Guide to Awareness About Liver Disease
Learn the essentials of liver disease awareness: symptoms, causes, risk factors, prevention, diagnosis, and treatment options. Know when to get tested, how to protect your liver, and what lifestyle changes truly make a difference. Take control of your liver health with expert-backed guidance.


Introduction
Your liver is a powerhouse—processing nutrients, filtering toxins, aiding digestion, regulating blood sugar, and supporting immunity every hour of the day. Yet liver disease commonly develops in silence, with little to no symptoms until substantial damage has already occurred. That is why being aware of risk factors, lifestyle influences, and early warning signs matters so much.
This guide simplifies the most important aspects of liver health so you can recognise problems early, prevent progression, and ask informed questions in medical appointments. We’ll explore common liver conditions, symptoms, diagnosis, advanced complications, treatment strategies, and practical lifestyle measures.
With everyday actions—such as safe alcohol habits, a nutrient-rich diet, exercise, weight management, and appropriate vaccinations—you can guard your liver for the long term. If symptoms persist beyond two weeks or concerns arise, you can consult a doctor online with Apollo 24|7 for timely guidance, and arrange home sample collection for liver function tests (LFTs) if needed.
Consult a Top Hepatologist for Personalised Advice
Understanding Liver Disease: What Your Liver Does and Why It Matters
Your liver supports digestion, detoxification, immunity, energy regulation, and blood-clotting — so damage can affect
health from head to toe.
What the liver does every day
- Produces bile to break down fats
- Filters toxins, alcohol, and by-products from blood
- Regulates glucose and stores vitamins and minerals
- Metabolises medicines and hormones
- Produces essential proteins such as albumin and clotting factors
What is liver disease?
“Liver disease” describes any condition that damages liver cells, disrupts function, or leads to inflammation and
scarring.
- Acute liver damage: sudden, usually reversible
- Chronic liver disease: long-term inflammation leads to fibrosis, then cirrhosis
- Cirrhosis: advanced scarring with serious complications, including liver failure and cancer
Many people feel completely well during early disease, so risk-based screening and lifestyle protection are essential.
Types of Liver Disease: The Major Categories
Different causes require different treatments, so recognising the category is critical.
Viral Hepatitis
Infections that cause liver inflammation.
Hepatitis A and E
Spread through contaminated food or water; usually short-term but can be severe in vulnerable individuals.
Vaccination protects against Hepatitis A.
Hepatitis B and C
Spread through blood and bodily fluids; may become chronic and lead to cirrhosis or liver cancer.
Hepatitis B vaccine prevents infection; Hepatitis C is now curable in most cases.
Metabolic Fatty Liver Disease (MASLD/MASH)
Associated with obesity, type 2 diabetes, high triglycerides, and insulin resistance.
About one in four adults is affected, often unknowingly.
Alcohol-Related Liver Disease (ARLD)
Ranging from fatty liver to hepatitis and cirrhosis, driven by quantity, pattern, and duration of alcohol use.
Autoimmune Liver Diseases
The immune system targets liver tissue or bile ducts.
Examples: Autoimmune hepatitis, Primary Biliary Cholangitis (PBC), Primary Sclerosing Cholangitis (PSC).
Genetic/Inherited Liver Disorders
Conditions affecting iron, copper, or protein processing such as:
- Haemochromatosis (iron overload)
- Wilson’s disease (copper accumulation)
- Alpha-1 antitrypsin deficiency
Cholestatic and Biliary Disorders
Reduced or blocked bile flow causes itching, jaundice, and vitamin deficiencies.
Liver Cancer (Hepatocellular Carcinoma — HCC)
Usually develops after years of chronic liver disease or cirrhosis.
People may have overlapping risks — for example, alcohol use plus diabetes significantly accelerates liver damage.
Early Signs and Symptoms You Shouldn’t Ignore
Symptoms often appear late — noticing subtle changes can lead to earlier intervention.
Common early symptoms
- Persistent fatigue
- Right upper-side abdominal discomfort
- Nausea or appetite loss
- Unexplained itching
- Dark urine, pale stools
- Easy bruising
Advanced warning signs (urgent)
- Jaundice (yellow eyes/skin)
- Swollen legs/abdomen (ascites)
- Vomiting blood or black stools
- Confusion or irritability (possible encephalopathy)
If symptoms persist beyond two weeks or risk factors apply, consult a doctor online with Apollo 24|7 for screening.
Causes and Risk Factors
Most liver disease is linked to modifiable behaviours — small improvements bring big benefits.
Major risk contributors
- Metabolic syndrome: abdominal fat, high sugar, high triglycerides, hypertension
- Alcohol consumption, especially binge patterns
- Viral hepatitis exposure
- Medications: excessive paracetamol, some antibiotics, antifungals and herbal supplements
- Environmental toxins
- Genetic disorders
- Autoimmune tendencies
Even mild alcohol use combined with metabolic risks escalates damage faster than either alone.
How Liver Disease Is Diagnosed
Timely testing allows for early action — often before symptoms occur.
Blood tests (LFTs and related)
- ALT, AST – enzyme levels rise with injury
- Bilirubin – jaundice marker
- Alkaline Phosphatase & GGT – bile duct markers
- Albumin & INR – liver synthetic function
- Platelets – lower counts suggest advanced fibrosis
Imaging
- Ultrasound for fatty change, masses, and fluid
- FibroScan (Elastography) to assess stiffness (fibrosis) and fat
Non-invasive fibrosis scores
Tools like FIB-4 estimate the risk of scarring and guide referrals.
Liver biopsy
Used only when diagnosis or staging remains unclear.
Apollo 24|7 offers home test booking for LFTs, hepatitis screening and metabolic markers convenient for those starting
evaluation.
Complications of Chronic Liver Disease
Early intervention prevents irreversible harm.
Potential consequences
- Cirrhosis – advanced scarring
- Portal hypertension – high vein pressure leading to varices
- Ascites – abdominal fluid buildup
- Bleeding risks – fragile swollen veins
- Hepatic encephalopathy – confusion from toxin build-up
- Hepatocellular carcinoma – liver cancer
Routine surveillance, including ultrasound every 6 months in at-risk individuals, enables earlier cancer detection and life-saving treatment.
Prevention and Lifestyle: Everyday Changes that Protect the Liver
Small daily choices have long-term protective effects — especially before fibrosis develops.
Weight and waist control
A 7–10% reduction in body weight can reverse fatty liver changes and improve inflammation.
Beneficial diet pattern — Mediterranean style
- Fruits, vegetables, legumes
- Whole grains and nuts
- Olive oil as the primary fat
- Fish and lean proteins
Limit sugary drinks, snack foods, red/processed meats, and deep-fried items.
Physical activity
Aim for:
- 150–300 mins/week moderate exercise
- 2 days/week strength training
Movement reduces liver fat even without weight loss.
Alcohol awareness
Those with fatty liver or hepatitis should avoid alcohol entirely.
Vaccination & infection prevention
Vaccines for Hepatitis A and B offer powerful protection.
Sleep and stress
Poor sleep and chronic stress worsen metabolic risk and inflammation.
Practical tip:
Use a Green–Amber–Red plate model to guide daily meals — more green, less red.
Treatment Options
Management depends on disease cause and progression — individualised assessment is essential.
Viral hepatitis
- Hepatitis B: long-term antivirals reduce cancer and cirrhosis risk
- Hepatitis C: most patients are now cured within 8–12 weeks using direct-acting antivirals
MASLD/MASH (Fatty Liver)
- Weight loss, exercise, improved glucose control
- New emerging therapies for selected patients with fibrosis
Alcohol-Related Liver Disease
- Complete abstinence critical
- Counselling and support programmes improve success
Autoimmune liver disease
- Immunosuppressive medications (e.g., steroids, UDCA) slow progression
Genetic liver disorders
- Condition-specific treatments (phlebotomy for haemochromatosis, chelation for Wilson’s disease)
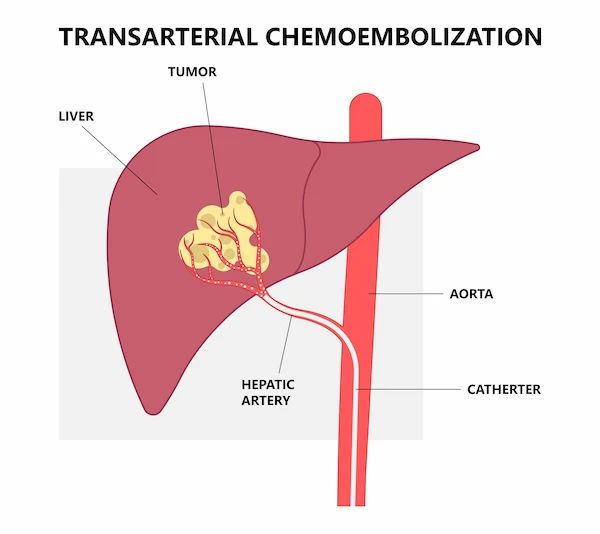
Advanced/end-stage disease
- Management of complications
- Liver transplantation for selected severe cases
If unsure what applies to you, speak with a doctor online via Apollo 24|7 for next-step guidance.
Medicines, Supplements, and Your Liver
Your liver processes most medicines — mindful use prevents harm.
Paracetamol safety
- Follow labelled daily maximums
- Avoid combining multiple paracetamol-containing products
- Avoid alcohol when taking paracetamol
Herbal and bodybuilding supplements
Some “natural” products — e.g., kava, certain weight-loss herbs — are linked to liver injury. Always disclose supplements to your doctor.
Annual medication review
Ask your doctor or pharmacist to reassess your full medication list each year.
Screening and Vaccination Guidelines
Screening catches liver disease before symptoms — where prevention works best.
Who should get screened?
- All adults for Hepatitis C at least once
- People with diabetes/metabolic syndrome for fatty liver
- High-risk groups for Hepatitis B
- Those with cirrhosis or high-risk hepatitis B require HCC surveillance every 6 months
If access is difficult, Apollo24|7 testing and online doctor consultations simplify the process.
Special Populations
Different life stages require tailored liver-health vigilance.
Pregnancy
Some liver problems rapidly worsen during pregnancy; urgent evaluation is required for severe itching or jaundice.
Children & adolescents
Paediatric fatty liver is increasing due to rising obesity — family-level lifestyle changes are crucial.
Older adults
Age reduces liver regeneration — cautious medication and alcohol use are essential.
Myths vs Facts About Liver Health
Clearing confusion empowers smart decisions.
How to Talk to Your Doctor
The better prepared you are, the faster you get answers and solutions.
What to share
- Alcohol habits (be honest)
- Medication/supplement list
- Family history and risk factors
- Any concerning symptoms
Smart questions to ask
- Do I need vaccines for Hepatitis A or B?
- What do my ALT, AST and platelet levels indicate?
- Should I have a FibroScan?
- Do I need surveillance for liver cancer?
Track changes over time
Record weight, waist circumference, blood glucose, and liver test trends in a simple logbook.
Online consults via Apollo 24|7 can help set achievable goals and arrange follow-up.
Resources and Future Directions in Liver Care
Global initiatives aim to detect disease earlier and prevent complications.
Reliable further information
- WHO — Viral hepatitis information and elimination goals
- National liver foundations — support groups and awareness material
- Medical associations — trustworthy patient education
What’s coming soon
- Greater use of AI tools to identify high-risk individuals
- More accessible non-invasive fibrosis tests
- A growing number of metabolic-targeted medicines
- Better integrated care for patients with diabetes and obesity
The future is optimistic — especially when patients take preventive steps early.
Conclusion
The liver’s role is profound — yet liver disease often hides until serious harm has already occurred. By learning key symptoms, addressing risk factors such as alcohol intake and metabolic health, staying vaccinated against hepatitis, and using appropriate screening tools, you can protect yourself long before damage becomes irreversible.
Even if you already have liver disease, modern treatments — from antiviral cures to emerging therapies for fatty liver — offer real hope. Combining medical care with small, sustainable lifestyle changes can dramatically improve outcomes.
If concerns persist or symptoms develop, consult a doctor online with Apollo 24|7. For diagnostic clarity, book a convenient home collection for liver function and related tests. Your liver works constantly for you — now is the time to return the favour with awareness, action, and preventive care.
Consult a Top Hepatologist for Personalised Advice
Consult a Top Hepatologist for Personalised Advice

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(175+ Patients)

Dr. Pukhraj Singh Jeji
Gastroenterology/gi Medicine Specialist
13 Years • MBBS, MD ( Internal Medicine ), DM ( Gastroenterology ), Consultant - Gastroenterology
Bhubaneswar
Apollo Hospitals Old Sainik School Road, Bhubaneswar

Dr. Aswin S. Krishna
Hepatologist
10 Years • MBBS, MD (Internal Medicine,MMC), DM (Hepatology, MMC), PDF(Fellowship in Liver Transplanatation)
Chennai
Apollo Hospitals Greams Road, Chennai
(125+ Patients)

Dr. Aakash Garg
Gastroenterology/gi Medicine Specialist
12 Years • MBBS, DNB (Medicine), DrNB (Gastroentrology).
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur
(150+ Patients)

Dr U V U Vamsidhar Reddy
Hepatologist
10 Years • MBBS, MD (JIPMER), DM (Hepatology, PGIMER)
Chennai
Apollo Hospitals Greams Road, Chennai
(75+ Patients)
Consult a Top Hepatologist for Personalised Advice

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(175+ Patients)

Dr. Pukhraj Singh Jeji
Gastroenterology/gi Medicine Specialist
13 Years • MBBS, MD ( Internal Medicine ), DM ( Gastroenterology ), Consultant - Gastroenterology
Bhubaneswar
Apollo Hospitals Old Sainik School Road, Bhubaneswar

Dr. Aswin S. Krishna
Hepatologist
10 Years • MBBS, MD (Internal Medicine,MMC), DM (Hepatology, MMC), PDF(Fellowship in Liver Transplanatation)
Chennai
Apollo Hospitals Greams Road, Chennai
(125+ Patients)

Dr. Aakash Garg
Gastroenterology/gi Medicine Specialist
12 Years • MBBS, DNB (Medicine), DrNB (Gastroentrology).
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur
(150+ Patients)

Dr U V U Vamsidhar Reddy
Hepatologist
10 Years • MBBS, MD (JIPMER), DM (Hepatology, PGIMER)
Chennai
Apollo Hospitals Greams Road, Chennai
(75+ Patients)
More articles from Liver Cancer
Frequently Asked Questions
Q1: What are the early signs of liver disease?
Fatigue, abdominal discomfort, itching, dark urine, and pale stools are common early signs, but many people have none until the disease is advanced.
Q2: Can fatty liver be reversed naturally?
Yes. Weight reduction of 7–10%, a Mediterranean-style diet, and regular exercise can significantly improve liver fat and inflammation.
Q3: How much paracetamol is safe for the liver?
Follow labelled maximum doses. People who drink alcohol regularly or with liver disease may require lower limits — ask a doctor or pharmacist.
Q4: Who should be tested for hepatitis B and C?
All adults should be tested for Hepatitis C at least once. Hepatitis B testing is recommended for high-risk groups and in pregnancy.
Q5: When do I need to see a liver specialist?
If LFTs remain abnormal, fibrosis is suspected, viral hepatitis is confirmed, or symptoms like swelling, confusion, or jaundice develop.