaginal cancer, as well as for cervical, vulvar, and anal cancers. HPV is a common sexually transmitted infection; most sexually active people will contract it at some point. In the majority of cases, the immune system clears the virus naturally. However, persistent infection with high-risk strains of HPV (especially types 16 and 18) can lead to cellular changes that may become cancerous over many years.
How HPV Leads to Cancer
High-risk HPV produces proteins that interfere with the normal control mechanisms of host cells, particularly proteins known as tumor suppressors. When these "brakes" on cell division are disabled, infected cells can multiply uncontrollably, leading to pre-cancerous conditions and, eventually, invasive cancer. This process is slow, often taking 10 to 20 years, which highlights the critical importance of long-term monitoring.
Reducing Your HPV Risk
The most effective way to reduce your risk is through vaccination. The HPV vaccine is recommended for both adolescents and adults up to age 45 and protects against the high-risk strains most commonly linked to cancer. Additionally, practicing safe sex using condoms can reduce, though not eliminate, the risk of transmission. If you are concerned about your HPV status or have abnormal Pap smear results, consulting a gynaecologist online with Apollo24|7 can provide timely guidance on next steps.
Consult a Gynaecologic Oncologist for the best advice
DES Exposure: A Historical Risk Factor
Between the 1940s and 1971, a synthetic form of estrogen called diethylstilbestrol (DES) was prescribed to some pregnant women to prevent miscarriage. Unfortunately, daughters born to these women ("DES daughters") were found to have a significantly higher risk of developing a rare type of vaginal cancer called clear cell adenocarcinoma. This risk is highest for those in their teens and early 20s, but it persists throughout life. While DES is no longer used, this historical episode underscores how prenatal exposures can have long-lasting health consequences. If you believe you may be a DES daughter, informing your doctor is essential for appropriate screening.
Pre-Cancerous Conditions: VAIN Explained
Vaginal Intraepithelial Neoplasia (VAIN) is a pre-cancerous condition where abnormal cells are found on the surface lining of the vagina. These cells are not cancerous, but they have the potential to become cancer over time if left untreated. VAIN is often detected through a Pap test that shows abnormal results. It is frequently linked to persistent HPV infection.
The Link Between VAIN and Cervical Cancer
Women who have had cervical cancer or a pre-cancerous cervical condition (CIN) are at a higher risk of developing VAIN. This is likely because the entire lower genital tract was exposed to the same causative agent, primarily HPV. Successful treatment of cervical cancer does not eliminate the risk for VAIN, making ongoing vaginal screening an important part of long-term follow-up care.
Lifestyle and Environmental Contributors
Certain lifestyle choices can influence your overall cancer risk, including for vaginal cancer.
The Impact of Smoking
Chemicals in tobacco smoke are absorbed into the bloodstream and can concentrate in cervical and vaginal fluids. These carcinogens can damage the DNA of cells in the vaginal lining. Furthermore, smoking suppresses the local immune system, making it harder for the body to clear HPV infections, thereby compounding the risk.
Weakened Immunity and HIV
A healthy immune system is vital for fighting off infections like HPV and destroying abnormal cells before they can become cancerous. Conditions that weaken the immune system, such as Human Immunodeficiency Virus (HIV) or immunosuppressive medications after an organ transplant, substantially increase the risk of developing vaginal cancer and other HPV-related diseases.
Chronic Irritation and Previous Hysterectomy
Some studies suggest a potential link between long-term vaginal irritation and an increased risk of squamous cell carcinoma of the vagina. This irritation could be from the use of pessaries (devices to support pelvic organ prolapse) or other factors. However, the evidence is not as strong as for other risk factors like HPV. Additionally, women who have had a hysterectomy (surgical removal of the uterus), particularly for benign reasons, may have a lower overall risk of gynaecologic cancer, but it's crucial to remember that the vagina remains and requires continued screening as advised by a doctor.
Proactive Steps for Prevention and Early Detection
Knowledge of risk factors is only powerful if it leads to action. Here’s how you can be proactive.
The Power of the HPV Vaccine
As mentioned, vaccination is the single most effective way to prevent the HPV infections that cause the majority of vaginal cancers. It is a safe and powerful tool for both girls and boys.
The Role of Regular Pelvic Exams and Pap Tests
Routine gynaecological care is non-negotiable. Pelvic exams allow your doctor to visually and physically inspect the vagina and cervix. The Pap test (or smear) is designed to detect abnormal cells in the cervix that could become cancerous, but it can sometimes pick up abnormal vaginal cells as well. Adhering to your doctor's recommended screening schedule is vital.
Conclusion: Knowledge is Your Best Defence
Vaginal cancer may be rare, but its impact is profound. By understanding the interplay of age, HPV infection, historical exposures, and lifestyle, you move from a position of uncertainty to one of empowered awareness. This guide has outlined that while some factors like age or DES exposure are beyond our control, many of the most significant risks are manageable. Getting vaccinated against HPV, avoiding smoking, and committing to regular gynaecological check-ups are powerful actions within your reach. Early detection dramatically improves treatment outcomes. Listen to your body, maintain open communication with your healthcare provider, and use this knowledge as your first line of defence. Your health journey is ongoing, and being informed is the most important step you can take.
Consult a Gynaecologic Oncologist for the best advice
Consult a Gynaecologic Oncologist for the best advice

Dr. Sai Lakshmi Daayana
Gynaecological Oncologist
18 Years • MBBS, MRCOG
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
(225+ Patients)

Dr. Revathi S Rajan
Obstetrician and Gynaecologist
24 Years • MBBS, DGO, DNB.FFMM
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Sreeparna Roy
Obstetrician and Gynaecologist
8 Years • MBBS , MS (OBSTETRICS & GYNAECOLOGY), Fellowship in Infertility, Endoscopy & Ultrasonography), Fellowship in Laparoscopy & Hysteroscopy,DRM
Kolkata
Dr Utsa Basu Clinic, Kolkata
Dr. B Shravanthi Reddy
Radiation Specialist Oncologist
8 Years • MBBS, DNB(Radiation Oncology)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir

Dr. Sushith C
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru
Consult a Gynaecologic Oncologist for the best advice

Dr. Sai Lakshmi Daayana
Gynaecological Oncologist
18 Years • MBBS, MRCOG
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
(225+ Patients)

Dr. Revathi S Rajan
Obstetrician and Gynaecologist
24 Years • MBBS, DGO, DNB.FFMM
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Sreeparna Roy
Obstetrician and Gynaecologist
8 Years • MBBS , MS (OBSTETRICS & GYNAECOLOGY), Fellowship in Infertility, Endoscopy & Ultrasonography), Fellowship in Laparoscopy & Hysteroscopy,DRM
Kolkata
Dr Utsa Basu Clinic, Kolkata
Dr. B Shravanthi Reddy
Radiation Specialist Oncologist
8 Years • MBBS, DNB(Radiation Oncology)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir

Dr. Sushith C
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru
More articles from Vaginal Cancer
Frequently Asked Questions
1. What are the early warning signs of vaginal cancer?
Early-stage vaginal cancer may not cause symptoms. When symptoms do occur, they can include abnormal vaginal bleeding (after menopause or between periods), unusual vaginal discharge, a palpable lump in the vagina, painful urination, or pelvic pain. It's important to note these symptoms are more often caused by other, less serious conditions, but they should always be evaluated by a doctor.
2. If I've had the HPV vaccine, am I completely protected from vaginal cancer?
The HPV vaccine is highly effective at protecting against the specific high-risk HPV strains that cause about 70-90% of vaginal cancers. However, it does not protect against all strains or other risk factors. It should be seen as a crucial layer of protection within a broader strategy that includes regular screenings.
3. Is vaginal cancer hereditary?
Most cases of vaginal cancer are not directly hereditary. The primary risk factors are related to HPV infection and environmental exposures. However, there may be a very slight increased risk if you have a strong family history of gynaecologic cancers, but this is not common.
4. How is VAIN different from vaginal cancer?
VAIN (Vaginal Intraepithelial Neoplasia) is a pre-cancerous condition where abnormal cells are confined to the surface layer of the vagina. Invasive vaginal cancer means the abnormal cells have broken through this surface layer and can spread deeper into vaginal tissues and to other parts of the body. VAIN is considered a precursor that can be treated to prevent cancer.
5. Can a Pap test detect vaginal cancer?
A Pap test is primarily designed to screen for cervical cancer. However, during the test, cells are collected from the cervix and sometimes from the upper vagina. While it's not a reliable screening tool for vaginal cancer, it can occasionally detect abnormal vaginal cells, leading to further investigation.