understanding-osteoporosis-causes-and-bone-impact
Discover how cooled radiofrequency treatment can help manage chronic knee pain, reduce discomfort, and improve mobility.

Written by Dr. Mohammed Kamran
Reviewed by Dr. D Bhanu Prakash MBBS, AFIH, Advanced certificate in critical care medicine, Fellowship in critical care medicine
Last updated on 13th Jan, 2026

Introduction
Have you ever thought of your bones as a living bank account? Throughout your life, you make deposits (bone formation) and withdrawals (bone loss). Osteoporosis occurs when withdrawals consistently exceed deposits, leaving your bones porous, fragile, and susceptible to fractures from minor falls or even simple actions like bending over. Often called a "silent disease," it progresses without symptoms until a bone breaks. This article will demystify what leads to osteoporosis, explore its profound impact on your skeletal strength and overall quality of life, and provide a clear roadmap for protecting your bone health. Understanding these factors is the first crucial step toward building a resilient framework for your body that lasts a lifetime.
What is Osteoporosis? The Silent Thief of Bone
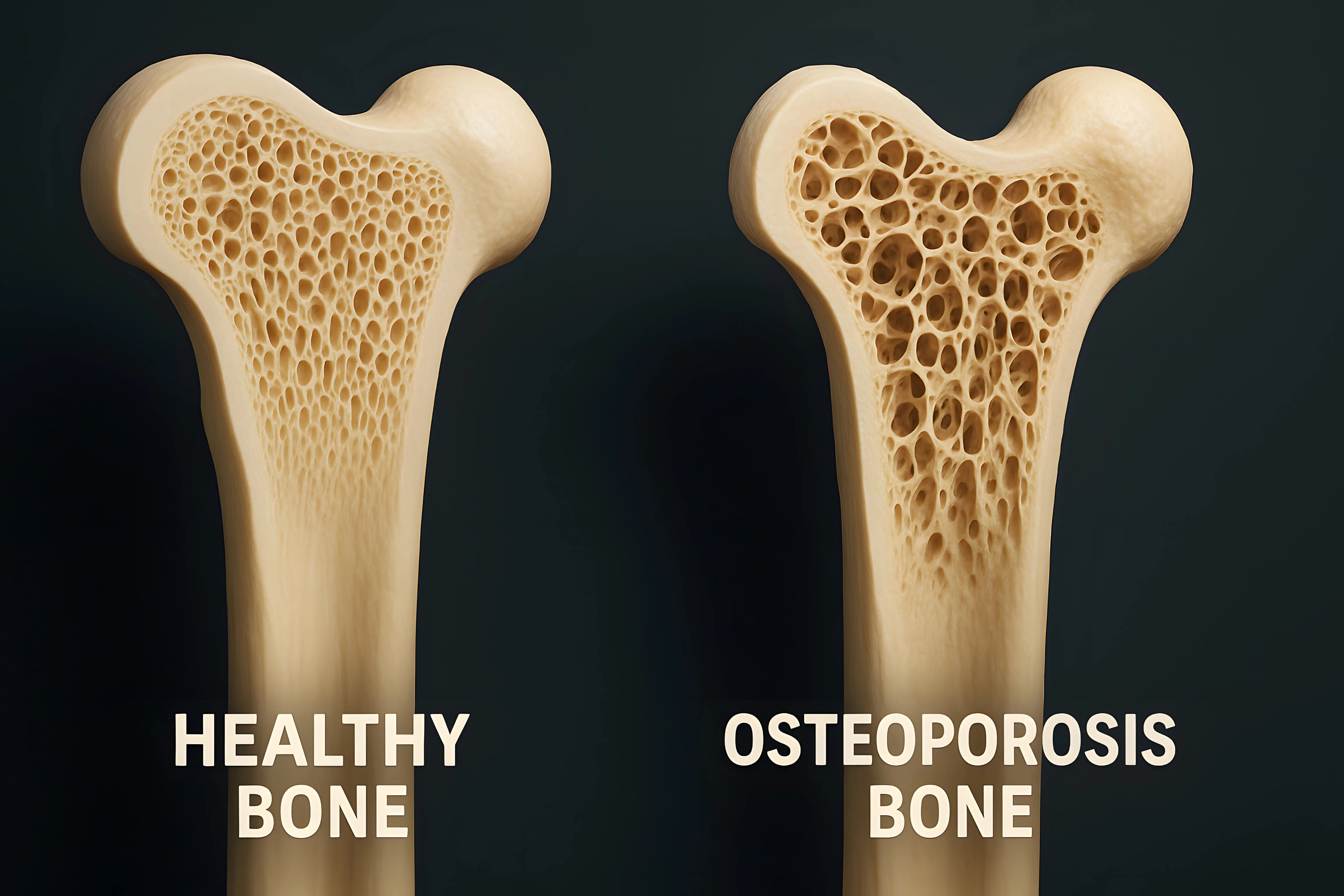
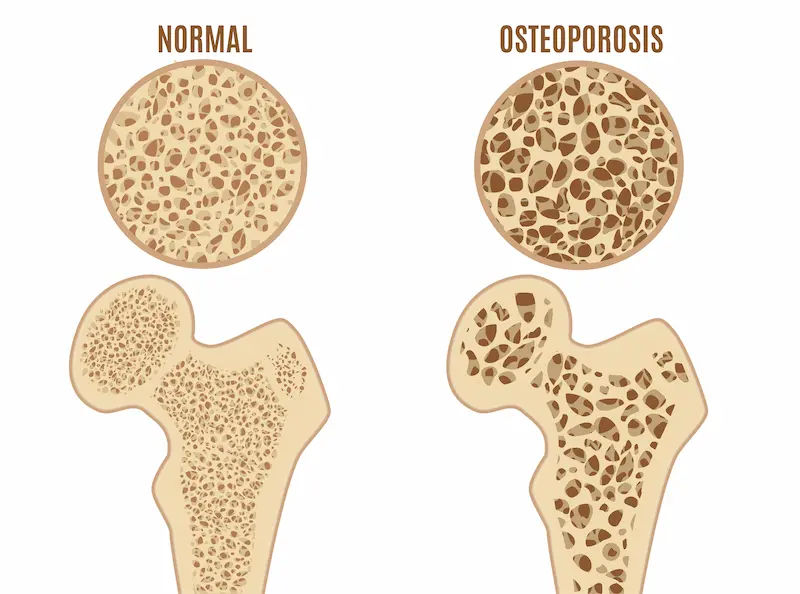
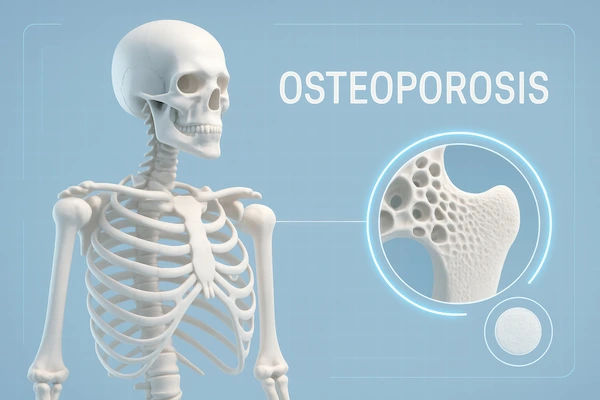
Osteoporosis literally means "porous bone." It is a chronic disease characterised by a decrease in bone density and quality, leading to weakened bones and an increased risk of fractures. Imagine a healthy bone's internal structure like a dense honeycomb. With osteoporosis, the holes and spaces in this honeycomb become much larger, making the bone less dense, significantly weaker, and more fragile.
The "silent" nature of the disease is what makes it so dangerous. Unlike many other health conditions, there is often no pain or obvious warning signs as bone mass deteriorates. Many people only discover they have osteoporosis after they suffer a sudden and unexpected fracture. The most common sites for these osteoporosis-related fractures are the hip, spine, and wrist. A fracture, especially later in life, can be a life-altering event, leading to chronic pain, loss of independence, and reduced quality of life.
The Primary Causes of Osteoporosis
The development of osteoporosis is typically not due to a single cause but a combination of factors that disrupt the delicate balance of bone remodelling—the lifelong process where old bone is broken down and new bone is formed.
The Role of Hormones: Oestrogen and Testosterone
Hormones are critical regulators of bone density. The most common cause of osteoporosis in women is the sharp decline in oestrogen during menopause. Oestrogen is a key protector of bones; its reduction accelerates bone loss. Similarly, in men, low levels of testosterone can lead to bone loss. Other hormonal disorders, such as an overactive thyroid (hyperthyroidism), overactive parathyroid glands (hyperparathyroidism), and adrenal disorders like Cushing's syndrome, can also severely disrupt bone remodelling.
Nutritional Deficiencies: Beyond Just Calcium
Your bones are a living tissue that requires constant nourishment. Chronic deficiency in key nutrients is a direct pathway to weakened bones.
• Calcium: The primary mineral that gives bones their strength and structure.
• Vitamin D: Absolutely essential for the body to effectively absorb calcium. Without it, your body cannot use the calcium you consume.
• Protein: Provides the foundational matrix upon which minerals are deposited.
• Other Micronutrients: Magnesium, Vitamin K, and Zinc also play vital supporting roles in bone health.
Lifestyle Factors: The Impact of Activity and Habits
A sedentary lifestyle is a major contributor to bone loss. Weight-bearing exercises (like walking, dancing, or lifting weights) send signals to the body to strengthen bones. Conversely, a lack of exercise tells the body that strong bones are not needed, leading to resorption. Furthermore, excessive alcohol consumption interferes with the body's calcium balance and vitamin D production. Similarly, tobacco use is directly toxic to bone-forming cells (osteoblasts), significantly harming bone health.
Medical Conditions and Medications
Certain conditions and their treatments can lead to secondary osteoporosis. These include gastrointestinal diseases like Coeliac or Crohn's (which impair nutrient absorption), rheumatoid arthritis, and some cancers. Long-term use of corticosteroids (e.g., prednisolone) is one of the most common causes of drug-induced osteoporosis, as they dramatically hinder the bone-forming process. Other medications, like some used for seizures and cancer, can also have adverse effects.
How Osteoporosis Impacts Your Bone Health and Body
The impact of osteoporosis extends far beyond a simple diagnosis; it affects the very architecture of your skeleton and your daily life.
The Weakened Microarchitecture of Bone
The internal scaffolding of your bones becomes compromised. The trabecular bone (the spongy interior) develops thinned and broken connections, while the cortical bone (the hard outer shell) becomes thinner. This structural decay means bones can no longer withstand normal stresses.
The Domino Effect of Fractures
A fracture often begins a devastating cycle. A vertebral fracture in the spine can lead to a stooped posture (kyphosis), which shifts your centre of gravity. This new posture increases the risk of falling and suffering a subsequent, more devastating hip fracture. Hip fractures frequently require surgery and prolonged rehabilitation, and are associated with a significant loss of independence and increased mortality in the year following the break.
The Pain and Loss of Mobility
The impact is profoundly physical and emotional. Multiple spinal fractures can cause chronic back pain and a severe loss of height. The resulting stoop can compress the abdomen, leading to discomfort and digestive issues. The fear of falling and fracturing a bone can cause anxiety and cause individuals to withdraw from social activities and exercise, further accelerating bone loss and isolation.
Who is at Risk? Key Risk Factors You Can't Ignore
While anyone can develop osteoporosis, certain factors increase susceptibility.
• Unchangeable Risks: Female sex, advanced age, small body frame, family history of osteoporosis or fractures, Caucasian or Asian ethnicity.
• Changeable Risks: Low calcium/vitamin D intake, sedentary lifestyle, smoking, excessive alcohol, eating disorders, certain medications (as above).
Proactive Steps: Prevention and Building Stronger Bones
It's never too early or too late to take action for your bone health. Prevention is the most effective strategy.
The Power of Diet: Key Nutrients for Bone Density
Aim for a balanced diet rich in calcium (dairy, leafy greens, fortified foods) and ensure adequate Vitamin D through sunlight exposure, fatty fish, or supplements as needed. If you struggle to get enough through diet, a doctor can order a simple blood test to check your levels. Apollo24|7 offers convenient home collection for tests like vitamin D, making it easy to monitor your status.
Exercise: The Best Medicine for Your Bones
Engage in a mix of:
• Weight-bearing exercises: Walking, jogging, tennis (30 mins most days).
• Strength training: Lifting weights or using resistance bands (2-3 times per week).
• Balance exercises: Tai chi or yoga to prevent falls.
Lifestyle Modifications for Long-Term Health
Avoid smoking and limit alcohol to no more than one drink per day for women and two for men. Fall-proof your home by removing tripping hazards and ensuring good lighting.
Diagnosis: How Osteoporosis is Detected
A DEXA scan (Dual-energy X-ray absorptiometry) is the gold standard test. It is a quick, painless scan that measures your Bone Mineral Density (BMD) at your hip and spine, giving you a "T-score" that compares your density to that of a healthy young adult.
Treatment Options: Slowing Loss and Building Strength
If diagnosed, treatment focuses on slowing bone loss and preventing fractures. This includes:
• Medications: Bisphosphonates are commonly prescribed. Other options include biologics, hormone-related therapy, and bone-building medications for severe cases.
• Nutritional Supplementation: High-dose calcium and vitamin D supplements are almost always recommended alongside prescription treatment.
• Physical Therapy: To improve strength, balance, and posture. It's crucial to work with a specialist to create a treatment plan. If you have risk factors or are concerned about bone loss, consult a doctor online with Apollo24|7 for an initial evaluation and guidance on next steps.
Conclusion
Understanding osteoporosis is the first step toward defeating it. This condition, driven by a complex mix of hormonal, nutritional, and lifestyle factors, has a profound and often devastating impact on bone health and overall well-being. However, it is not an inevitable part of ageing. By recognising the risk factors early, adopting bone-healthy habits, and seeking timely medical advice, you can take powerful control of your skeletal future. Protecting your bones is an investment in your mobility, independence, and quality of life for years to come. Start making deposits into your bone bank today.
More articles from Osteopetrosis
Frequently Asked Questions
What are the first signs of osteoporosis?
Unfortunately, there are often no early 'signs.' The first obvious indication is frequently a broken bone from a minor incident. Later signs can include back pain caused by a fractured vertebra, loss of height over time, or a stooped posture.
Can men get osteoporosis?
Absolutely. While more common in women, about 20-25% of osteoporosis-related fractures occur in men. Causes in men are often linked to low testosterone, excessive alcohol use, smoking, or long-term use of corticosteroids.
At what age should you start worrying about bone density?
Building peak bone mass happens until your late 20s. Prevention should start in childhood. Screening with a DEXA scan is generally recommended for all women at age 65 and men at age 70. However, if you have significant risk factors (like a family history or steroid use), your doctor may recommend screening earlier.
Is osteoporosis reversible?
While the condition itself is chronic, treatment can significantly slow down or even stop bone loss. Some medications can even help rebuild bone and increase density, effectively 'reversing' some of the damage, though not completely curing the disease.
Are there any natural treatments for osteoporosis?
'Natural' treatments are the foundation of prevention and management: a nutrient-dense diet, consistent weight-bearing exercise, adequate sun exposure for Vitamin D, and avoiding smoking and excess alcohol. These should always be done in conjunction with a doctor's advice, not as a replacement for prescribed medication if it is needed.

 (1).webp)