Alcohol-Related Liver Diseases: Risk, Signs, and Care
Know all about the alcohol-related liver diseases, what it is, stages of ARLD, risks, signs, symptoms and causes. Learn about the diagnosis and treatment options.

Written by Dr. Md Yusuf Shareef
Reviewed by Dr. D Bhanu Prakash MBBS, AFIH, Advanced certificate in critical care medicine, Fellowship in critical care medicine
Last updated on 13th Jan, 2026

Introduction
Alcohol-related liver diseases are among the most preventable causes of serious illness worldwide, yet they’re rising in younger adults and women. If you or someone you love drinks regularly, understanding the real risk to the liver can be a life-changing step. This guide demystifies the topic in plain language: how alcohol injures the liver, the stages of disease, who is most at risk, and what symptoms to watch for. You’ll also learn how doctors diagnose alcohol-related liver diseases, the treatments that truly help, and practical ways to reduce harm, whether you choose to cut back or quit. If you need support, we’ll point you to options for online care and home testing that make getting help easier. Read on for a clear, compassionate guide to diseases of the liver related to alcohol and how to take control of your risk.
What Are Alcohol-Related Liver Diseases (ARLD)?
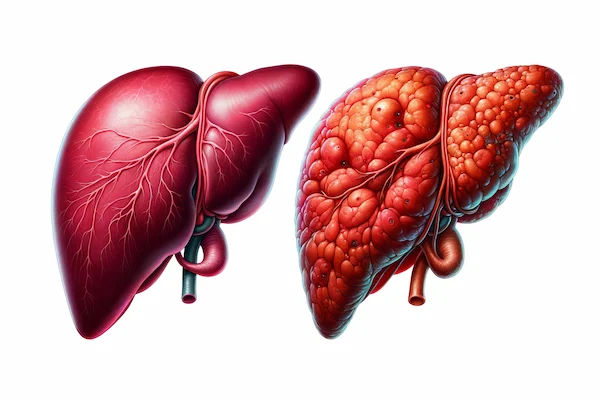
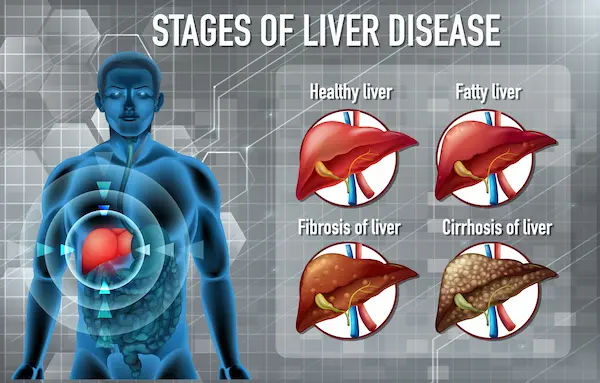
Alcohol-related liver disease (ARLD) is a spectrum of liver damage caused by alcohol, from simple fat build-up (fatty liver) to inflammation (alcoholic hepatitis), scarring (fibrosis), cirrhosis, and even liver cancer. Many people with early ARLD feel fine, which is why screening and awareness are crucial. The earlier it’s found, the more reversible it is.
Consult a Top Hepatologist for Personalised Advice
Why ARLD matters now: trends and who is affected
Alcohol is a leading cause of preventable liver-related deaths globally. Rates of alcoholic hepatitis and cirrhosis have risen in recent years, including during and after the COVID-19 pandemic, especially among younger adults and women. While any drinking increases health risk, heavier patterns like daily heavy drinking or frequent binge episodes dramatically raise liver risk. A practical insight: liver risk comes not only from “how much” you drink overall, but also “how you drink” (bingeing, lack of alcohol-free days) and “what else” is going on (obesity, viral hepatitis, genetics).
How Alcohol Damages the Liver
The damage to the liver involves:
From metabolism to inflammation
The liver breaks down alcohol into acetaldehyde, a toxic molecule that triggers oxidative stress and inflammation. Repeated exposure leads to fat accumulation (steatosis), immune activation, and eventually cell death and scarring. In lab and clinical studies, typical blood patterns in alcohol-related injury include an AST-to-ALT ratio greater than 2 and elevated GGT, reflecting both hepatocyte injury and enzyme induction [3][4]. Over time, the liver’s ability to regenerate is overwhelmed.
The role of the gut microbiome and nutrition
Alcohol alters the gut barrier and microbiome, allowing bacterial products (endotoxins) to reach the liver and amplify inflammation. Poor diet compounds risk; protein-calorie malnutrition and vitamin deficiencies (especially thiamine, folate) are common in alcohol use disorder (AUD) and worsen outcomes. Unique insight: improving gut health (adequate protein, fibre, and micronutrients) and correcting deficiencies can meaningfully reduce inflammation and support liver repair alongside alcohol cessation, an often underemphasized pillar of care.
Stages of ARLD
The stages are divided as
Alcoholic fatty liver (steatosis): reversible changes
Fatty liver is the earliest stage, often detected on ultrasound or by elevated liver enzymes. The good news: it’s usually reversible within weeks of abstinence. Even reductions in drinking can help, but complete alcohol cessation leads to the fastest improvements in liver fat and enzyme levels. Long-tail keyword: alcoholic fatty liver reversible.
Alcoholic hepatitis: inflammation and acute injury
Alcoholic hepatitis is a potentially life-threatening flare of inflammation. Symptoms can include jaundice, fever, abdominal pain, and weakness. Hospitalisation is common; mortality can be high in severe cases. Doctors use severity scores such as Maddrey’s Discriminant Function to decide on treatments like corticosteroids; the Lille score after 7 days helps determine response. Long-tail keywords: alcoholic hepatitis symptoms and treatment, Maddrey discriminant function.
Fibrosis and cirrhosis: scarring and complications
With ongoing drinking, inflammation leads to scarring (fibrosis) and eventually cirrhosis, where the liver becomes nodular and stiff. Complications can include ascites, variceal bleeding, hepatic encephalopathy, and increased infection risk. Even at this stage, abstinence improves survival, reduces complications, and may partly reverse fibrosis in some people.
Liver cancer (HCC) risk in ARLD
Cirrhosis from alcohol increases the risk of hepatocellular carcinoma (HCC). Surveillance (ultrasound with or without AFP every 6 months) is recommended for people with cirrhosis to catch cancer early, when curative treatments are possible.
Who Is at Highest Risk?
The risk is understood in the following ways:
Quantity, pattern, and duration of drinking
Risk rises with the total amount of alcohol consumed over time (cumulative dose) and with patterns like daily heavy drinking or binge drinking (for example, ≥5 drinks for men or ≥4 for women on one occasion). Some research suggests cirrhosis risk increases notably once average daily intake exceeds about 3 drinks in men and 2 in women, but importantly, WHO emphasises no level is completely risk-free.
Sex differences, genetics (PNPLA3), and co-morbidities
Women develop ARLD at lower alcohol doses than men, partly due to differences in alcohol metabolism. Genetics matter: variants like PNPLA3 (I148M) increase susceptibility to liver fat and scarring when combined with alcohol, though genetic testing isn’t routinely needed. Co-morbid conditions like metabolic syndrome or type 2 diabetes amplify risk.
Obesity, viral hepatitis, and smoking
Excess body fat and alcohol act synergistically, accelerating liver injury. Co-infection with hepatitis B or C raises the risk of cirrhosis and liver cancer. Smoking worsens outcomes and increases HCC risk [3][4]. Unique insight: treating metabolic syndrome (dietary pattern, weight reduction, physical activity) can reduce alcohol-related liver stress even before full abstinence is achieved.
Signs and Symptoms to Watch
The signs and symptoms to look out for include:
Early, subtle signs vs. urgent red flags
Early ARLD may cause fatigue, poor sleep, right upper abdominal discomfort, or mild enzyme elevations. Red flags needing urgent evaluation include jaundice (yellowing eyes/skin), severe abdominal swelling, vomiting blood or black stools, confusion, fever with abdominal pain, or rapid weight loss. Long-tail keyword: alcoholic cirrhosis life expectancy (discussed below).
When to see a doctor
If you have any persistent symptoms (fatigue, abdominal pain, nausea) or drink heavily, it’s wise to get checked. If symptoms persist beyond two weeks, consult a doctor online with Apollo24|7 for further evaluation. Emergency symptoms like vomiting blood, severe jaundice, or confusion require immediate medical attention.
How ARLD Is Diagnosed
Blood tests (AST/ALT, GGT, bilirubin) and what they mean
Doctors start with liver function tests (LFTs): AST, ALT, alkaline phosphatase, GGT, bilirubin, albumin, and clotting (INR). Alcohol-related patterns often show AST higher than ALT (often AST/ALT >2) and elevated GGT; bilirubin and INR can signal severity. Other helpful tests include CBC (macrocytosis), ferritin, and viral hepatitis screening. Apollo24|7 offers convenient home collection for tests like LFTs, making it easier to start screening if getting to a clinic is hard.
Imaging (ultrasound, FibroScan) and non-invasive scores (FIB-4)
1. Ultrasound can detect fatty liver, nodularity, and ascites.
2. Transient elastography (FibroScan) measures liver stiffness, helping estimate fibrosis without a biopsy.
3. Non-invasive scores like FIB-4 (uses age, AST, ALT, platelet count) help triage who needs speciality referral.
Get Your Symptoms Assessed
When a biopsy is considered
A liver biopsy provides a definitive diagnosis when uncertainty remains (e.g., distinguishing alcoholic hepatitis from other causes) or when decisions about treatments like steroids hinge on the findings. It’s not required for every patient.
Treatment: What Works, What Doesn’t
What should be done and shouldn't be done, includes:
Abstinence and harm reduction
Complete alcohol abstinence is the most effective treatment at every stage, improving survival and stabilising or reversing damage. If abstinence feels out of reach, harm reduction steps (more alcohol-free days, avoiding binges, switching to lower-alcohol options) still reduce risk. Unique insight: schedule “alcohol-free experiments” of 2–4 weeks; people are often encouraged by how quickly sleep, mood, and LFTs improve.
Nutrition, vitamins, and managing deficiencies
Aim for 1.2–1.5 g/kg/day of protein (unless otherwise advised), a Mediterranean-style dietary pattern, and correction of deficiencies. Thiamine (vitamin B1) should be given before glucose in anyone at risk to prevent Wernicke’s encephalopathy. Folate, magnesium, and vitamin D are commonly low in people with AUD. Apollo24|7 offers home collection for tests like vitamin D if your clinician recommends them.
Medications for alcohol use disorder (AUD): what’s safe in liver disease
1. Naltrexone and acamprosate are first-line; naltrexone is generally avoided in acute hepatitis or advanced liver failure.
2. A camprosate is renally cleared and often preferred when liver function is impaired.
3. Baclofen has evidence for reducing alcohol intake and is considered safer in advanced liver disease; it’s used off-label in many settings.
4. Disulfiram is generally avoided in significant liver disease. Gabapentin or topiramate may help as adjuncts.
If your condition does not improve after trying these methods, book a physical visit to a doctor with Apollo24|7 for a personalised plan.
Special Focus: Alcoholic Hepatitis and Advanced Cirrhosis
Severity scoring (Maddrey, MELD, Lille) and steroids
Severe alcoholic hepatitis carries high short-term mortality. The Maddrey Discriminant Function (DF ≥32) and MELD score guide treatment, including trial of corticosteroids after ruling out active infection and gastrointestinal bleeding. The Lille score after 7 days assesses response; if poor, steroids are discontinued. Long-tail keywords: Lille score alcoholic hepatitis.
Managing complications and transplant pathways
Complications include ascites (managed with diuretics and salt restriction), variceal bleeding (endoscopy and beta-blockers), encephalopathy (lactulose, rifaximin), and infections (low threshold for antibiotics). Early involvement of a transplant centre is important for select patients; strict abstinence support and psychosocial evaluation are key. Notably, many programs no longer require a fixed “6-month sobriety” for listing; decisions are individualised. Unique insight: building a documented recovery support plan (therapy attendance, peer support, family involvement) can strengthen transplant candidacy and outcomes.
Prevention and Lower-Risk Drinking
The things to prevent and lower the risk of drinking include:
How much is too much? Understanding limits
Public health guidance varies, but the trend is clear: there’s no completely safe level of alcohol for health, and lower is better for liver risk. Traditional “low-risk” thresholds (e.g., up to 2 standard drinks/day for men and 1 for women) should not be seen as guarantees of safety, especially if you have additional risk factors (obesity, viral hepatitis). Avoid binge drinking, build several alcohol-free days weekly, and track intake honestly.
Vaccinations, coffee, and lifestyle supports
Vaccinate against hepatitis A and B if not immune.
Coffee consumption (2–3 cups/day) has been associated with a lower risk of chronic liver disease progression in observational studies; it’s not a cure, but it may be a helpful adjunct.
Exercise, sleep, and stress management reduce relapse risk and support liver health.
Screening and Getting Help
The screening and getting help include:
AUDIT-C screening and brief interventions
The AUDIT-C is a 3-question screen you can complete in minutes; it helps identify risky drinking. Brief counselling and goal-setting can reduce intake significantly. Biomarkers like CDT or PEth may be used in some settings when accurate detection of alcohol use is essential.
Therapy options (CBT, mutual-help groups), family involvement
Cognitive-behavioural therapy, motivational interviewing, and contingency management all help. Mutual-help groups (AA, SMART Recovery) are accessible and can be combined with medical care. Family coaching improves outcomes by supporting accountability and reducing triggers. If you’re ready to talk to a professional, consult a doctor online with Apollo24|7 to discuss screening, medications, and referral pathways.
Life After Diagnosis: Monitoring and Recovery
Timeline of improvement after quitting alcohol
1. Days 3–7: Sleep improves; tremors and cravings ease. LFTs may start trending down.
2. Weeks 2–4: Steatosis often improves on imaging; energy and mood are more stable.
3. 3–6 months: Fibrosis stabilisation or partial regression in some; weight and metabolic markers often improve.
4. 1–2 years: Significant survival benefit becomes apparent; cirrhosis complications may reduce with sustained abstinence.
Follow-up tests and imaging schedule
Your clinician may repeat LFTs in 4–8 weeks, then every 3–6 months, and use FibroScan/ultrasound to track fibrosis or cirrhosis. If you have cirrhosis, HCC surveillance with ultrasound every 6 months is typical.
Myths vs. Facts
Beer vs. spirits, “detoxes,” and “liver cleanses”
1. Myth: “Beer is safer than spirits.” Fact: Standard drinks contain similar alcohol; total ethanol dose drives risk.
2. Myth: “A monthly detox undoes daily drinking.” Fact: The liver cares about cumulative dose and pattern; frequent binges are especially harmful.
3. Myth: “Liver cleanse supplements fix damage.” Fact: No supplement reverses scarring; abstinence, nutrition, and medical care do.
Conclusion
Alcohol-related liver diseases are common, serious, and largely preventable. Whether you’re just beginning to question your drinking or you’ve already been told you have fatty liver, alcoholic hepatitis, or cirrhosis, the most powerful step you can take is to reduce or stop alcohol. Your liver is remarkably resilient: in many cases, steatosis clears within weeks and inflammation quiets over months, especially when you pair abstinence with good nutrition and medical care. Remember that risk depends not just on quantity, but on pattern and personal factors like sex, obesity, and co-existing conditions. Screening is simple, often starting with a few questions and basic blood tests; imaging like FibroScan can refine the picture without a biopsy. If symptoms persist beyond two weeks or you’re worried about your drinking, consult a doctor online with Apollo24|7 for tailored advice, referrals, and medication options. If your clinician orders tests, Apollo24|7 offers convenient home collection for LFTs and other labs, which can help you get started sooner.
Consult a Top Hepatologist for Personalised Advice
Consult a Top Hepatologist for Personalised Advice

Dr. Pavan Kumar Y M
Gastroenterology/gi Medicine Specialist
5 Years • MBBS, MD Medicine, DM Gastroenterology
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(150+ Patients)
Dr Pradeep Krishna R V
Hepatologist
16 Years • MBBS,MS (General Surgery),MCh (Surgical Gastroenterology),Fellowship in Liver Transplant and HPB Surgery
Bengaluru
Apollo Hospitals Bannerghatta Road, Bengaluru

Dr. Aakash Garg
Gastroenterology/gi Medicine Specialist
12 Years • MBBS, DNB (Medicine), DrNB (Gastroentrology).
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur
(150+ Patients)

Prof. Dr. Kanhu Charan Das
Gastroenterology/gi Medicine Specialist
24 Years • MBBS, MD (Medicine) DM (Gastroenterology & Hepatology, CMC, Vellore). Advanced Proceduralist (ERCP, EUS, POEM & ESD) Senior Consultant - Gastroenterologist.
Bhubaneswar
Apollo Hospitals Old Sainik School Road, Bhubaneswar
(325+ Patients)
Consult a Top Hepatologist for Personalised Advice

Dr. Pavan Kumar Y M
Gastroenterology/gi Medicine Specialist
5 Years • MBBS, MD Medicine, DM Gastroenterology
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(150+ Patients)
Dr Pradeep Krishna R V
Hepatologist
16 Years • MBBS,MS (General Surgery),MCh (Surgical Gastroenterology),Fellowship in Liver Transplant and HPB Surgery
Bengaluru
Apollo Hospitals Bannerghatta Road, Bengaluru

Dr. Aakash Garg
Gastroenterology/gi Medicine Specialist
12 Years • MBBS, DNB (Medicine), DrNB (Gastroentrology).
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur
(150+ Patients)

Prof. Dr. Kanhu Charan Das
Gastroenterology/gi Medicine Specialist
24 Years • MBBS, MD (Medicine) DM (Gastroenterology & Hepatology, CMC, Vellore). Advanced Proceduralist (ERCP, EUS, POEM & ESD) Senior Consultant - Gastroenterologist.
Bhubaneswar
Apollo Hospitals Old Sainik School Road, Bhubaneswar
(325+ Patients)
More articles from Alcoholic Liver Disease
Frequently Asked Questions
1) Is alcoholic fatty liver reversible?
Yes. In most people, fatty liver from alcohol improves within weeks of abstinence and healthy nutrition. Even cutting back reduces risk, but quitting provides the fastest reversal. Long-tail keyword: alcoholic fatty liver reversible.
2) What blood tests suggest alcohol-related liver disease?
LFTs showing AST higher than ALT (often a ratio >2), elevated GGT, and increased bilirubin or INR can suggest alcohol-related injury. Your doctor may also use FIB-4 to estimate fibrosis. Long-tail keywords: AST ALT ratio alcohol, GGT high alcohol causes.
3) How is fibrosis checked without a biopsy?
Non-invasive tools like FIB-4 scoring and FibroScan (transient elastography) estimate scarring. Many people avoid a biopsy unless the results would change treatment. Long-tail keyword: FibroScan for liver fibrosis.
4) What medications help me stop drinking if I have liver disease?
Acamprosate is often preferred with significant liver impairment. Baclofen can help reduce alcohol intake and is considered safer in advanced disease. Discuss naltrexone risks/benefits with your doctor. If your condition does not improve, book a physical visit to a doctor with Apollo24|7.
5) Are there safe alcohol limits for my liver?
There’s no completely safe level. Lower is better, especially if you have added risks (obesity, hepatitis B/C). Avoid binge drinking and plan alcohol-free days each week. Long-tail keyword: safe alcohol limits for liver health.