Understanding Osteoporosis: A Comprehensive Guide to Stronger Bones
Discover a complete guide to osteoporosis—causes, symptoms, diagnosis, treatment, and prevention strategies for stronger, healthier bones.

Written by Dr. Siri Nallapu
Reviewed by Dr. Shaik Abdul Kalam MD (Physician)
Last updated on 13th Jan, 2026

Introduction
Imagine your bones as the foundation of a house. Over time, if this foundation becomes porous and weak, the entire structure is at risk. Osteoporosis, which literally means "porous bone," is a condition that does exactly that—it silently weakens your bones, making them fragile and more likely to break. Often called a "silent disease" because it progresses without symptoms until a fracture occurs, understanding osteoporosis is your first and most powerful step towards prevention and management. This guide will demystify the condition, from its underlying causes and risk factors to the latest in diagnosis, treatment, and empowering lifestyle strategies. We’ll equip you with the knowledge to build and maintain strong, resilient bones for life, turning fear into actionable insight.
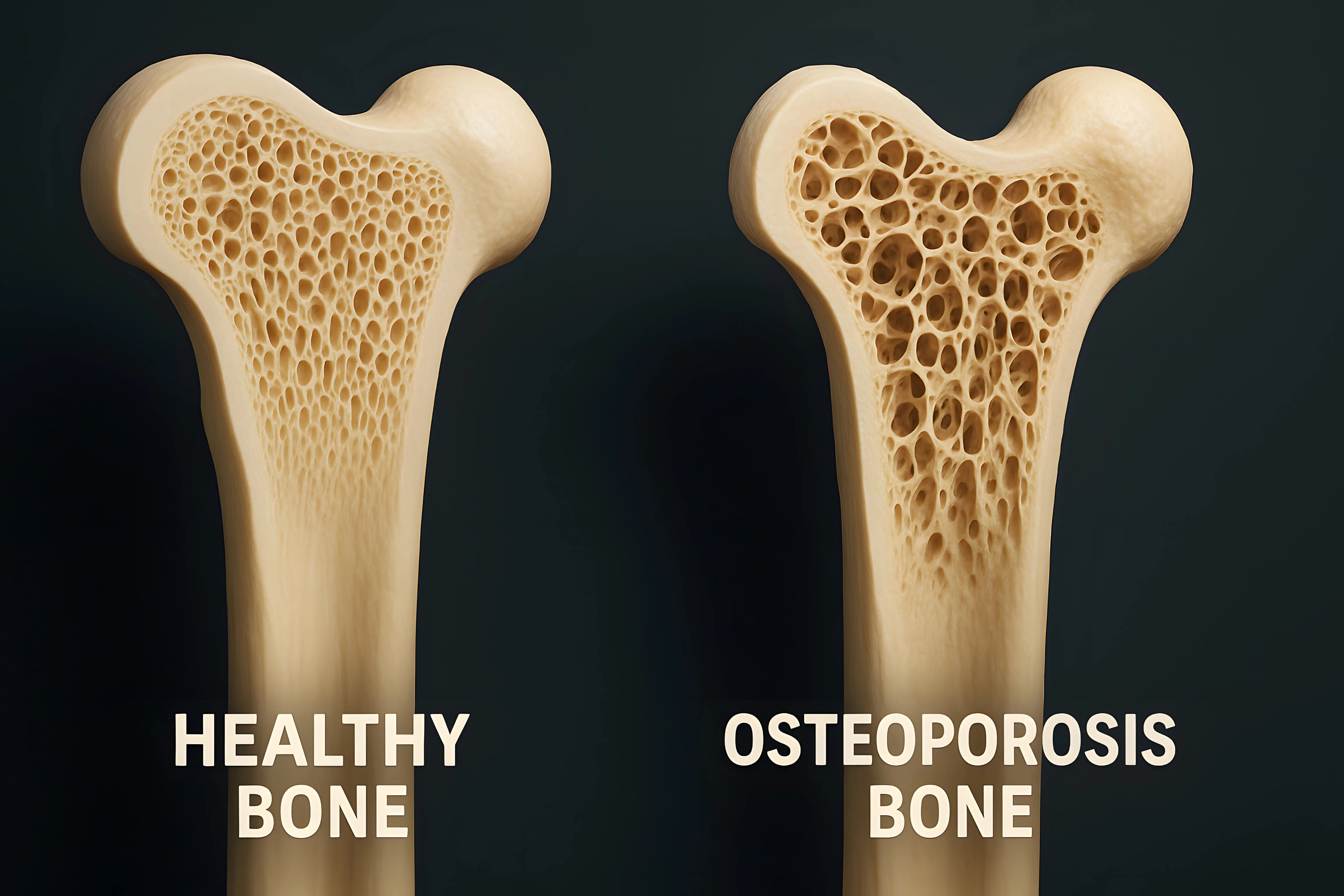
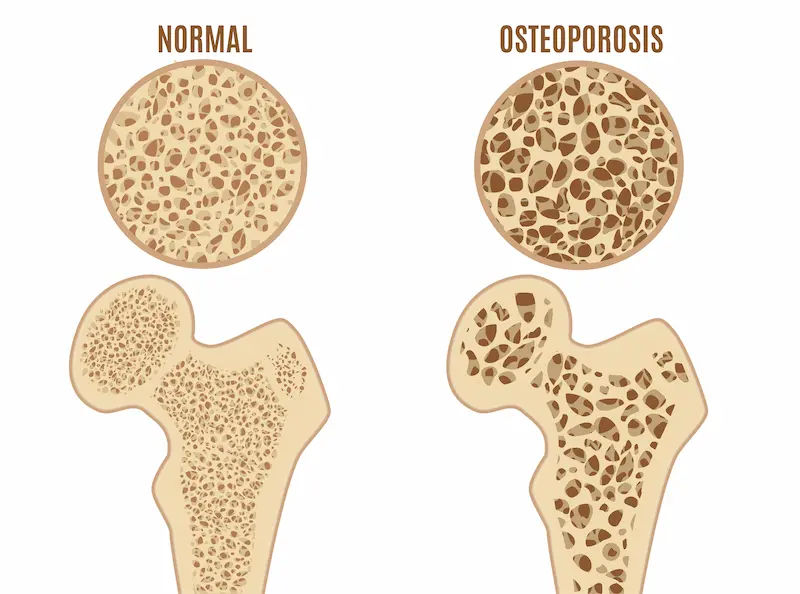
What is Osteoporosis? More Than Just Brittle Bones
Osteoporosis is a systemic skeletal disease characterised by low bone mass and deterioration of bone tissue. This leads to increased bone fragility and a consequent increase in fracture risk. Think of bone as a living tissue that is constantly being broken down and replaced. Up until around age 30, you build bone faster than you lose it. After that, this process reverses. Osteoporosis occurs when the creation of new bone doesn't keep up with the removal of old bone. It's not just about bones becoming "thin"; it's about the architecture of the bone becoming compromised. The honeycomb-like structure inside bones becomes larger, with holes and spaces much wider than in healthy bone, significantly reducing its density and quality.
The Silent Disease: Why Early Detection is Crucial
The most challenging aspect of osteoporosis is its stealthy nature. Unlike many other health conditions, there is often no pain or obvious warning sign as bone density decreases. Many people only discover they have osteoporosis after a minor fall or a sudden strain causes a broken bone, typically in the hip, wrist, or spine. A fracture from a simple action like bending over or coughing can be the first indicator. This is why proactive screening, especially for those with risk factors, is not just recommended—it is essential. Early detection through a bone density test can identify osteopenia (low bone mass, a precursor to osteoporosis) or osteoporosis itself, allowing for early intervention to strengthen bones and prevent devastating fractures.
Who is at Risk? Key Osteoporosis Risk Factors
Certain factors can increase your likelihood of developing osteoporosis. Some you cannot change, but many are within your control. Understanding your personal risk profile is a critical part of osteoporosis prevention.
Unchangeable Risk Factors
- Sex: Women are far more likely to develop osteoporosis than men, primarily due to the dramatic drop in oestrogen levels during menopause, which accelerates bone loss.
- Age: The risk increases for everyone as they get older.
- Family History: Having a parent or sibling with osteoporosis puts you at greater risk, especially if a parent had a hip fracture.
- Body Frame Size: Men and women with small body frames tend to have a higher risk because they might have less bone mass to draw from as they age.
- Race: Those of White or Asian descent are at highest risk.
Modifiable Risk Factors and Lifestyle Choices
- Sex Hormone Levels: Reduced oestrogen in women (e.g., during menopause) and low testosterone in men can contribute to bone loss.
- Dietary Factors: A lifelong lack of calcium intake and vitamin D deficiency play a major role. Vitamin D is crucial for calcium absorption.
- Medications: Long-term use of corticosteroid medications (e.g., prednisolone) is damaging to bone. Other drugs can also increase risk.
- Lifestyle: A sedentary lifestyle, excessive alcohol consumption, and tobacco use are significant contributors to weak bones.
How Do You Know? Recognising Osteoporosis Symptoms
As mentioned, there are typically no symptoms in the early stages. However, once bones have been weakened by the disease, you might notice signs that indicate it is time to speak to a doctor.
The First Signs Are Often Fractures
The most common clinical manifestation is a fragility fracture—a break that occurs from a fall from standing height or less, or even without any trauma. The most serious are hip fractures, which often require surgery and can lead to a loss of independence. Spinal fractures (vertebral compression fractures) are also very common.
Consult a Specialist for Personalised Advice
Beyond Fractures: Posture Changes and Pain
When osteoporosis affects the vertebrae in the spine, it can lead to:
- Back pain, caused by a fractured or collapsed vertebra.
- Loss of height over time.
- A stooped posture (kyphosis), sometimes called a "dowager's hump."
If you notice any of these changes, especially if you have other risk factors, it is important to consult a doctor online with Apollo24|7 for further evaluation. They can assess your symptoms and recommend the next steps, which likely include a diagnostic scan.
Getting a Diagnosis: The Bone Density Test and Beyond
If you are at risk, your doctor will likely recommend a diagnostic test. Do not wait for a fracture to be your first test.
The Gold Standard: The DEXA Scan (T-Score Explained)
A Dual-Energy X-ray Absorptiometry (DEXA/DXA) scan is the most common and accurate test to measure bone mineral density. It is painless, non-invasive, and uses low levels of X-rays. Your results are given as a T-score:
- Normal: T-score of -1.0 and above.
- Osteopenia (Low bone mass): T-score between -1.0 and -2.5.
- Osteoporosis: T-score of -2.5 or below.
Other Diagnostic Tools: FRAX Assessment and Lab Tests
Your doctor may also use the FRAX tool, which uses your bone density and other risk factors to estimate your 10-year probability of having a major fracture. Additionally, blood and urine tests can help identify underlying conditions that cause bone loss (e.g., thyroid problems, vitamin D deficiency). Apollo24|7 offers convenient home collection for tests like vitamin D or calcium levels, making this diagnostic process easier.
Building Your Defence: Osteoporosis Treatment Options
A diagnosis of osteoporosis is not a verdict; it is a call to action. Osteoporosis treatment aims to slow or stop bone loss, prevent fractures, and manage pain.
Common Osteoporosis Medications and How They Work
- Bisphosphonates (e.g., alendronate, risedronate): These are the most commonly prescribed drugs. They slow the rate of bone breakdown.
- Monoclonal Antibodies (e.g., Denosumab): Given by injection every six months, it reduces bone breakdown.
- Bone-Building Medications (e.g., Teriparatide, Abaloparatide): These are synthetic versions of parathyroid hormone and stimulate new bone growth. They are used for those at very high risk of fracture.
- Hormone-Related Therapy: Raloxifene mimics oestrogen's beneficial effects on bone density without some of the risks.
The Role of Hormone Therapy
Oestrogen therapy, particularly when started soon after menopause, can help maintain bone density. However, because it can also increase the risk of blood clots, heart disease, and certain cancers, it is typically used for bone health only if a woman is also seeking treatment for menopausal symptoms. The decision is highly individual and must be made with a doctor.
Prevention is Power: How to Prevent Osteoporosis Naturally
The best treatment is always prevention. Building strong bones during your youth and maintaining bone health as you age can dramatically reduce your risk.
Nutrition for Bone Health: Calcium and Vitamin D
These two nutrients are the building blocks and the delivery system for your bones.
- Calcium: Adults need 1,000-1,200 mg per day. Excellent sources include dairy products, dark leafy greens, sardines, and fortified foods.
- Vitamin D: Adults need 600-800 IU per day. Your skin makes it from sunlight, but it can be hard to get enough. Fatty fish, egg yolks, and fortified milk are good sources. Supplements are often necessary.
The Best Exercises for Bone Density
Bone is living tissue that gets stronger when stressed. The right exercises for osteoporosis are crucial.
Weight-Bearing Exercises
These force you to work against gravity. Examples include brisk walking, jogging, dancing, and stair climbing.
Muscle-Strengthening Exercises
Lifting weights or using resistance bands puts stress on your bones, stimulating them to get stronger. Focus on major muscle groups.
Balance and Posture Exercises
Tai chi, yoga, and simple balance exercises (e.g., standing on one leg) are critical for fall prevention, which is the ultimate goal of managing osteoporosis.
Living Well with Osteoporosis: Daily Management and Safety
A diagnosis means adapting your lifestyle to protect your bones without giving up the activities you love.
Fall-Proofing Your Home Environment
Remove tripping hazards like loose rugs and electrical cords. Install grab bars in the shower and near the toilet. Ensure your home is well-lit.
Pain Management and Mental Wellbeing
Chronic pain from fractures can affect your mental health. Physiotherapy, pain management strategies, and seeking support from friends, family, or a therapist are all important parts of a holistic treatment plan. If your condition does not improve after trying these methods, book a physical visit to a doctor with Apollo24|7 to create a comprehensive pain management plan.
Conclusion: Your Journey to Lifelong Bone Health
Understanding osteoporosis is the foundation upon which you can build a future of strength and mobility. While the diagnosis can feel daunting, it is important to remember that you have significant power to influence the health of your bones. From the food you eat and the activities you choose to the proactive decisions you make with your doctor, every action counts. This is not about fear; it is about empowerment. By embracing a bone-healthy lifestyle, adhering to treatment plans, and making your environment safe, you can significantly reduce your risk of fracture and maintain your independence and quality of life for years to come. Start today—your future self will thank you for the strong foundation you build.
Consult a Specialist for Personalised Advice
Consult a Specialist for Personalised Advice

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr Syed Mateen Pasha
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Syed Ismail Ali
General Practitioner
7 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr. Debajyoti Goswami
Obstetrician and Gynaecologist
10 Years • MBBS,D.G.O(DNB),Adv. Infertility Tech.(AIIMS),Fellowship in Diabetes(U.K),Comprehensive Abortion Care(Govt. Of W.B), Certificate in Clinical Embryology(AIIMS, BHUBANESWAR)
Bankura
D.G Clinic, Bankura
(25+ Patients)
Consult a Specialist for Personalised Advice

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr Syed Mateen Pasha
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Syed Ismail Ali
General Practitioner
7 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr. Debajyoti Goswami
Obstetrician and Gynaecologist
10 Years • MBBS,D.G.O(DNB),Adv. Infertility Tech.(AIIMS),Fellowship in Diabetes(U.K),Comprehensive Abortion Care(Govt. Of W.B), Certificate in Clinical Embryology(AIIMS, BHUBANESWAR)
Bankura
D.G Clinic, Bankura
(25+ Patients)
More articles from Osteopetrosis
Frequently Asked Questions
What is the difference between osteopenia and osteoporosis?
Osteopenia is a precursor to osteoporosis. It means your bone density is lower than normal but not yet low enough to be classified as osteoporosis. It's a warning sign to take action with lifestyle changes to prevent progression.
Can men get osteoporosis?
Absolutely. While it is more common in women, about 20-25% of osteoporotic fractures occur in men. Risk factors for men include low testosterone, excessive alcohol use, certain medications, and underlying medical conditions.
Are there any natural remedies for osteoporosis?
While no 'remedy' can replace prescribed medication if needed, natural approaches are foundational. This includes ensuring adequate calcium intake and vitamin D, performing regular weight-bearing exercises, and avoiding smoking and excessive alcohol. Always discuss supplements with your doctor.
At what age should I get a bone density test?
The National Osteoporosis Foundation recommends a DEXA scan for all women age 65 and older and all men age 70 and older. However, if you have significant risk factors (e.g., a previous fracture, use of steroids, family history), your doctor may recommend screening sooner.
Can you rebuild bone density after a diagnosis?
Yes, to an extent. While it is difficult to completely reverse osteoporosis, treatment with bone-building medications can significantly increase density. For most people, the goal of treatment is to slow or stop bone loss, which effectively strengthens bones and prevents fractures.

 (1).webp)