What Leads To Signs Of Diabetes And Types
Discover the different types of diabetes, their warning signs, causes, and diagnosis methods. Learn how to identify symptoms early and manage the condition effectively.


Introduction
Diabetes is a word we hear often, but its reality is far more complex than just "high blood sugar." It's a multifaceted metabolic disorder affecting how your body turns food into energy, impacting millions globally. Understanding the signs of diabetes is the first critical step towards proactive health management. This condition isn't monolithic; it manifests in different forms, primarily Type 1 and Type 2 diabetes, each with distinct causes and characteristics. Are you experiencing unusual thirst, frequent trips to the bathroom, or unexplained fatigue? These could be more than just passing quirks, they might be your body's early warning signals. This article will demystify the different types of diabetes, decode their tell-tale symptoms, explore their root causes, and empower you with the knowledge to take the next steps. Let's unravel the complexities of this condition together.
What Exactly Is Diabetes?
Diabetes mellitus, commonly known as diabetes, is a chronic health condition that occurs when your body cannot effectively manage the level of sugar (glucose) in your blood. Glucose is vital for health as it's a primary source of energy for the cells that make up your muscles and tissues. It's also your brain's main fuel source. The problem arises when this glucose builds up in your bloodstream instead of being efficiently transported into your cells.
The Role of Insulin and Glucose
Think of your body as a car and glucose as its fuel. For this fuel to enter the cells and power the engine, it needs a key. That key is a hormone called insulin, produced by the beta cells in the pancreas. After you eat, your digestive system breaks down carbohydrates into glucose, which enters your bloodstream. In response, your pancreas releases insulin. Insulin unlocks your cells, allowing glucose to enter and be used for energy. In diabetes, this process breaks down. Either the pancreas doesn't produce enough (or any) insulin, or the body's cells become resistant to insulin's effects. In both cases, the result is the same: glucose remains trapped in the blood.
The Common Thread: Hyperglycaemia
This state of having too much glucose circulating in your blood is called hyperglycaemia. Chronic hyperglycaemia, the hallmark of all types of diabetes, is what leads to the common symptoms and, if unmanaged, can cause serious damage to nerves, blood vessels, and organs over time.
Unveiling the Different Types of Diabetes
While high blood sugar is a universal feature, the reasons behind it differ significantly, leading to several types of diabetes.
Type 1 Diabetes: The Autoimmune Response
Type 1 diabetes is an autoimmune condition. This means the body's own immune system, which normally fights
harmful viruses and bacteria, mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. The result is a severe lack of insulin. People with Type 1 diabetes require lifelong insulin therapy via injections or a pump to survive. It accounts for about 5-10% of all diabetes cases and often, but not always, appears in childhood or adolescence.
Who is at Risk for Type 1 Diabetes?
The exact cause is unknown, but it's believed to involve a combination of genetic predisposition and an environmental trigger, such as a virus. Unlike Type 2 diabetes, it is not linked to lifestyle or weight.
Type 2 Diabetes: The Insulin Resistance Epidemic
Type 2 diabetes is the most common form, representing about 90-95% of cases. Here, the body doesn't use insulin properly—a condition known as insulin resistance. Initially, the pancreas makes extra insulin to compensate, but over time, it can't keep up and insulin production decreases. This leads to a gradual build-up of glucose in the blood. Type 2 diabetes can develop at any age, though it most commonly occurs in middle-aged and older adults.
Key Risk Factors for Developing Type 2 Diabetes
- Weight: Being overweight is a primary risk factor.
- Inactivity: Physical activity helps control weight and uses glucose for energy.
- Family History: Risk increases if a parent or sibling has it.
- Age: Risk increases after age 45.
- Prediabetes: A condition where blood sugar is high but not yet high enough for a Type 2 diabetes diagnosis.
Gestational Diabetes, During Pregnancy
This type develops during pregnancy in women who didn't previously have diabetes. Hormones produced by the
placenta can make the mother's cells more resistant to insulin. Usually, the pancreas responds by producing enough extra insulin to overcome this resistance. But sometimes, it can't, leading to gestational diabetes. It typically resolves
after the baby is born, but it increases the mother's future risk of developing Type 2 diabetes.
Other Types, Prediabetes and Beyond
Prediabetes is a serious health condition where blood sugar levels are higher than normal, but not high enough yet to be diagnosed as Type 2 diabetes. It's a critical warning sign. Other, rarer types of diabetes include monogenic diabetes (caused by a single gene mutation) and diabetes related to cystic fibrosis or pancreatic surgery.
Decoding the Warning Signs: What Your Body is Telling You
Recognising the early signs of diabetes is crucial for early intervention. Many symptoms are shared, but their onset can
differ.
Consult a Specialist for the best advice
Early Signs and Symptoms Common to Most Types
These classic symptoms are primarily caused by hyperglycaemia.
- Polyuria (Frequent Urination): The kidneys work overtime to filter and absorb excess sugar. When they can't keep up,
the sugar is excreted into your urine, dragging fluids from your tissues, leading to frequent urination. - Polydipsia (Extreme Thirst): As you lose more fluids, you become dehydrated, leading to intense thirst.
- Polyphagia (Increased Hunger): Without enough insulin to move sugar into your cells, your muscles and organs
become depleted of energy, triggering intense hunger. - Unexplained Weight Loss: Despite eating more, you may lose weight. Without the ability to metabolise glucose, the
body uses alternative energy stored in muscle and fat, burning it off quickly. - Fatigue: When your cells are deprived of sugar, you can become tired and irritable.
- Blurred Vision: High blood sugar can pull fluid from the lenses of your eyes, affecting their ability to focus.
Symptoms More Specific to Type 1 Diabetes
These symptoms often develop very quickly, over weeks or even days. The weight loss can be severe and sudden.
Symptoms and Indicators of Type 2 Diabetes
These symptoms of Type 2 diabetes often develop much more slowly, over years. Many people have no symptoms at allfor a long period.
- Slow-Healing Sores or Frequent Infections: High blood sugar impairs blood flow and the body's natural healing process.
- Areas of Darkened Skin: A condition called acanthosis nigricans, often in the armpits and neck, can be a sign of insulin
resistance. - Tingling, Numbness, or Pain in Hands/Feet (Neuropathy): This is caused by nerve damage from prolonged high blood
sugar.
Recognising Gestational Diabetes
Gestational diabetes often has no noticeable symptoms. This is why screening tests between 24 and 28 weeks of
pregnancy are standard practice for most pregnant women.
What Causes Diabetes? The Triggers Behind the Types
The Cause of Type 1 Diabetes: A Mystery Trigger
The exact causes of Type 1 diabetes remain unknown. It is primarily believed to be an autoimmune disorder where
genetics play a role, but an environmental trigger (like a virus) is thought to initiate the immune system's attack on the
pancreas.
The Causes of Type 2 Diabetes: Lifestyle and Genetics
Type 2 diabetes is caused by a combination of factors:
- Genetics and Family History: Your genes can make you more susceptible.
- Lifestyle: This is the major modifiable factor. Being overweight, especially with abdominal fat, and being physically
inactive are primary drivers of insulin resistance. - Cell Signalling: In Type 2 diabetes, fat, liver, and muscle cells often respond incorrectly to insulin because of
dysfunction in their internal signalling pathways.
How is Diabetes Diagnosed?
If you're experiencing potential signs of diabetes, it's essential to see a doctor for proper testing. Self-diagnosis is not safe.
If your symptoms are persistent, consult a doctor online with Apollo24|7 for further evaluation and to order the
necessary tests.
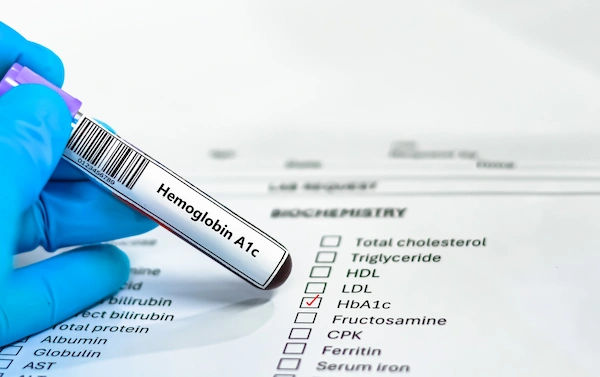
Common Blood Tests for Diabetes
- A1C Test: Measures your average blood sugar level over the past 2-3 months. An A1C level of 6.5% or higher on two
separate tests indicates diabetes. - Fasting Blood Sugar Test: A blood sample is taken after an overnight fast. A level of 126 mg/dL or higher suggests
diabetes. - Oral Glucose Tolerance Test (OGTT): Your blood sugar is tested after fasting and then again two hours after drinking a
sugary liquid. A reading of 200 mg/dL or higher indicates diabetes.
Conclusion
Understanding the distinct types of diabetes and their unique warning signs empowers you to be an active participant in
your health journey. While a diagnosis can feel daunting, it is also the first step towards effective management and a
full, healthy life. Remember, symptoms like unquenchable thirst or persistent fatigue are your body's signals, paying
attention to them is paramount. Whether it's the autoimmune origin of Type 1 or the lifestyle-influenced Type 2
diabetes, modern medicine offers numerous strategies for management, from insulin therapy to dietary changes and
medication. If anything you've read here resonates with your own experience, don't wait. Take action today by
consulting a healthcare professional on Apollo24|7 to discuss your concerns and get accurate testing. Knowledge is
indeed the most powerful tool in navigating and managing diabetes.
Consult a Specialist for the best advice
Consult a Specialist for the best advice

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Ashita Kuruvilla
General Practitioner
7 Years • MBBS
Kolkata
KVC CLINIC, Kolkata

Dr. Sougata Kumar
General Practitioner
8 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Arthi S
Family Physician
3 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr Syed Mateen Pasha
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru
Consult a Specialist for the best advice

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Ashita Kuruvilla
General Practitioner
7 Years • MBBS
Kolkata
KVC CLINIC, Kolkata

Dr. Sougata Kumar
General Practitioner
8 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Arthi S
Family Physician
3 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr Syed Mateen Pasha
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru
More articles from Diabetes
Frequently Asked Questions
Can you suddenly become diabetic?
Yes, particularly with Type 1 diabetes, symptoms can appear very suddenly over a few weeks. However, Type 2 diabetes usually develops gradually over years. The sudden onset of severe symptoms requires immediate medical attention.
What are the first signs of being diabetic?
The most common first signs of diabetes are the 'three Polys': Polyuria (frequent urination), Polydipsia (extreme thirst), and Polyphagia (increased hunger). Unexplained weight loss and blurred vision are also strong early indicators.
What is the main cause of diabetes?
The main cause depends on the type. Type 1 diabetes is caused by an autoimmune reaction that destroys insulin-producing cells. The main cause of Type 2 diabetes is a combination of genetics and lifestyle factors that lead to insulin resistance, with obesity and physical inactivity being major contributors.
Can diabetes be cured?
Currently, there is no cure for Type 1 diabetes, and it requires lifelong insulin management. Type 2 diabetes is a manageable condition. It can often be controlled so effectively with lifestyle changes, medication, and weight loss that blood sugar levels return to a non-diabetic range, effectively putting the disease into 'remission,' but the underlying tendency remains.
What is the difference between Type 1 and Type 2 diabetes?
The key difference is the mechanism. Type 1 is an autoimmune condition where the body produces no insulin. Type 2 is a metabolic condition where the body doesn't use insulin properly (insulin resistance) and eventually may not produce enough. Type 1 is not preventable and often starts in youth; Type 2 is largely preventable and linked to lifestyle and age.