Understanding Osteoporosis Bone Health
Explore the causes, symptoms, and prevention of osteoporosis. Learn how to protect your bone health through nutrition, exercise, and early diagnosis to reduce the risk of fractures and bone loss.

Written by Dr. Shaik Abdul Kalam
Reviewed by Dr. J T Hema Pratima MBBS, Fellowship in Diabetes Mellitus
Last updated on 13th Jan, 2026
%20(1).webp?tr=q-80,f-webp,w-350,dpr-2,c-at_max 700w)
Imagine your bones as the foundation of your house. For years, they’re strong and silent, supporting everything you do. But what if that foundation slowly, quietly began to crumble without you even noticing? This is the reality of osteoporosis, a “silent disease” characterised by weakened bones and an increased risk of sudden, unexpected fractures. It’s not just an inevitable part of ageing; it’s a manageable condition. Whether you’re in your 30s looking to build a strong bone foundation or in your 60s seeking to preserve your bone health, this guide will empower you with the knowledge to take control. We’ll break down the causes, symptoms, and diagnosis process, and provide actionable strategies for treatment and prevention to help you live a stronger, more vibrant life.
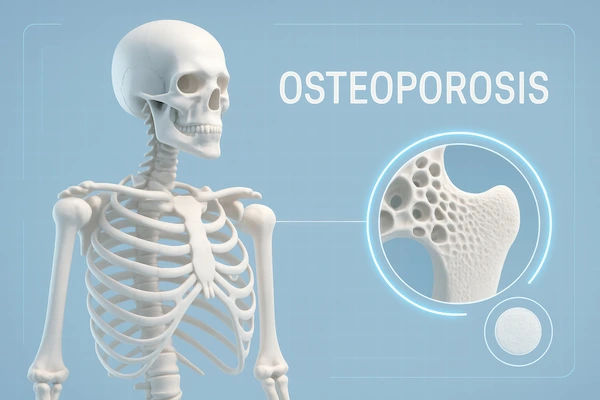
What is Osteoporosis?
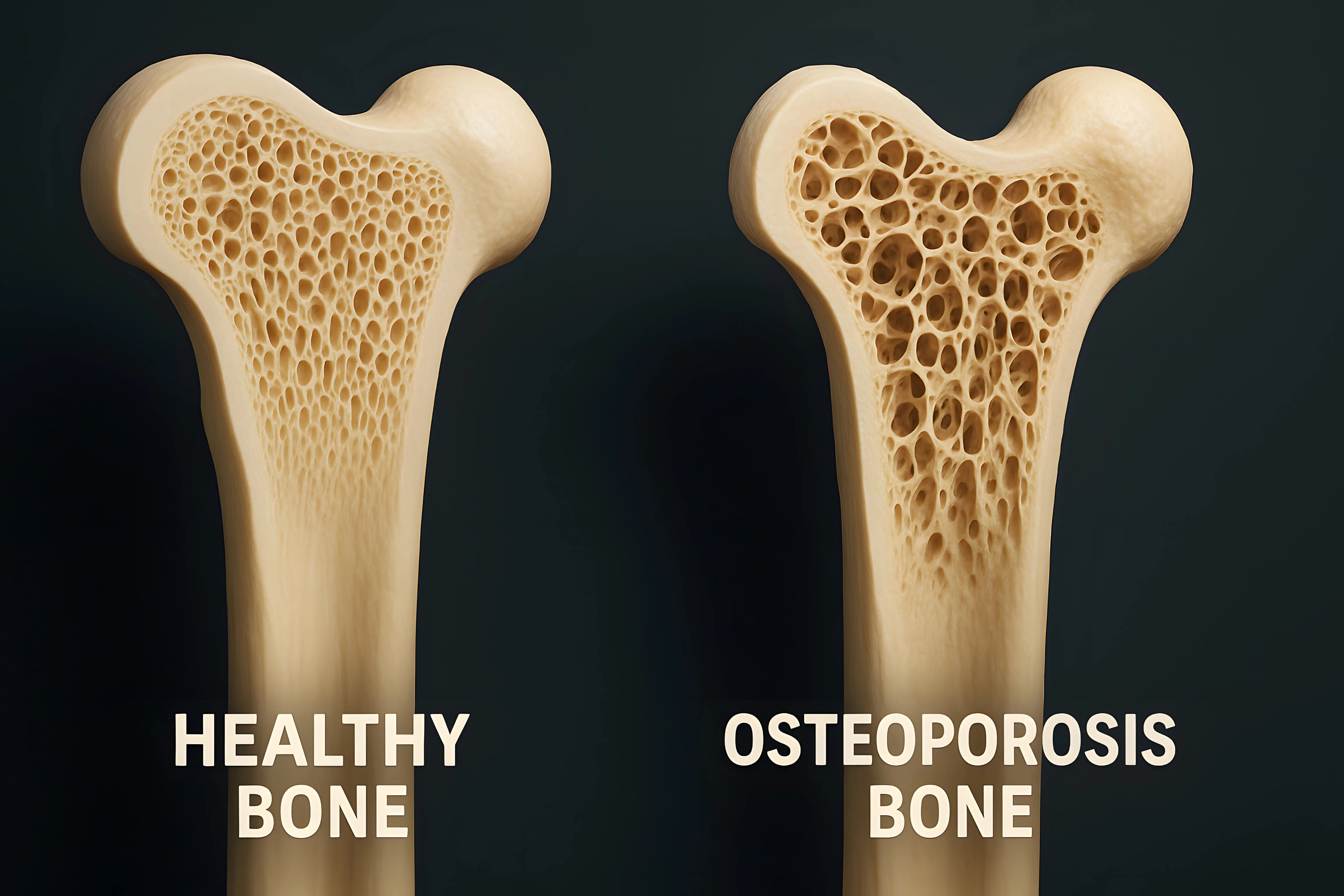
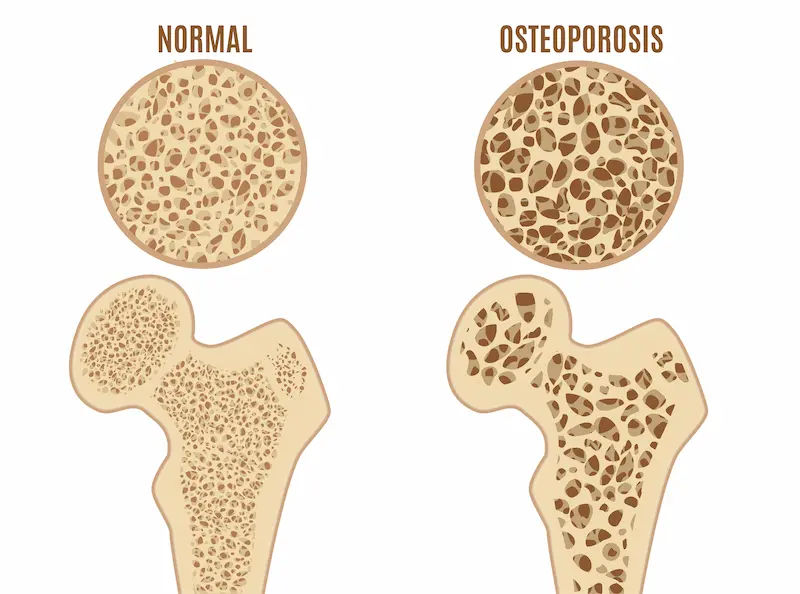
Osteoporosis is a bone disease that occurs when the body loses too much bone, makes too little bone, or both. This results in bones becoming weak, porous, and brittle—so fragile that a minor fall, bending over, or even coughing can cause a fracture. The term literally means “porous bone.” Under a microscope, healthy bone looks like a dense honeycomb. In osteoporotic bone, these spaces and holes become much larger, significantly reducing density and strength.
Bone Density vs. Bone Quality
While bone mineral density (BMD) is the primary measurement used for diagnosis, it's only part of the story. Bone quality—a measure of the architecture, turnover, and mineralisation of bone—is equally important. Think of it like a wooden beam: you can have a thick beam (good density) that is riddled with termite holes (poor quality), making it prone to snapping. This is why some people with only moderately low density can experience fractures, while others with lower density might not. Modern research is increasingly focused on assessing both factors for a complete picture of bone health.
Key Osteoporosis Risk Factors
Understanding your risk is the first step toward prevention. These factors are divided into those you can't change and those you can.
Non-Modifiable Risk Factors (What You Can't Change)
Sex: Women are far more likely to develop osteoporosis than men, primarily due to the dramatic drop in estrogen during menopause, which accelerates bone loss.
Age: The older you get, the higher your risk. Bone rebuilding slows down naturally after your mid-30s.
Family History: Having a parent or sibling with osteoporosis or a hip fracture puts you at greater risk, suggesting a genetic link.
Body Frame Size: Men and women with small body frames tend to have a higher risk because they may have less bone mass to draw from as they age.
Race: Those of White or Asian descent are at highest risk.
Modifiable Risk Factors (What You Can Control)
Sex Hormone Levels: Lowered estrogen in women (e.g., from menopause or surgical removal of ovaries) and low testosterone in men are significant contributors.
Dietary Factors: Inadequate calcium and vitamin D intake throughout your life plays a major role in the development of osteoporosis.
Medications: Long-term use of corticosteroid medications (e.g., prednisone) is devastating to bone. Other drugs, like some for cancer or seizures, can also increase risk.
Lifestyle: A sedentary lifestyle, excessive alcohol consumption (more than 2 drinks a day), and tobacco use all weaken bones significantly.
Recognising Osteoporosis Symptoms
The most challenging aspect of osteoporosis is its silent progression. There are typically no symptoms of osteoporosis in the early stages of bone loss.
The First Sign is Often a Fracture
Often, the first clinical sign is a fracture itself. This could be a broken wrist from a minor fall, a hip fracture after a stumble, or a fracture in the spine (vertebrae) from something as simple as bending forward to pick up a grocery bag.
Posture Changes and Chronic Pain
Once bones have been weakened by osteoporosis, you might experience:
Back pain, caused by a fractured or collapsed vertebra.
Loss of height over time.
A stooped posture or dowager’s hump (kyphosis).
A bone that breaks much more easily than expected.
If you notice a sudden onset of back pain or a change in your posture, it is crucial to consult a doctor. If your condition does not improve after trying these methods, book a physical visit to a doctor with Apollo24|7 for further evaluation.
How Osteoporosis is Detected?
Early diagnosis is key to preventing fractures. Diagnosis typically involves a combination of a physical exam, reviewing your medical history, and specialized tests.
The DXA Bone Density Scan
The most common and accurate way to diagnose bone loss is a DEXA scan (Dual-energy X-ray Absorptiometry). It's a quick, non-invasive, and painless test that uses low levels of X-rays to measure the bone mineral density in your spine and hip.
Understanding Your T-Score
Your results are given as a T-score, which compares your bone density to that of a healthy 30-year-old adult.
Normal: T-score of -1.0 and above.
Osteopenia (Low bone mass): T-score between -1.0 and -2.5. This is a warning sign.
Osteoporosis: T-score of -2.5 and below.
Other Diagnostic Tools
Your doctor may also use the FRAX® tool, which uses your bone density and other risk factors to estimate your 10-year risk of having a major fracture. Additionally, blood tests for osteoporosis may be ordered to rule out other conditions that can cause bone loss, such as thyroid problems or vitamin D deficiency. Apollo24|7 offers convenient home collection for tests like vitamin D or HbA1c to help in this diagnostic process.
Consult Top Specialists
Treatment Options for Osteoporosis
Osteoporosis treatment aims to slow or stop bone loss, prevent fractures, and manage pain. A comprehensive plan is always multi-faceted.
Prescription Medications to Halt Bone Loss and Build Bone
Several classes of drugs are effective:
Bisphosphonates (e.g., alendronate, risedronate): The most commonly prescribed medications for osteoporosis. They slow bone breakdown.
Monoclonal Antibodies (e.g., Denosumab): Given by injection every six months, it reduces bone breakdown.
Anabolic Agents (e.g., Teriparatide, Abaloparatide): These are bone-building medications, reserved for those with very high fracture risk.
Hormone-Related Therapy: Estrogen therapy for women and testosterone therapy for men can help maintain bone density.
Calcium and Vitamin D Supplementation
Medication is ineffective without proper nutritional building blocks. Calcium and vitamin D for bones are non-negotiable.
Calcium: The recommended daily amount for adults over 50 is 1,200 mg. Focus on dietary sources first (dairy, leafy greens, fortified foods).
Vitamin D: Crucial for calcium absorption. The recommended daily amount for adults is 600-800 IU. Sun exposure and supplements are often necessary.
How to Protect Your Bone Health?
It’s never too early or too late to invest in your bone health. The best way to prevent osteoporosis is through proactive lifestyle choices.
Nutrition for Strong Bones
A bone-healthy diet is rich in:
Calcium: Dairy products, almonds, broccoli, kale, canned salmon with bones.
Vitamin D: Fatty fish (tuna, mackerel), egg yolks, fortified milk and cereals.
Protein: Lean meat, poultry, fish, beans, lentils. Protein makes up about 50% of bone volume.
Other Key Nutrients: Magnesium (nuts, seeds), Potassium (fruits and vegetables), and Vitamin K (leafy greens).
The Best Exercises for Bone Density
Bone is living tissue that gets stronger under stress. The best exercises for bone density are:
Weight-Bearing Exercises: Force you to work against gravity. This includes walking, jogging, dancing, tennis, and stair climbing.
Strength Training: Using free weights, resistance bands, or your own body weight (e.g., squats, push-ups) places stress on bones, stimulating them to become stronger.
Balance and Stability Exercises: Tai chi and yoga can improve balance and coordination, critically reducing your risk of falls.
Fall Prevention Strategies at Home
Preventing falls is paramount. Make your home safer by:
Removing clutter and loose wires from floors.
Using non-slip mats in the bathtub and shower.
Installing grab bars next to the toilet and in the shower.
Ensuring bright lighting throughout your home, especially on stairs.
Living Well with Osteoporosis
A diagnosis of osteoporosis is not a life sentence of limitation. It’s a call to action. By embracing treatment, prioritising nutrition, staying active with safe exercises for bone density, and making your environment safe, you can significantly reduce your risk of fracture and maintain your independence and quality of life for years to come.
Conclusion
Your journey to stronger bone health is a lifelong commitment, but it is one filled with empowering choices. Understanding osteoporosis—from its silent beginnings to its proactive management—is your greatest weapon. By incorporating a nutrient-rich diet, a consistent and bone-smart exercise regimen, and regular check-ups, you can actively fortify your body’s foundation. Remember, the choices you make today, from taking a walk to choosing a calcium-rich snack, directly impact your strength and mobility tomorrow. Don’t wait for a wake-up call. Start a conversation with your healthcare provider about your bone health and take the first step towards a future of unwavering strength and vitality.
Consult Top Specialists
Consult Top Specialists

Dr. Anil Pradeep Jadhav
Orthopaedician
23 Years • MBBS MS (Ortho)
Nashik
Apollo Hospitals Nashik, Nashik
(25+ Patients)

Dr. Rupam Chowdhury
Orthopaedician
10 Years • MBBS, DNB (Ortho.)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr. Suraj Prakash
Orthopaedician
5 Years • MBBS, MS (Ortho)
Bengaluru
Apollo Clinic, Indiranagar, Bengaluru

Dr. Padam Singh Gautam
General Physician/ Internal Medicine Specialist
43 Years • M.B.B.S (WARDHA M. S.), F.A.G.E. (MANIPAL), F.A.I.M.S. (Pb.), M.A.I.M.S. (Pb.), M.R.S.H. (LONDON)
Noida
Dr Padam Singh Gautam Fracture Clinic, Noida

Dr. Susheel B
Orthopaedician
13 Years • MBBS, MS, Ortho Fellowship in Trauma ( Germany) Fellowship in Arthroscopy and Arthroplasty ( Switzerland)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru
More articles from Osteopetrosis
Frequently Asked Questions
1. What is the difference between osteopenia and osteoporosis?
Both indicate low bone density, but osteopenia is a precursor, not a full-blown disease. Think of it as the warning stage where bone density is lower than normal but not yet at the fragile level of osteoporosis. It's a critical time to intervene with lifestyle changes.
2. Can men get osteoporosis?
Absolutely. While more common in women, about 20-25% of osteoporotic fractures occur in men. Risk factors for men include low testosterone, excessive alcohol use, smoking, and long-term use of certain medications like corticosteroids.
3. Are there any natural treatments for osteoporosis?
Natural management is a cornerstone of treatment but should complement, not replace, a doctor's plan. It focuses on high-impact lifestyle changes: ensuring adequate calcium and vitamin D intake through diet and supplements, engaging in regular weight-bearing exercises, avoiding smoking, and limiting alcohol.
4. How often should I get a bone density test?
If you have normal bone density or mild osteopenia, repeating a DEXA scan every 2-5 years is typical. If you are on osteoporosis treatment, your doctor may recommend testing every 1-2 years to monitor the effectiveness of the medication.
5. What are the best dietary sources of calcium for someone who is lactose intolerant?
Excellent non-dairy sources of calcium include canned sardines and salmon (with bones), fortified plant-based milks (almond, soy, oat), tofu made with calcium sulfate, dark leafy greens (kale, collards), almonds, and broccoli.