Guide to Are You Suffering From Weak Bones
Learn the signs, causes, and steps you can take if you suspect you have weak bones or are at risk for osteoporosis. A complete guide to bone health, diagnosis, and treatment.


Introduction
Do you often dismiss that nagging backache as just a sign of aging? Or perhaps you’ve noticed a slight loss in height over the years? While these might seem like minor inconveniences, they could be your body’s way of signaling a deeper issue: weakening bones. Often a "silent" condition with no obvious symptoms until a fracture occurs, weak bones affect millions worldwide, leading to pain, reduced mobility, and a loss of independence. This guide is designed to demystify bone health, moving beyond the basics of "take calcium" to give you a clear, actionable understanding of what weak bones mean, how to spot the early signs, and most importantly, how to build and maintain strong, resilient bones for life. We’ll explore the critical difference between osteopenia and osteoporosis, uncover the often-missed risk factors, and outline a proactive plan for prevention and management. If you’ve ever wondered whether your bones are as strong as they should be, you’re in the right place.
What Are Weak Bones, Really? Understanding Bone Density
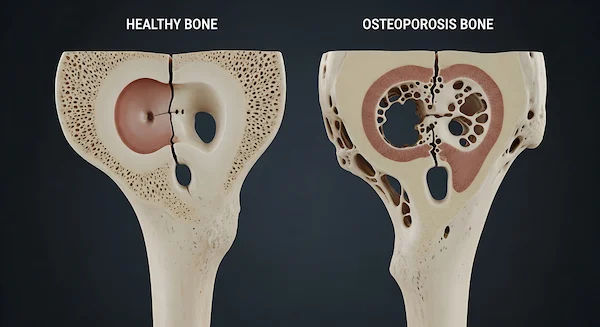
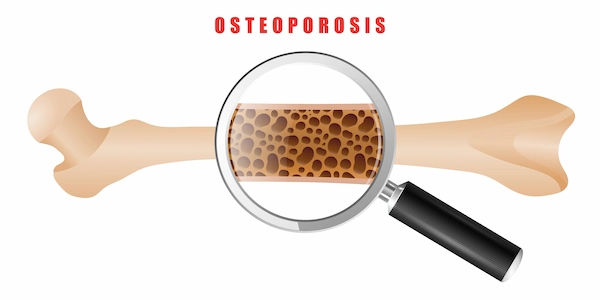
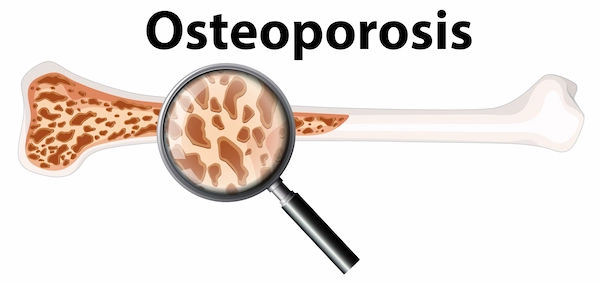
At its core, having weak bones means your bone mineral density (BMD) is lower than normal. Think of bone density as the measure of how tightly packed the minerals, primarily calcium and phosphate, are within your bone structure. Strong bones are dense and can withstand stress, while weak bones are porous, fragile, and more susceptible to fractures, even from minor bumps or falls.
The Bone Remodeling Process: A Constant Cycle (H3)
Your bones are not static; they are living tissues constantly undergoing a process called remodeling. Special cells called osteoclasts break down old bone (resorption), while cells called osteoblasts build new bone (formation). In your youth, bone formation outpaces resorption, leading to peak bone mass around age 30. After that, the balance slowly shifts, and you naturally begin to lose a small amount of bone density each year. The problem of weak bones arises when this breakdown process accelerates or new bone formation slows down too much, leading to a net loss.
Osteopenia vs. Osteoporosis: Knowing the Difference (H3)
These two terms describe stages of bone loss:
• Osteopenia: This is the middle ground between healthy bones and osteoporosis. It means your bone density is lower than average for your age but not yet severe enough to be classified as osteoporosis. It’s a warning sign that you need to take action to prevent further loss.
• Osteoporosis: This is the more advanced stage, where bones have become significantly porous ("brittle bones"), dramatically increasing fracture risk. A diagnosis of osteoporosis means the structural integrity of your bones is compromised.
Consult Top Specialists
Are You at Risk? Key Risk Factors for Weak Bones
Understanding your personal risk is the first step toward prevention. These factors are divided into those you can't change and those you can influence.
Non-Modifiable Risk Factors (You Can't Change)
• Age and Gender: Bone loss accelerates after menopause in women due to dropping estrogen levels. Women over 50 are at the highest risk. Men also experience age-related bone loss but typically later in life.
• Family History: A parent or sibling with osteoporosis or a hip fracture increases your risk.
• Body Frame Size: Men and women with small body frames tend to have a higher risk because they may have less bone mass to draw from as they age.
• Ethnicity: Those of Caucasian or Asian descent are at higher risk.
Modifiable Risk Factors (You Can Influence)
ietary Deficiencies: Chronically low intake of calcium and vitamin D is a primary culprit. Vitamin D is crucial for calcium absorption.
• Sedentary Lifestyle: Bones get stronger in response to weight-bearing and muscle-strengthening exercises. A lack of activity leads to faster bone loss.
• Smoking and Excessive Alcohol: Tobacco use interferes with the body's ability to use calcium. Consuming more than two alcoholic drinks a day can damage bone-forming cells.
• Certain Medications: Long-term use of corticosteroids (like prednisone), some anticonvulsants, and certain cancer treatments can contribute to bone loss.
• Other Medical Conditions: Conditions like celiac disease, inflammatory bowel disease, kidney or liver disease, and hyperthyroidism can affect nutrient absorption and bone health.
Silent but Not Invisible: Recognizing the Symptoms of Weak Bones
Osteoporosis is often called a "silent disease" because bone loss itself has no symptoms. However, there are signs that can point toward weakening bones.
Early Warning Signs Often Missed
• Receding Gums: Your jawbone supports your teeth. If it's losing density, gums can recede.
• Weakened Grip Strength: Studies have linked poorer handgrip strength to lower bone mineral density.
• Brittle Fingernails: While not a definitive diagnostic tool, consistently weak and brittle nails can sometimes indicate nutritional deficiencies affecting bone health.
Signs of Advanced Bone Loss
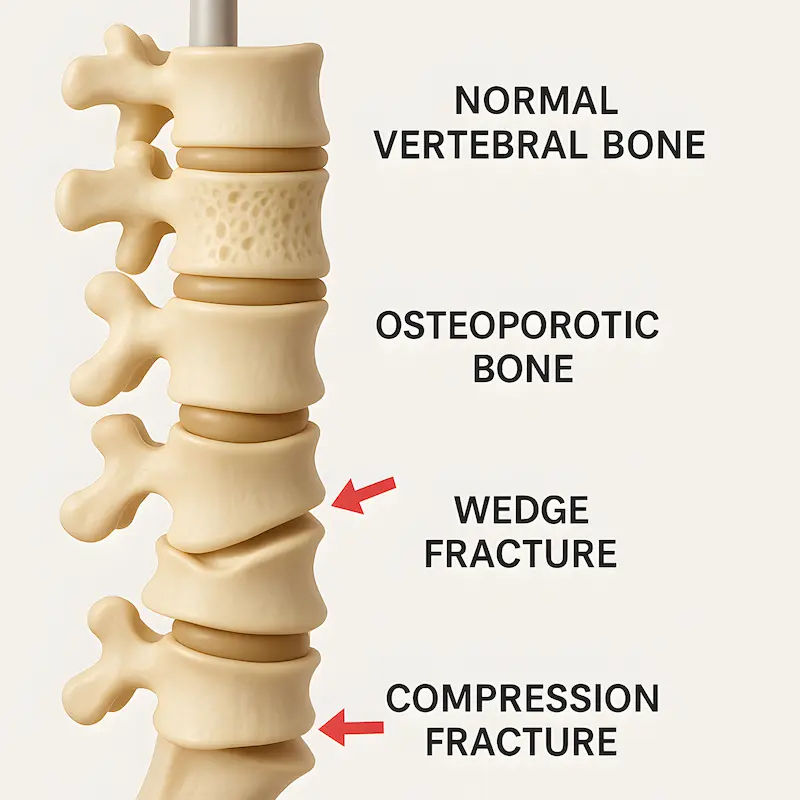
• Loss of Height: Compression fractures in the spine can cause a noticeable loss of height over time.
• A Stooped Posture (Kyphosis): Also caused by spinal fractures, leading to a curved upper back.
• Back or Neck Pain: Sudden, severe pain can signal a collapsed or fractured vertebra.
• A Fracture from a Minor Fall: This is the most common and serious sign. A fracture from a standing height or less is often a major indicator of osteoporosis.
How Are Weak Bones Diagnosed? Getting the Right Tests
If you identify with several risk factors or notice potential symptoms, it’s important to get evaluated.
The Gold Standard: The DEXA Scan (Hone Density Test)
A Dual-Energy X-ray Absorptiometry (DEXA or DXA) scan is a quick, painless, low-radiation test that measures your bone density at the hip and spine. The result is a T-score that compares your density to that of a healthy young adult.
• Normal: T-score of -1.0 or above
• Osteopenia: T-score between -1.0 and -2.5
• Osteoporosis: T-score of -2.5 or below
Other Diagnostic Tools and Blood Tests
Your doctor might order blood tests to rule out other conditions that cause bone loss, such as checking your Vitamin D levels, calcium, thyroid function, and testosterone (in men). If your condition is complex, a doctor can interpret these results and recommend a tailored plan. Apollo24|7 offers convenient home collection for tests like vitamin D or calcium levels, making initial screening easier.
Building Stronger Bones: Your Action Plan for Prevention and Management
Whether you’re preventing bone loss or managing osteopenia/osteoporosis, the principles are similar: nutrition, exercise, and lifestyle.
Nutrition for Bone Health: Beyond Calcium and Vitamin D
• Calcium: Aim for 1,000-1,200 mg daily from dietary sources like dairy, leafy greens, fortified foods, sardines, and almonds.
• Vitamin D: Get 15-20 minutes of sunlight several times a week and consume fatty fish, egg yolks, and fortified milk. Supplementation is often necessary, especially for those with a vitamin D deficiency.
• Other Key Nutrients: Protein, Magnesium, Vitamin K, and Potassium all play supporting roles in bone health. A balanced diet rich in fruits, vegetables, and lean proteins is essential.
The Best Exercises to Strengthen Your Bones
Bones respond to stress by becoming stronger. Focus on:
• Weight-Bearing Exercises: Activities where you work against gravity. This includes brisk walking, jogging, dancing, and stair climbing.
• Muscle-Strengthening Exercises: Using free weights, resistance bands, or your own body weight (e.g., squats, push-ups) places stress on the bones, stimulating growth.
Lifestyle Changes for Optimal Bone Density
• Quit Smoking: This is one of the most significant steps you can take.
• Limit Alcohol: Stick to moderate consumption (one drink per day for women, two for men).
• Fall Prevention: Make your home safer by removing tripping hazards, using non-slip mats, and ensuring good lighting.
When to Seek Professional Help?
If you have multiple risk factors, are over 50 and have experienced a fracture, or are concerned about your bone density loss, don't wait. If you are experiencing persistent back pain or have noticed a change in your posture, consulting a doctor online with Apollo24|7 can be a great first step for evaluation and guidance. They can advise if an in-person visit or a DEXA scan is necessary.
Conclusion
Weak bones don't have to be an inevitable part of aging. By understanding the risk factors and recognizing the subtle signs, you can take proactive control of your skeletal health. The journey to stronger bones is built on a foundation of consistent, healthy habits: a nutrient-rich diet, regular weight-bearing exercise, and smart lifestyle choices. Remember, it's never too early or too late to start. Whether you're in your 30s aiming to build peak bone mass or in your 60s working to preserve what you have, every positive change counts. If you're unsure where you stand, take that first step and speak to a healthcare professional. Your future, mobile, and independent self will thank you.
Consult Top Specialists
Consult Top Specialists

Dr. B Rachana
General Physician/ Internal Medicine Specialist
8 Years • MBBS, Fellowship in Diabetes, Fellowship in Applied Nutrition,CCEBDM(Diabetes)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Ashok M L
General Physician/ Internal Medicine Specialist
24 Years • MD Med.
Bengaluru
Apollo Hospitals Jayanagar, Bengaluru
(75+ Patients)

Dr. Chethan T L
General Physician/ Internal Medicine Specialist
5 Years • MBBS, MD, DNB (General Medicine)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Lakshmi Sanjitha Kakani
General Physician/ Internal Medicine Specialist
6 Years • MBBS, MD (General Medicine)
Visakhapatnam
Apollo 24|7 Clinic - Andhra Pradesh, Visakhapatnam

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
26 Years • MBBS
Kolkata
B Ghose Foundation Doctor's Chamber, Kolkata
(50+ Patients)
Consult Top Specialists

Dr. B Rachana
General Physician/ Internal Medicine Specialist
8 Years • MBBS, Fellowship in Diabetes, Fellowship in Applied Nutrition,CCEBDM(Diabetes)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Ashok M L
General Physician/ Internal Medicine Specialist
24 Years • MD Med.
Bengaluru
Apollo Hospitals Jayanagar, Bengaluru
(75+ Patients)

Dr. Chethan T L
General Physician/ Internal Medicine Specialist
5 Years • MBBS, MD, DNB (General Medicine)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Lakshmi Sanjitha Kakani
General Physician/ Internal Medicine Specialist
6 Years • MBBS, MD (General Medicine)
Visakhapatnam
Apollo 24|7 Clinic - Andhra Pradesh, Visakhapatnam

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
26 Years • MBBS
Kolkata
B Ghose Foundation Doctor's Chamber, Kolkata
(50+ Patients)
More articles from Osteoporosis
Frequently Asked Questions
1. Can young people get weak bones?
Yes. While more common in older adults, young people can develop weak bones due to factors like eating disorders, certain medical conditions, long-term use of corticosteroid medications, or extreme nutritional deficiencies.
2. What are the best calcium-rich foods for someone who is lactose intolerant?
Excellent non-dairy sources of calcium include fortified plant-based milks and juices, leafy green vegetables (kale, bok choy), canned sardines and salmon (with bones), tofu, almonds, and beans.
3. Are there any specific symptoms of weak bones in the legs?
There are usually no direct symptoms in the legs until a fracture occurs. However, general weakness, muscle aches, or pain when standing or walking could be indirect signs, but these are non-specific and should be evaluated by a doctor to rule out other causes.
4. How often should I get a bone density test?
For most women, screening is recommended starting at age 65, and for men at 70. However, if you have significant risk factors (like a previous fracture or steroid use), your doctor may recommend earlier and more frequent testing, typically every 2 years.
5. Can you rebuild bone density after it's lost?
While it's challenging to completely reverse osteoporosis, you can significantly slow bone loss and even achieve modest improvements in bone density through a combination of prescribed medications, intense exercise, and optimal nutrition. The primary goal is to prevent fractures.