Guide to Understanding Osteoporosis Bone Health
Discover everything you need to know about osteoporosis—causes, risk factors, symptoms, diagnosis, prevention, and treatment.

Written by Dr. Shaik Abdul Kalam
Reviewed by Dr. J T Hema Pratima MBBS, Fellowship in Diabetes Mellitus
Last updated on 13th Jan, 2026

Introduction
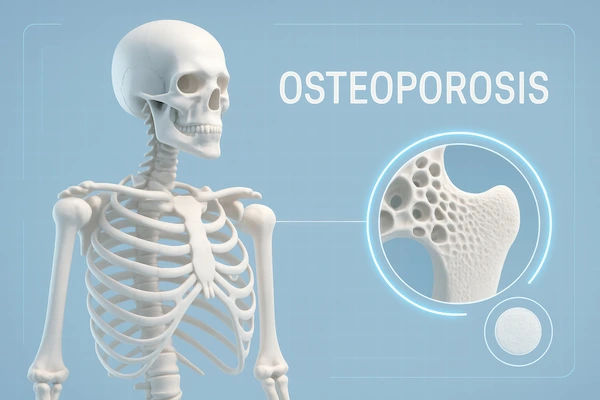
Imagine your skeleton as the foundation of your body. For millions, this foundation silently weakens over time, a condition known as osteoporosis. Often called a "silent disease" because it progresses without symptoms until a fracture occurs, osteoporosis affects over 200 million people worldwide, predominantly postmenopausal women, but also men. It's characterized by a decrease in bone density and quality, making bones porous, fragile, and susceptible to breaks from minor falls or even simple actions like bending over. But here's the crucial message: osteoporosis is not an inevitable part of aging. This guide will empower you with knowledge—from understanding your risk factors and getting an accurate diagnosis to actionable strategies for prevention and management. We'll explore the vital roles of nutrition, exercise, and modern treatments in building and maintaining strong, resilient bones for life.
What Exactly Is Osteoporosis? Beyond Just "Weak Bones"
Osteoporosis is more than just weak bones; it's a systemic skeletal disorder. To understand it, we must first see bone as the living, dynamic tissue it is.
The Living Tissue: How Your Bones Remodel Themselves
Your bones are constantly undergoing a process called remodelling. Special cells called osteoclasts break down and resorb old bone, while cells called osteoblasts form new bone tissue. This process is essential for repairing micro-damages from everyday stress and for regulating calcium levels in your blood. In your youth, bone formation outpaces resorption, allowing you to reach your peak bone mass around age 30.
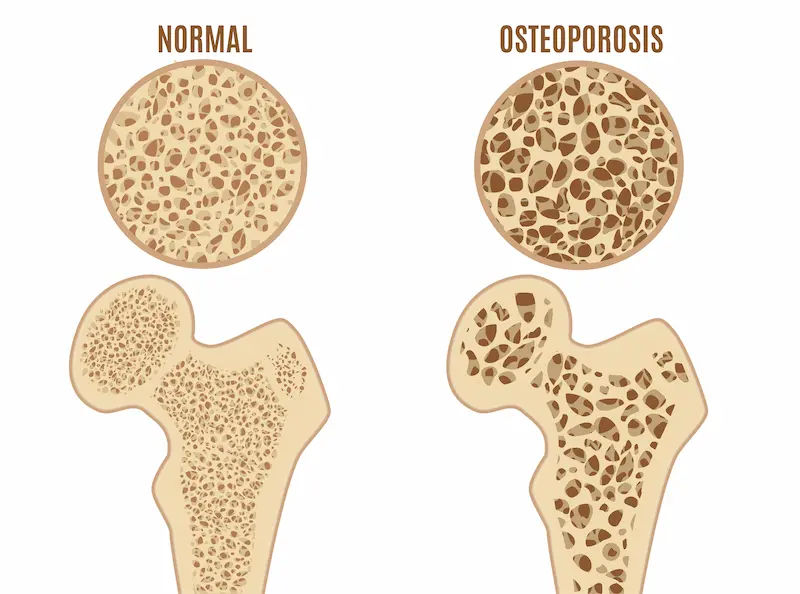
When the Balance is Lost: Bone Loss vs. Bone Formation
Osteoporosis occurs when this delicate balance is disrupted. As we age, and particularly after menopause in women due to dropping oestrogen levels, bone resorption begins to outpace bone formation. The inner honeycomb-like structure of the bone becomes more porous, and the outer shell becomes thinner. This loss of bone mineral density and deterioration of bone microarchitecture is what leads to increased fragility and fracture risk. It’s not that your bones are just "weak"; their internal structure has fundamentally changed for the worse.
Consult an Orthopaedist or Rheumatologist for the best advice
Understanding the Causes and Risk Factors of Osteoporosis
Knowing your risk is the first step toward prevention. These factors are divided into those you can't change and those you can influence.
Unchangeable Risks: Age, Gender, and Genetics
Age: Risk increases significantly after 50.
Gender: Women are at higher risk because they have lower peak bone mass and experience rapid bone loss after menopause.
Family History: Having a parent who had a hip fracture doubles your own risk.
Body Frame Size: Men and women with small body frames tend to have a higher risk because they may have less bone mass to draw from as they age.
Race: Those of White or Asian descent are at highest risk.
Lifestyle and Dietary Factors You Can Control
Low Calcium & Vitamin D Intake: A lifelong lack of these nutrients contributes to diminished bone density.
Eating Disorders: Severely restricting food intake and being underweight weakens bone.
Sedentary Lifestyle: Bones become stronger with use. Inactivity accelerates bone loss.
Tobacco and Alcohol Use: Tobacco use contributes to weak bones. Similarly, more than two alcoholic drinks a day can increase your risk.
Certain Medications: Long-term use of corticosteroid medications (e.g., prednisone) interferes with the bone-rebuilding process.
The Silent Thief: Recognizing the Signs and Symptoms
Osteoporosis is notorious for its lack of early warning signs. Pain is not typically present until a fracture occurs.
Early Indicators Often Go Unnoticed
There are often no clear symptoms of osteoporosis in women or men in the early stages. The bone loss itself is painless. Many first discover they have low bone density after a minor incident causes an unexpected fracture.
The Tell-Tale Signs of Advanced Bone Loss
As the condition progresses, symptoms may include:
Back pain, caused by a fractured or collapsed vertebra.
Loss of height over time.
A stooped posture or curvature of the spine (sometimes called a "dowager's hump").
A bone that breaks much more easily than expected (e.g., from a minor fall or cough).
Getting a Diagnosis: How Osteoporosis is Detected
If you have risk factors or are over 65 (or postmenopausal with risk factors), discussing screening with your doctor is crucial.
The Gold Standard: The DEXA Scan (Bone Density Test)
A dual-energy X-ray absorptiometry (DEXA or DXA) scan is the most common and accurate test to measure bone mineral density. It's a quick, non-invasive, and painless test that uses low levels of X-rays to scan typically the hip and spine.
Understanding Your T-Score and What It Means
The result of your DEXA scan is reported as a T-score, which compares your bone density to that of a healthy 30-year-old adult.
Normal: T-score of -1.0 and above
Osteopenia (Low Bone Mass): T-score between -1.0 and -2.5
Osteoporosis: T-score of -2.5 or below
Other Tests: FRAX Assessment and Laboratory Tests
Your doctor may use the FRAX® tool, which incorporates your T-score and other risk factors to estimate your 10-year probability of having a major fracture. Blood and urine tests may also be ordered to rule out other conditions that can cause bone loss or to check levels of calcium, vitamin D, and other markers. Apollo24|7 offers convenient home collection for tests like vitamin D or calcium levels, making it easier to get the insights you need.
Building Your Defense: Proactive Prevention of Osteoporosis
Prevention is the best medicine. Building strong bones before age 30 and slowing loss afterward is key.
The Dynamic Duo: Calcium and Vitamin D for Bone Health
Calcium: The primary mineral in bone. Adults need 1,000-1,200 mg daily. Excellent sources include dairy products, dark leafy greens, sardines, and fortified foods.
Vitamin D: Essential for calcium absorption. Your skin makes it from sunlight, but many people are deficient. Aim for 600-800 IU daily from fatty fish, fortified foods, or supplements.
The Best Exercises for Building Bone Density
Bone responds to force by becoming stronger. The best exercises for osteoporosis are:
Weight-Bearing: Walking, jogging, climbing stairs, dancing.
Strength Training: Using free weights, resistance bands, or weight machines to stress the bones in your arms and upper spine.
Balance Exercises: Tai chi and yoga can improve balance and coordination, reducing the risk of falls.
Lifestyle Choices: Smoking, Alcohol, and Bone Health
Quitting smoking is one of the single best things you can do for your bones and overall health. If you drink alcohol, do so in moderation (no more than one drink per day for women, two for men).
Treatment Options: Strengthening Bones After a Diagnosis
A diagnosis of osteoporosis isn't a life sentence of fragility. Effective treatments can slow bone loss and even rebuild bone.
Common Medications and How They Work
Bisphosphonates (e.g., alendronate, risedronate): The most commonly prescribed treatment for osteoporosis. They slow the rate of bone breakdown.
Monoclonal Antibodies (e.g., Denosumab): Given by injection every six months, it targets a protein involved in bone breakdown.
Anabolic Agents (e.g., Teriparatide, Abaloparatide): These are bone-building medications, reserved for those with very high fracture risk.
The Role of Hormone Replacement Therapy (HRT)
Oestrogen therapy can help maintain bone density in postmenopausal women. However, due to potential risks (e.g., blood clots, certain cancers), it's only recommended for women at significant risk of osteoporosis who also need treatment for menopausal symptoms. It's essential to discuss the risks and benefits with a specialist. You can consult a gynaecologist or endocrinologist online with Apollo24|7 to get personalised advice.
Living Well with Osteoporosis: Safety and Fracture Prevention
Managing osteoporosis is a lifelong commitment focused on safety and maintaining quality of life.
Fall-Proofing Your Home Environment
Most serious fractures are caused by falls. Simple changes can drastically reduce risk:
Remove tripping hazards like loose rugs and electrical cords.
Use non-slip mats in the shower and bathtub.
Install grab bars next to your toilet and in the shower.
Ensure your home is well-lit.
Nutrition and Exercise Plans for Managing Bone Health
Continue following a bone-healthy diet and exercise plan tailored to your abilities. A physical therapist can design a safe programme that emphasises strength and balance without risking injury.
Conclusion
Understanding osteoporosis is the first powerful step toward taking control of your bone health. While certain risk factors are beyond our control, the power of prevention and management through nutrition, exercise, and informed medical care should not be underestimated. Building strong bones is a lifelong investment that pays dividends in your mobility, independence, and overall quality of life as you age. Remember, it's never too early or too late to start prioritizing your skeletal health. If you have concerns about your risk factors, have experienced a loss in height, or are simply entering a high-risk age group, take the proactive step of speaking with a healthcare professional. Your future, fracture-free self will thank you for the strong foundation you build today.
Consult an Orthopaedist or Rheumatologist for the best advice
Consult an Orthopaedist or Rheumatologist for the best advice

Dr. Anil Pradeep Jadhav
Orthopaedician
23 Years • MBBS MS (Ortho)
Nashik
Apollo Hospitals Nashik, Nashik
(25+ Patients)

Dr. Suraj Prakash
Orthopaedician
5 Years • MBBS, MS (Ortho)
Bengaluru
Apollo Clinic, Indiranagar, Bengaluru

Dr. Padam Singh Gautam
General Physician/ Internal Medicine Specialist
43 Years • M.B.B.S (WARDHA M. S.), F.A.G.E. (MANIPAL), F.A.I.M.S. (Pb.), M.A.I.M.S. (Pb.), M.R.S.H. (LONDON)
Noida
Dr Padam Singh Gautam Fracture Clinic, Noida

Dr. Susheel B
Orthopaedician
13 Years • MBBS, MS, Ortho Fellowship in Trauma ( Germany) Fellowship in Arthroscopy and Arthroplasty ( Switzerland)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Prof. Dr. Jambu N
Orthopaedician
23 Years • MBBS, M.S Ortho, FRCS ,FACS
Chennai
Apollo Speciality Hospitals Vanagaram, Chennai
(150+ Patients)
More articles from Osteopetrosis
Frequently Asked Questions
1. What is the difference between osteopenia and osteoporosis?
Both mean low bone density, but osteopenia is a precursor to osteoporosis. Think of it as the middle ground between healthy bones and osteoporosis. It's a warning sign to take action to prevent progression.
2. Can men get osteoporosis?
Absolutely. While more common in women, about 1 in 4 men over 50 will break a bone due to osteoporosis. Risk factors for men include low testosterone, certain medications, and chronic diseases.
3. Are there any natural remedies for osteoporosis?
The most effective 'natural' strategies are a diet rich in calcium rich foods for bones (like dairy, leafy greens, and fortified foods), adequate vitamin D from sunlight or supplements, and regular weight-bearing exercise. Always discuss supplements with your doctor first.
4. How often should I get a bone density test?
If your initial test is normal or shows osteopenia, your doctor may recommend a follow-up in 2-5 years. If you are on medication for osteoporosis, a test every 1-2 years is typical to monitor treatment effectiveness.
5. Can you reverse osteoporosis?
While you may not fully 'reverse' it to the bone density of a 30-year-old, treatment can significantly increase bone density and strength over time, moving you from the osteoporosis category back into osteopenia and drastically reducing your fracture risk.


 (1).webp)