Osteoporosis and Bone Health: Causes, Risks, and Proactive Steps
Know about the osteoporosis, what it is, causes, risk factors, diagnosis, treatment options and prevention.

Written by Dr. Shaik Abdul Kalam
Reviewed by Dr. Dhankecha Mayank Dineshbhai MBBS
Last updated on 13th Jan, 2026
Introduction
Imagine your bones as the steel framework of a building. Over time, if that framework weakens, the entire structure becomes fragile. Osteoporosis is a condition that does exactly that to your skeleton, silently leaching minerals and strength from your bones, making them porous, brittle, and highly susceptible to fractures. Often called a "silent disease" because it progresses without symptoms until a bone breaks, understanding what leads to osteoporosis and its profound impact on overall bone health is the first step toward prevention and maintaining a strong, active life. This article will demystify the causes, from factors beyond your control to the lifestyle choices that play a crucial role.
What is Osteoporosis? The Silent Thief of Bone
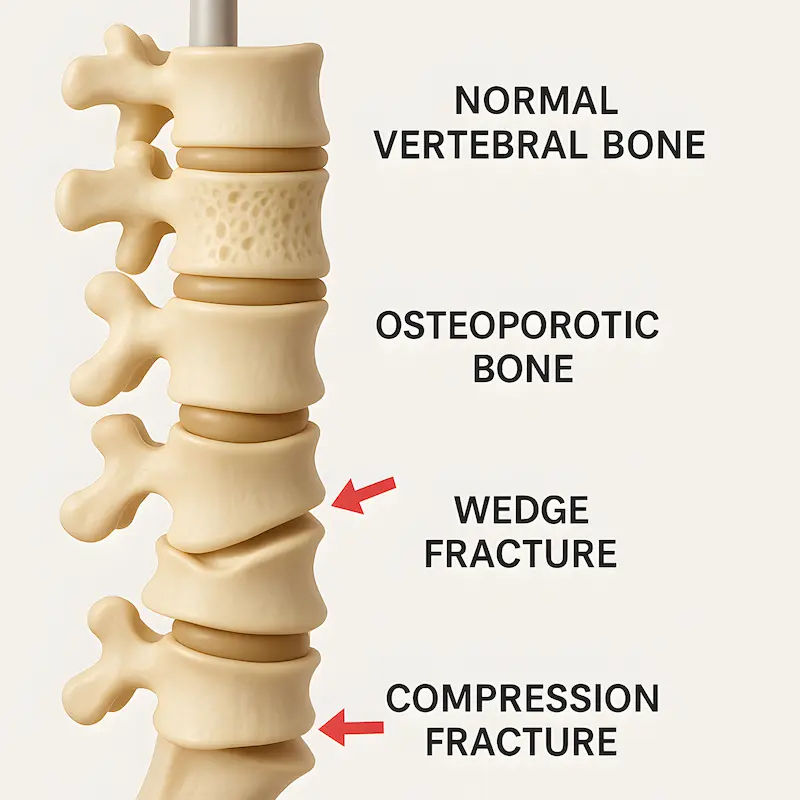
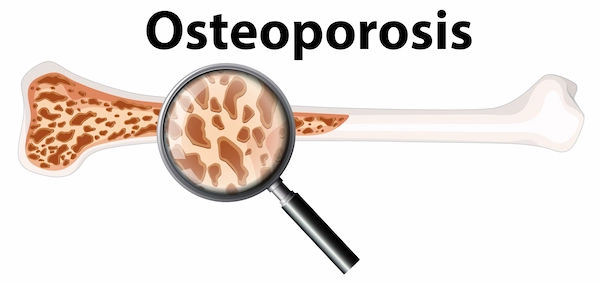
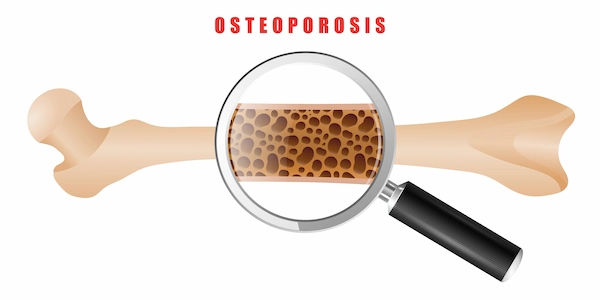
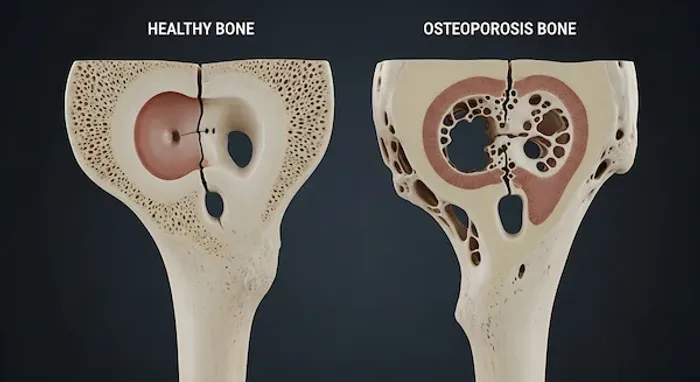
At its core, osteoporosis is a disease characterised by low bone mass and deterioration of bone tissue. To understand it, think of your bones as living tissue that is constantly being broken down and rebuilt in a process called remodelling. Up until around age 30, you build bone faster than you lose it, reaching your peak bone mass. After that, the balance can shift, and breakdown slowly overtakes formation. In osteoporosis, this process becomes unbalanced, leading to excessive bone loss. The internal structure of the bone becomes honeycombed with larger holes, weakening its architecture. This is why a simple stumble, a minor bump, or even a sneeze can cause a fracture in someone with advanced osteoporosis. The impact is not just on the skeleton; it's a whole-body health issue that compromises mobility, independence, and quality of life.
Consult a Top Bone Specialist for Personalised Advice
The Primary Causes: Why Bones Lose Their Strength
The development of osteoporosis is rarely due to a single cause. It's typically a combination of factors that accumulate over a lifetime. We can divide these into two main categories: those you cannot change and those you can.
The Non-Modifiable Risk Factors You Can't Change
Certain risk factors are inherent and serve as important indicators for your personal level of vigilance.
Age: The Inevitable Factor
Age is the most significant risk factor. After peak bone mass is achieved, everyone experiences a gradual decline. For women, this loss accelerates significantly for about 5-10 years after menopause due to dropping estrogen levels.
Gender and Hormones: Why Women Are at Higher Risk
Women are four times more likely to develop osteoporosis than men. This is primarily because women have smaller, less dense bones to begin with and experience a sharp decline in estrogen at menopause, a hormone crucial for bone protection. In men, lower testosterone levels can also contribute, but the decline is more gradual.
Family History and Genetics
If a parent or sibling has had osteoporosis or a fragility fracture (especially a hip fracture), your risk is higher. Your genetic blueprint influences your peak bone mass and how quickly you lose it.
Modifiable Risk Factors: Where You Can Take Control
This is the area where you have the most power to influence your bone health trajectory.
Nutritional Deficiencies: The Calcium and Vitamin D Gap
Calcium is the primary mineral that makes bones hard. Vitamin D is essential for your body to absorb calcium. A long-term deficiency in either is a direct pathway to weakened bones. Many adults do not get the recommended daily amounts, making calcium-rich foods for bones and sensible sun exposure or supplementation critical.
Sedentary Lifestyle: Use It or Lose It
Bones are living tissue that respond to stress by becoming stronger. A sedentary lifestyle fails to provide the stimulus needed for bone maintenance. Weight-bearing and muscle-strengthening exercises are non-negotiable for how to increase bone density naturally.
Smoking and Excessive Alcohol Consumption
Tobacco use is terrible for bones. It reduces blood supply to the bones, slows the production of bone-forming cells, and impairs calcium absorption. Similarly, consuming more than two alcoholic drinks per day can interfere with the body's ability to absorb calcium and vitamin D.
The Domino Effect: How Osteoporosis Impacts Your Body and Life
The impact of osteoporosis extends far beyond a simple diagnosis. It triggers a domino effect that can profoundly alter a person's life.
Fractures: The Most Direct and Devastating Consequence
Fractures are the most common and serious complication. The most frequent sites are the hip, spine (vertebrae), and wrist. A hip fracture often requires surgery and can lead to a loss of independence and increased risk of mortality. Spinal fractures can occur without a fall, simply from the pressure of gravity.
Loss of Height and the Dowager's Hump (Kyphosis)
Multiple fractures in the spine can cause the vertebrae to collapse. This leads to a gradual loss of height and a curvature of the upper back, known as kyphosis or a "dowager's hump." This can cause chronic back pain and compress the lungs and abdomen, affecting breathing and digestion.
Chronic Pain and Reduced Mobility
The pain from fractures and altered posture can be debilitating. Fear of falling and causing another fracture can lead to anxiety and a self-imposed reduction in activity. This creates a vicious cycle: less activity leads to further bone loss and muscle weakness, increasing the risk of falls.
The Psychological Impact: Anxiety and Loss of Independence
The constant worry about fractures and the physical limitations can lead to depression, social isolation, and a loss of self-esteem. The feeling of losing independence is one of the most significant psychological burdens for individuals with this condition.
Diagnosis: How Osteoporosis is Detected
Because osteoporosis is silent, diagnosis often comes after a fracture or through screening. If you have significant risk factors, it's wise to discuss screening with your doctor.
The Gold Standard: The DXA Bone Density Scan
The most common test is a DXA (Dual-Energy X-ray Absorptiometry) scan. It's a quick, painless scan that measures bone mineral density (BMD) at the hip and spine. The results are given as a T-score, which compares your BMD to that of a healthy young adult. A T-score of -2.5 or lower indicates osteoporosis.
If you have risk factors like early menopause or a family history of hip fractures, consulting a doctor online with Apollo24|7 can help you determine if a DXA scan is right for you.
Building Strong Bones: Prevention and Management Strategies
The good news is that osteoporosis is largely preventable and manageable. The strategies for prevention are also the cornerstone of treatment.
The Bone-Building Diet: More Than Just Calcium
Aim for 1,000-1,200 mg of calcium daily from dietary sources like dairy products, leafy greens, fortified foods, and sardines. Pair this with adequate Vitamin D (600-800 IU for most adults) from sunlight, fatty fish, eggs, and supplements if needed. Apollo24|7 offers convenient home collection for tests like vitamin D levels to check if you are deficient.
The Best Exercises for Bone Density
Weight-bearing exercises (where you work against gravity) are key. This includes walking, jogging, dancing, and tennis. Muscle-strengthening exercises using weights or resistance bands are equally important, as they put stress on the bones they are attached to. Balance exercises like Tai Chi can also help prevent falls.
Medications and When They Are Necessary
When bone loss is significant or a fracture has occurred, doctors may prescribe medications. These include bisphosphonates (which slow bone breakdown), hormone-related therapy, and anabolic agents (which build bone). If your condition does not improve after trying these lifestyle methods, book a physical visit to a doctor with Apollo24|7 to discuss a comprehensive treatment plan tailored to your needs.
Conclusion
Understanding what leads to osteoporosis and its impact on bone health empowers you to take charge of your skeletal strength. While some risk factors are beyond your control, the most powerful levers nutrition, exercise, and lifestyle habits—are firmly in your hands. The journey to strong bones is a marathon, not a sprint. It requires consistent, daily choices that nourish and challenge your skeleton. By prioritising a bone-healthy lifestyle today, you are investing in a future of mobility, independence, and vitality. Start building your foundation for lifelong bone health now. If you have concerns about your personal risk, take the proactive step of speaking with a healthcare professional to create a plan that works for you.
Consult a Top Bone Specialist for Personalised Advice
Consult a Top Bone Specialist for Personalised Advice

Dr. Mohammed Tanzeem P
Orthopaedician
5 Years • MBBS, MS Orthopaedics
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Vishruta A V
Orthopaedician
5 Years • MBBS MS Orthopaedics
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Sushruth J
Orthopaedician
5 Years • MBBS, MS (ORTHOPEDICS),Fellowship in Arthroplasty,FRGUHS – Spine surgery,FIFA Diploma in Football Medicine
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Rupam Chowdhury
Orthopaedician
10 Years • MBBS, DNB (Ortho.)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr. Sudipta Saha
Orthopaedician
8 Years • MBBS,(D. Ortho)
Kolkata
VDC Clinic, Kolkata
More articles from Osteoporosis
Frequently Asked Questions
1. What are the early signs of osteoporosis?
Unfortunately, there are often no early symptoms, which is why it's called a silent disease. The first sign is frequently a fracture from a minor incident. Later signs can include back pain, loss of height, and a stooped posture.
2. Can you reverse osteoporosis?
While you may not fully 'reverse' it to the bone density of a 30-year-old, you can significantly improve bone strength and density through a combination of medication (if prescribed), a high-calcium and vitamin D diet, and specific weight-bearing exercises. The goal is to stop bone loss and stimulate new bone formation.
3. What is the difference between osteopenia and osteoporosis?
Osteopenia is a precursor to osteoporosis. It means your bone density is lower than normal but not yet low enough to be classified as osteoporosis. It's a warning sign that you should take proactive steps to prevent further loss.
4. Are men at risk for osteoporosis?
Yes. While it's more common in women, about 1 in 4 men over 50 will break a bone due to osteoporosis. Men often have larger, denser bones to start with and don't experience the rapid hormonal shift that women do at menopause, but age-related bone loss still occurs.
5. What are the best weight-bearing exercises for bone health?
Activities that make you work against gravity are excellent. This includes brisk walking, hiking, jogging, climbing stairs, dancing, and playing tennis. Strength training with free weights, resistance bands, or weight machines is also highly effective.